Dear Editor,
Anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis is a form of autoimmune encephalitis involving anti-NMDAR antibodies, which is specific to the NR1/NR2 heteromers of the NMDAR.1 To the best of our knowledge, herein we report the first case of anti-NMDAR encephalitis associated with systemic lupus erythematosus (SLE).
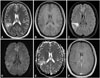
A 33-year-old woman presented to our hospital with complex partial seizures. Her medical history included SLE for the previous 12 years and bilateral avascular necroses. Her SLE was previously treated with immunosuppressive agents such as cyclophosphamide, and at the current presentation she was receiving treatment with prednisone (5 mg/day) and hydroxychloroquine (400 mg/day). Her score on the Systemic Lupus Erythematosus Disease Activity Index 2000 was 8. Brain MRI showed right temporal and parietal lobe mild hyperintensity on T1-weighted and T2-weighted images, respectively, and hyperintensity on fluid attenuated inversion recovery sequences; a similar signal was observed on diffusion-weighted imaging. The MRI enhancement appeared as ring-shaped reinforcement (Fig. 1). A CSF sample showed normal intracranial pressure (115 mmH2O) and levels of, 2 leukocytes, protein (0.28 g/L), glucose (2.91 mmol/L), and chlorine. The results of viral serological and CSF analyses were negative. We used human embryonic kidney 293 cells expressing the NR1 subunit of NMDARs to test for the presence of NMDAR antibodies in serum (1:10 initial dilution) and CSF (no dilution). Antibodies binding to the surface of NMDAR-HEK293 cells were identified by fluorescence microscopy using a test kit (EUROIMMUN Medical Laboratory Diagnostics). Both the serum and CSF exhibited weak positivity for anti-NMDAR antibodies. The patient also exhibited positive results for tests for antinuclear antibodies (titer, 1:320), and anti-U1-nRNP and anticentromere antibodies, but negative results for anti-double-stranded DNA antibodies and anti-ribosomal-P protein antibodies. Screening tests for occult tumors produced negative results. On day 8 she underwent a comprehensive neuropsychological assessment, and all test results were normal. The patient was treated with oral prednisone.
The medical history of this case included SLE, and the first presenting symptom was a seizure. In contrast to previous reports,23 no other clinical manifestations were seen in our patient. Brain MRI showed lesions in the right temporal and parietal lobes. She was misdiagnosed as neuropsychiatric SLE (NPSLE) until tests revealed the presence of anti-NMDAR antibody in her CSF and serum.
NPSLE is an autoimmune disease, common symptoms of which include cerebrovascular disease, seizures, cognitive dysfunction, and headache.4 The first presenting symptom of our patient was seizure. Although 80% of patients with anti-NMDAR encephalitis reportedly have seizures,2 another study found that only 28% and 33% of those with primary NPSLE and secondary NPSLE, respectively, had seizures.4 Since anti-NMDAR encephalitis and NPSLE share similar clinical features, it is difficult to distinguish the disease unless specific antibodies are tested for.
The correlation between anti-NMDAR encephalitis and SLE is yet to be clarified. Previous studies have found autoantibodies to an NR2 peptide of NMDAR in 25–30% of SLE patients, and these autoantibodies might play a role in cognitive dysfunction and psychiatric disease.56 DeGiorgio et al.7 showed that lupus antibodies could cross-react with the NMDA receptor, and could mediate neural death via an apoptotic pathway.
Mackay et al.8 described two patients presenting with progressive cognitive dysfunction and NMDAR antibodies with sporadic Creutzfeldt-Jakob disease (CJD). Those authors suggested that the immune response was due to NMDA receptors released from damaged neurons, and further believed that a positive antibody test did not exclude CJD. Anti-NMDAR encephalitis and NPSLE have previously been demonstrated to be associated with the NR1 subunit and NR2 subunit, respectively. Ogawa et al.9 showed that autoantibodies to the NMDAR NR1 subunit were expressed in SLE, especially in NPSLE. They also suggested that autoantibodies to that subunit could be involved in the pathogenesis of NPSLE. Our case showed weak positivity for anti-NMDAR antibodies in both serum and CSF. Zandi et al.10 mentioned that weak positivity is unlikely to mislead clinicians, but it could result in an opportunity for treatment being missed. Therefore, further studies are required to delineate the mechanism of anti-NMDAR encephalitis with SLE.
The treatment for SLE-associated anti-NMDAR encephalitis has not been established conclusively. The conventional recommended treatment for anti-NMDAR encephalitis is methylprednisolone plus immunoglobulin or plasma exchange as the first-line therapy, and rituximab, cyclophosphamide, or their combination as the second-line therapy.3 In the US, only three compounds have been approved by the Food and Drug Administration for SLE treatment: glucocorticoids, aspirin, and hydroxychloroquine.5 Cyclophosphamide is the only drug used to treat SLE in cases of organ-threatening disease.3
The present case is a reminder that SLE with seizures could lead to a diagnosis of NPSLE and also of anti-NMDAR encephalitis. This case and previous reports suggest that SLE is an indicator in the development of anti-NMDAR encephalitis. Whether lupus antibodies cross-react with NMDAR—possibly resulting in neuropsychiatric disorders—should be further assessed in more cases.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download