Abstract
Background and Purpose
The requirement for neurology liaison is increasing in accordance with the growing health care demands associated with aging populations. The aim of this study was to characterize the nature of neurological inpatient liaisons (NILs) to help plan for the appropriate use of neurology resources.
Methods
This was a retrospective cross-sectional study of NILs in a secondary referral hospital over a 12-month period.
Results
There were 853 neurological consultations with a liaison rate of 3% per admission case. Chest medicine, gastroenterology, and infectious disease were the three most frequent specialties requesting liaison, and altered consciousness, seizure, and stroke were the three most frequent disorders for which a NIL was requested. Infection was the most common cause of altered consciousness. Epilepsy, infection, and previous stroke were common causes of seizure disorders. Acute stroke accounted for 44% of all stroke disorders. Electroencephalography was the most recommended study, and was also the most frequently performed. Ninety-five percent of emergency consultations were completed within 2 hours, and 85% of regular consultations were completed within 24 hours. The consult-to-visit times for emergency and regular consultations were 44±47 minutes (mean±standard deviation) and 730±768 minutes, respectively, and were shorter for regular consultations at intensive care units (p=0.0151) and for seizure and stroke disorders (p=0.0032).
Conclusions
Altered consciousness, seizure, and stroke were the most common reasons for NILs. Half of the patients had acute neurological diseases warranting immediate diagnosis and treatment by the consulting neurologists. Balancing increasing neurologist workloads and appropriate health-care resources remains a challenge.
Taiwan has one of the fastest aging populations in the world, with 11.3% of the general population being over 65 years of age.1 At the current growth rate, that percentage is expected to exceed 14% by 2017. The aging population of those aged 80 years and older is also expanding proportionally. Consequently, the health-care system is challenged by the growing service demand and complex comorbidities of the expanding geriatric population. The prevalence of chronic illnesses among the elderly population reached 65.2% according to the Foundation for Chinese Labor-Management Affairs.2 Neurological problems are frequently encountered during admission, accounting for 15-20% of all admissions to medical wards.3 One-third of patients admitted into intensive care units (ICUs) have a neurological complication detrimental to their outcome, which can double the length of the hospital stay and the likelihood of death.4 However, nonneurologists care for most patients with neurological diseases,5 and so neurological inpatient liaisons (NILs) are frequently requested for the further diagnosis and management of these patients.67 This requirement and its clinical relevance to NILs have grown in the past few years. NIL consultations halve the length of hospital stays for patients with acute neurological emergencies and result in more accurate diagnoses, with obvious clinical and financial advantages to the patients with acute neurological disorders.48 Understanding the characteristics of NIL facilitates the delivery of rapid and appropriate responses. The current study describes the impact of NILs on inpatient care.
All NIL consultations were collected retrospectively from a computer-based consultation system during a 12-month period (July 1, 2012 to June 30, 2013) in a secondary referral hospital in New Taipei City, Taiwan. The hospital is a 995-bed general hospital with 256 visiting staff that serves approximately 2,700 inpatients and 80,000 outpatients per month. In the neurological department, the responsibility for NILs is assigned to eight consultant neurologists according to a regular schedule. When a neurological regular consultation is requested by a physician from another department through the computer-based consultation system, the system automatically sends an assignment and notification of the consultation to the neurologist on rotation. The time from the consultation request to the neurologist visiting the patient (consultto-visit time) is recommended to be within 2 hours (120 minutes) for an emergency consultation and within 24 hours (1,440 minutes) for a regular consultation. Detailed information about each NIL and its corresponding responses were retrieved from the hospital consultation system. All of the imaging studies were reviewed in the picture archiving and communication system of the hospital. Other information was obtained by reviewing medical charts and the neurological laboratory database. Altered consciousness, including coma, stupor, obtundity, delirium, confusion, and drowsiness, was categorized based on the consultation request form. All symptoms regarding suspicion of stroke were categorized as stroke disorder. Neuromuscular disorders included symptoms of radiculopathy, neuropathy, myofascial pain, and nonspecific pain syndrome. Unexplained or suspected focal limb weakness that was not believed to arise from a stroke was categorized as limb weakness.
SPSS software (SPSS Inc., Chicago, IL, USA) was used for data analysis, and means with standard deviations and proportions with confidence intervals were calculated. Statistical comparisons were made using chi-square analysis, analysis of variance (ANOVA), and Student's t-tests, as appropriate. The threshold for statistical significance was set at p<0.05.
This study was approved by the Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation Institutional Review Board (approval no. 02-X24-110).
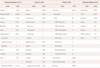
A total of 853 NILs occurred throughout the 1-year study period, during which 33,211 patients were admitted to the hospital. After excluding 649 patients who were admitted to the neurology ward and 4,051 pediatric patients, the liaison rate was about 3% per eligible admission case (n=28,511). The age of the patients was 70.5±16.3 years (mean±standard deviation). There was no significant difference in either mean patient age or male-to-female ratio between patients who received regular and emergency consultations or between patients in the regular wards and in the ICU (Table 1). The otolaryngology patients with NILs were younger (57.8±16.8 years) than for cardiology patients (76.1±13.9 years; p<0.0001, ANOVA). Patients with dementia were the oldest (82.2±8.9 years), while those with headache were the youngest (55.6±18.7 years; p<0.0001, ANOVA).
Emergency consultations comprised 5% of all consultations (43/853), and 15% (126/853) of consultation requests arose from the ICU, of which 68% (86/126) originated from physicians in the department of chest medicine. The departments of chest medicine, gastroenterology, and infectious disease were the three most frequently requested specialties for liaison, and comprised 55% of all NILs (466/853). The consulting neurologists completed 95% of emergency consultations within 2 hours and 85% of regular consultations within 24 hours. The consult-to-visit times for emergency and regular consultations were 44±47 minutes and 730±768 minutes, respectively; the overall was 696±763 minutes. The mean consult-to-visit time did not differ between the ICU and regular wards for emergency consultations. For regular consultations, the duration was shorter in the ICU (571±667 minutes) than in the regular wards (757±780 minutes; p=0.0151, unpaired t-test). The consult-to-visit time was shorter in cases of seizure (536±665 minutes) and stroke (601±888 minutes), and longer for neuromuscular disorders (935±861 minutes) and headache (902±1,101 minutes; p=0.032, ANOVA) (Table 2).
Altered consciousness, seizure, stroke, and movement disorders were the most often requested disorders, comprising 57% (488/853) of all NILs (Table 2). Doctors in the department of chest medicine most commonly requested NILs for these four conditions. Stroke, seizure, and altered consciousness were the most common reasons for emergency consultations (40/43, 93%). Of the 853 patients, 29 (3.4%) were transferred to the neurology ward after consultation. The transfer rate was higher for emergency consultations (5/43, 11.6%) than for regular consultations (24/810, 2.9%; p=0.0087, chi-square test).
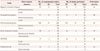
Table 3 lists the plausible etiologies for the four most common disorders prompting NILs. Causes of each disorder were multifarious in some cases; for example, sepsis and hyponatremia could occur simultaneously, with both contributing to altered consciousness. Infection was the most common cause of altered consciousness (72/174, 41%), followed by metabolic disorders (52/174, 30%), dementia (17/174, 10%), and hypoxia (12/174, 7%). Concurrent infection and metabolic disorder were observed in 12% (21/174) of patients. Delirium was the primary symptom of patients with dementia causing altered consciousness. A history of epilepsy (29/109, 27%) in patients who had seizures during hospitalization was the most common cause of seizure disorder. Other causes of seizure included infection (27/109, 25%), previous stroke (22/109, 20%), intracranial lesion (19/109, 17%), and metabolic disorder (15/109, 14%). Intracranial lesions included brain tumor, hydrocephalus, intracranial hemorrhage, and brain abscess. A history of epilepsy due to an old stroke occurred in 8% (9/109) of patients. Seizure disorder was excluded in 8% (9/109) patients after neurological consultation. Acute stroke was found in 44% (48/108) of patients with stroke disorder, followed by old stroke (26/108, 24%), and transient ischemic attack (6/108, 6%). Stroke was excluded in 26% (28/108) of patients. Four of the 48 patients with acute stroke developed intracranial hemorrhage. Another 44 patients experienced acute ischemic stroke. Of these patients, 57% (25/44) had large-artery atherosclerosis according to the Trial of ORG 10172 in Acute Stroke Treatment criteria;9 41% (18/44) of strokes occurred in the middle cerebral arterial territory. The most common cause of movement disorders was Parkinson's disease and related disorders (44/94, 45%), followed by tremor (23/97, 24%). Tension headache and migraine comprised 66% (29/44) of headache disorders. Other particular causes of headache included meningitis in four patients, metastatic brain tumor in three patients, and intracranial hypotension in two patients. Causes of limb weakness included myelopathy from metastatic spinal tumors in four patients, neuropathy in three, myositis in three, radiculopathy in two, and cerebrovascular disorder in two patients.
There was no difference in gender or mean age among patients in the regular wards and ICU (Table 4). The percentage of emergency consultations in the ICU (9/126, 7.1%) did not differ statistically from that in the regular wards (34/727, 4.6%). The average consult-to-visit time was shorter in the ICU than in the regular wards (533±657 minutes vs. 724±777 minutes; p=0.004, unpaired t-test). As indicated in Table 1, this difference was significant for regular consultations but not for emergency consultations. Altered consciousness, seizure, and stroke accounted for 84% of neurological consultations in the ICU but only 39% of them in the regular wards (p<0.001, chi-square test).
Six main studies were suggested by neurologists during NILs: magnetic resonance imaging (MRI), computed tomography (CT), electroencephalography (EEG), nerve conduction velocity (NCV), color-coded carotid (CCD) with or without transcranial (TCCS) duplex sonography, and evoked potential. Table 5 lists the studies recommended by the consulting neurologists and those that were actually performed by the referring physicians after consultation. The overall performance rate for all six recommended studies was 73% (553/760). EEG was the most often recommended investigation, and was most frequently requested due to altered consciousness and seizure disorder. MRI and CT were recommended for disorders of altered consciousness and stroke. CCD with or without TCCS was recommended for stroke and dizziness. NCV was suggested for neuromuscular disorders and limb weakness. The measurement of evoked potentials was recommended for patients with dizziness or vertigo. EEG was performed in 83% (241/289) of recommendations and was the study that was performed most often after NILs. The performance rates for other studies varied between 55% and 70%. Epileptiform discharge on EEG was found in 31 out of 241 patients (13%). Ten of these cases proved to be nonconvulsive status epilepticus (five patients with altered consciousness, four with seizure, and one with stroke disorder). Twenty out of 53 patients (38%) had extracranial carotid stenosis of 50% or more or intracranial atherosclerosis during CCD/TCCS, which required antiplatelet treatment.
The Taiwan Joint Commission on Hospital Accreditation recommends that inpatient emergency and regular consultations be completed within 2 hours and 24 hours, respectively. Nevertheless, there is no recommendation on the ideal percentages of those consultations completed within these time limits. In the present analysis, 95% of emergency consultations were completed within 2 hours and 85% of regular consultations were completed within 24 hours. These percentages are in line with quality control targets in our hospital setting (90% for emergency consultations and 85% for regular consultations). Ali et al.10 reported that the use of a Web-based internal neurology referral service resulted in them seeing 77% (782/1016) of patients within 24 hours of referral, of which 40% were seen in the emergency room and 87% were reviewed by consultant neurologists. In the present study, all of the referred patients were inpatients and were reviewed by a consultant neurologist.
The liaison rate per each admission case was 3% in this study, which was lower than the previously observed percentage of 15-20% of inpatients with neurological problems.3 There are several possible reasons for the low inpatient liaison rate:
1) Most patients with significant neurological symptoms in the emergency room had been evaluated by neurologists through emergency consultations and were admitted to the neurology ward. This is also likely to be a reason for the small percentage of emergency consultations (5%) among all NILs.
2) Patients who have neurological disorders might already have received treatment at the outpatient neurology clinic, and physicians tended to contact the neurologist directly via a phone call to obtain recommendations.
3) Some minor neurological symptoms that are clearly not correlated with the patient's hospitalization might not be considered as a problem requiring an NIL.
The chest medicine, gastroenterology, and infectious disease departments had the largest numbers of inpatients in the medical wards and thus requested more than half of all the NILs, with the department of chest medicine requesting the most NILs. In addition, half of these inquiries arose from the ICU. It is not surprising that cardiology patients were much older than the otolaryngology patients, since coronary and cerebral arterial diseases share similar pathogeneses and commonly occur in older people. Similarly, patients with dementia, movement disorders, and stroke were older than patients with headache disorders.
Common neurological disorders involving liaison varied according to the practice setting and the fundamental characteristics of each institution. In this study, which focused on the inpatient wards, altered consciousness, seizure, stroke, and movement disorder contributed to 58% of the NILs. Altered consciousness was the problem that the other specialties were most concerned about, despite the presence of severe medical illness. A neurological evaluation is frequently requested to exclude the possible coexistence of a brain lesion, such as a stroke or seizure. However, systemic infections and metabolic disorders were the two most common causes of altered consciousness in this study. In septic encephalopathy, the release of cytokines, procalcitonin, tumor necrosis factor α, and interleukin 6 might lead to altered cerebral hemodynamics, disruption of the blood-brain barrier, cerebral edema, and disturbed neuronal function.411 In metabolic encephalopathy, interruption of the delivery of energy substrates to the brain (in hypoglycemia and hypoxia) or altered neuronal excitability (in hepatic and renal failure, and electrolyte imbalance) result in an altered mental state.4 Stroke, intracranial lesion, and seizure only contributed to 16% (28/174) of altered-consciousness NIL requests in the present study.
Previous studies have shown that cerebrovascular disease is the most common reason for NILs, prompting 17.2-29% of total NIL requests.356712 Stroke is the most common neurological disorder in our hospital, but since neurologists care for most patients with acute stroke in the emergency room, stroke occurs infrequently in specialty wards. None of the 62 patients who experienced acute stroke in the hospital fulfilled the criteria for intravenous thrombolytic therapy. Some strokes occurred during night sleeping, but they exceeded the 3-hour "golden time," and some patients had concomitant severe illness that precluded thrombolytic therapy. It is interesting that stroke was excluded in 26% of patients who were initially suspected of stroke syndrome. The probability of a stroke diagnosis after a NIL was close to the value of 72% on the Cincinnati Prehospital Stroke Scale for the presence of any one of three signs (arm weakness, speech, and facial droop).13 Ferro et al.14 noted that nonneurologists make a correct diagnosis of acute stroke in up to 85% of cases. Validating a stroke diagnosis may be more difficult in inpatients due to the presence of concomitant illnesses.
Seizure and collapse were the most commonly reported reasons for neurological referrals in two studies.1015 A high level of diagnostic agreement exists between neurologists and former specialists regarding convulsive seizures. A history of epilepsy was noted in 27% of patients who developed seizures during hospitalization. Withdrawal of anticonvulsant medications or acute illness, such as infection or metabolic disorders, may be precipitating factors for seizure recurrence. The first episode of seizure had various etiologies. Newly diagnosed intracranial lesions corresponding to seizure were found in 17% (19/109) of patients, and 15 of these 19 patients required prompt treatment of the lesion (tumor, hemorrhage, and abscess) in addition to seizure control. Although epileptiform discharges were detected in only 13% of all EEG studies, abnormal EEG findings indicated to the referring physicians that ten patients had nonconvulsive status epilepticus. All of these patients improved gradually after receiving appropriate anticonvulsant treatment. Towne et al.16 reported that nonconvulsive status epilepticus occurred in 8% of all comatose patients without signs of seizure activity. They recommended that EEG be included in the routine evaluation of comatose patients, even when clinical seizure activity is not apparent.16
Parkinson's disease and related disorders were the primary disorders in the patients with movement disorders. Aggravation of rigidity or tremor, or unfamiliarity with the appropriate dosage of antiparkinsonism medications prompted the need for an NIL. Stroke, seizure, and altered consciousness were the most common disorders, comprising 93% (40/43) of all emergency consultations and 84% (106/126) of consultations in the ICU. Active intracranial lesions were found in 89 of the 391 patients (17%) with these 3 disorders. These lesions included acute stroke in 62 patients, brain tumor in 13, transient ischemic attack in 6, central nervous system infection in 5, and subdural hematoma in 3 patients. Combined with the other 95 patients with seizures (85 with seizure disorders, 8 with altered consciousness, and 2 with stroke disorder but not with stroke), and 9 patients with delirium due to dementia, 193 patients out of 391 patients (49%) warranted an immediate diagnosis and prompt treatment as suggested by consulting neurologists. In addition, intracranial lesions such as meningitis, metastatic brain tumor, and intracranial hypotension were found in 9 out of 44 patients (20%) with headache disorder.
Patients were transferred to the neurology ward more often after an emergency consultation (11.6%) than after a regular consultation (2.9%). Most patients transferred to the neurology ward had acute stroke or intractable seizures. The consult-to-visit times were almost the same for patients requiring emergency consultations, regardless of whether they were in a regular ward or the ICU. Only 7.1% of NILs in the ICU were emergency consultations. A consult-to-visit time within 24 hours for a regular consultation is considered acceptable by most ICU physicians in this hospital. The average consult-to-visit time for a regular consultation was 33% shorter for patients in the ICU (571 minutes) than in the ward (757 minutes). Neurologists had a higher level of alertness and tended to visit patients earlier when they received liaison requests from the ICU. The consult-to-visit times are shorter for seizure disorders and stroke and are longer for neuromuscular disorder and headache. The symptoms prompting the liaisons also affect the time taken for neurologists to visit patients.
EEG was both the most common recommended and performed study, particularly in patients with altered consciousness and seizure disorder. MRI and CT were recommended more in patients with altered consciousness and stroke. Although CT is more convenient, rapid, and widely available than MRI, one explanation for there being fewer recommendations for CT than for MRI by neurologists is that some patients had already had CT studies before their NIL. CCD/TCCS is regarded as an essential study for patients with stroke in Taiwan. In the present study, stenotic carotid artery disease or intracranial atherosclerosis was detected in 6 out of 18 patients with dizziness or vertigo, and these patients received long-term antiplatelet treatment after the study.
NILs are typically time-consuming and sometimes require several revisits and follow-ups. The secondary referral hospital where this study was conducted did not have a resident doctor trained in neurology. In addition to daily neurological work at the outpatient clinic, inpatient ward service, and the neurological electrophysiology laboratory, neurologists also rotate through the hospital, providing a 24-hour service for inpatient care and consultation. There were 1,340 emergency consultations arising from the emergency room during the same 1-year period as in this study. Together with the 853 NILs, there were 2,193 neurological consultations during the 1-year period. The requested consult-to-visit time for an emergency consultation from the emergency room was 30 minutes, which was much shorter than that for inpatient emergency consultations (120 minutes). When a special "cerebrovascular accident call" is initiated from the emergency room for a suspected acute stroke occurring within 3 hours, the on-duty neurologist is required to evaluate the patient in the emergency room immediately so that intravenous thrombolytic therapy can be provided within 1 hour of the patient's arrival. Although not all neurologists in Taiwan participate in emergency consultations outside of office hours, the new workload burden of neurologists for emergency consultations associated with 24-hour acute thrombolytic therapy-particularly for so-called stroke neurologists-has developed a "neurophobia" among young doctors. Fewer and fewer medical students are willing to devote themselves to clinical neuroscience. The "invisible" work from inpatient and emergency room referrals with very little resources has become a hazard for neurologists.5 A new concept of a "neurohospitalist" for inpatient neurological care is a possible solution to this problem.17
In conclusion, half of the patients presenting with altered consciousness, seizure, and stroke have acute neurological diseases that warrant immediate diagnosis and treatment by neurologists. Balancing increasing neurologist workloads and appropriate health-care resources remains a significant challenge.
Figures and Tables
Table 1
Specialties requesting neurological inpatient liaison (NILs) in the 853 study patients by types of consultations and wards

Table 2
Reasons for requesting NILs in 853 patients by type of consultation, age, consult-to-visit time, specialty, and transfer to the neurology ward

Table 3
Plausible causes of the four most common disorders prompting NILs in 488 patients
*Multiple causes might contribute to the etiology of altered consciousness or seizure.
ACA: anterior cerebral artery, MCA: middle cerebral artery, NILs: neurological inpatient liaisons, PCA: posterior cerebral artery, TOAST: Trial of ORG 10172 in Acute Stroke Treatment diagnostic classification of ischemic stroke.
Table 4
Comparison of neurological consultations in the ICU and regular wards in 853 patients

Table 5
Recommended and carried out investigations according to neurological consultation
Acknowledgements
We wish to thank to Professor Meei-Shyuan Lee for her help on reviewing the statistic analysis.
The study was supported by grants from the Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (TCRD-TPE-103-RT-16) and (TCRD-TPE-103-RT-7).
References
1. Department of Statistics, Ministry of Interior, ROC. Interior Affair Statistic Bulletin [Internet]. Taiwan: Department of Statistics, Ministry of the Interior, R.O.C. Taiwan;2013. Available from: http://www.moi.gov.tw/files/news_file/week10233.pdf.
2. Lin MH, Chou MY, Liang CK, Peng LN, Chen LK. Population aging and its impacts: strategies of the health-care system in Taipei. Ageing Res Rev. 2010; 9:Suppl 1. S23–S27.

3. Morrow JI, Patterson VH. The neurological practice of a district general hospital. J Neurol Neurosurg Psychiatry. 1987; 50:1397–1401.

4. Razvi SS, Bone I. Neurological consultations in the medical intensive care unit. J Neurol Neurosurg Psychiatry. 2003; 74:Suppl 3. iii16–iii23.

5. Douglas MR, Peake D, Sturman SG, Sivaguru A, Clarke CE, Nicholl DJ. The inpatient neurology consultation service: value and cost. Clin Med. 2011; 11:215–217.

6. Steiger MJ, Enevoldson TP, Hammans SR, Ginsberg L. Influence of obtaining a neurological opinion on the diagnosis and management of hospital inpatients. J Neurol Neurosurg Psychiatry. 1996; 61:653–654.

7. Costello DJ, Renganathan R, O'Hare A, Murray B, Lynch T. Audit of an inpatient neurology consultation service in a tertiary referral centre: value of the consulting neurologist. Ir Med J. 2005; 98:134–137.
8. Forbes R, Craig J, Callender M, Patterson V. Liaison neurology for acute medical admissions. Clin Med. 2004; 4:290.

9. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.

10. Ali E, Chaila E, Hutchinson M, Tubridy N. The 'hidden work' of a hospital neurologist: 1000 consults later. Eur J Neurol. 2010; 17:e28–e32.

12. Carroll C, Zajicek J. Provision of 24 hour acute neurology care by neurologists: manpower requirements in the UK. J Neurol Neurosurg Psychiatry. 2004; 75:406–409.

13. Kothari R, Hall K, Brott T, Broderick J. Early stroke recognition: developing an out-of-hospital NIH Stroke Scale. Acad Emerg Med. 1997; 4:986–990.

14. Ferro JM, Pinto AN, Falcão I, Rodrigues G, Ferreira J, Falcão F, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke. 1998; 29:1106–1109.
15. Perkin GD. Necessity for inpatient services in neurological practice. J R Soc Med. 1983; 76:920–923.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download