Abstract
Background and Purpose
Neuropathic pain (NeuP) associated with traumatic brachial plexus injury (BPI) can be severe, persistent, and resistant to treatment. Moreover, comorbidity associated with NeuP may worsen the pain and quality of life. This study compared persistent NeuP after BPI between patients with and without co-morbid conditions (psychiatric dysfunction and other painful conditions) and tramadol usage as a second-line agent in combination with an antiepileptic and/or antidepressant during a 2-year follow-up.
Methods
The medical records of patients diagnosed with BPI referred to a pain center between 2006 and 2010 were reviewed for 2 years retrospectively. Data regarding patient demographics, injury and surgical profiles, characteristics of NeuP and its severity, and treatment received were compared between patients with and without manifesting co-morbid conditions. The NeuP and pain intensity assessments were based on the DN4 questionnaire and a numerical rating scale, respectively.
Results
Of the 45 patients studied, 24 patients presented with one of the following co-morbid conditions: myofascial pain (21%), psychiatric disorder (17%), phantom limb pain (4%), complex regional pain syndrome (21%), and insomnia (37%). Tramadol was required by 20 patients with co-morbidity and, 9 patients without co-morbidity (p<0.001). The mean pain score after 2 years was higher in patients with co-morbidity than in those without co-morbidity (p<0.05).
The underlying causes of brachial plexus injury (BPI) include compression, ischemia, metabolic condition, infection, neoplasia, radiation, and trauma being the most common cause.123 The advent of both diagnostic and prognostic neurophysiological tests, and microsurgical techniques has improved the functional recovery following BPI over the past decade. Nevertheless, BPIs are devastating injuries that are difficult to manage and require a holistic approach.
The incidence of the chronic pain following traumatic BPI is reported to be as high as 50%.4 Moreover, the neuropathic pain (NeuP) that develops after BPI becomes resistant to narcotic analgesics,5 and NeuP reduces the quality of life, including mood, physical, and social functioning.67 Hence, early aggressive treatment with a multidisciplinary team approach is essential to preventing refractory pain.
As for any other chronic pain condition, subjects with NeuP are likely to have co-morbidities such as sleep disturbances and mood disorder. These coexisting co-morbidities can worsen the pain and complicate the treatment if they are not addressed in the overall management strategy. Therefore, the purpose of this study was to determine the occurrence of co-morbidities (especially psychiatric illness and other painful conditions) following BPI induced NeuP and their effect on pain severity and tramadol usage as a second-line agent in combination with an antiepileptic and/or antidepressant during a 2-year follow-up.
The medical records of patients diagnosed with BPI and referred to the Multidisciplinary Pain Center, for evaluation and possible treatment of their chronic pain condition between 2006 and 2010 were reviewed retrospectively. Patient files were reviewed after receiving approval from the Institutional Review Board (approval number Si 289/2012).
Data from the medical chart of each patient were reviewed by one of the authors who had not been involved in the evaluation or treatment of the patients. Information was obtained regarding patient demographics, injury profile, and radiological evaluation of the location of the injury in relation to the dorsal root ganglion, surgical interventions, and pain management.
Data regarding the characteristics of NeuP and, both pharmacological and non-pharmacological therapies received during the 2-year follow-up were recorded. The Thai version of the DN4 questionnaire was used for screening NeuP. Light touch and pinprick sensations were assessed using cotton wool and disposable pins, respectively. The pain intensity was assessed using a numerical rating scale at 0 week, 2 weeks, 1 month, 3 months, 1 year, and 2 years. Likewise, the incidences of co-morbid factors related to psychiatric dysfunction and other painful conditions that can influence the severity of pain over the follow-up period were recorded.
Data are presented as mean and standard deviation values for continuous variables, and frequencies and percentages for categorical variables. Student's t-test was used to campare continuous variables, while the chi-square test and Fisher's exact test were used for categorical variables as appropriate. The pain severities in the groups during the follow-up were compared using one-way ANOVA test. A p value of <0.05 was considered to indicate statistical significance. All statistical analyses were performed using SPSS software (version 16.0, SPSS Inc., Chicago, IL, USA).
Of the 58 patients studied, 48 patients met the criteria for NeuP according to responses on the DN4 questionnaire. Three patients were excluded (2 lost during follow-up and 1 with incomplete information), and so 45 subjects were finally analyzed. At the time of first visit to the pain clinic, the patients presented with the following symptoms and signs: sensations of electric shock (91%), pins and needles (46%), burning (31%), tingling (26%), painful cold (24%), numbness (48%), allodynia (26%), and itching (7%), with mixed pain characteristics appearing in 19 patients (42%). The distribution of pain characteristics among the patients with and without co-morbid conditions is presented in Table 1. Seventeen (38%) patients experienced pain at ≥3 months after injury, while 28 (62%) patients experienced the early onset of pain (<3 months).
During the 2-year follow-up, 24 patients manifested co-morbidities of psychiatric disorders and other painful conditions. Myofascial pain, psychiatric disorder, phantom limb pain, complex regional pain syndrome (CRPS), and insomnia were observed in five (21%), four (17%), one (4%), five (21%), and nine (37%) patients, respectively. Four patients experienced psychiatric dysfunction: two with depression and two with posttraumatic stress disorder (PTSD). The demographic, injury, and surgical profiles of the patients are presented in Table 2 and 3. Table 4 lists the various pharmacological and non-pharmacological treatments that the patients received during the study period. Fig. 1 compares the severity of pain between patients with and without co-morbidities during the 2-years follow-up.
Subgroup analysis of 24 patients in co-morbid group dichotomized into other painful conditions (11 patients) and psychiatric co-morbidity, including insomnia (13 patients) did not show a significant difference in pain severity or for opioid usage at the 2-year (p>0.05).
Following BPI, early rehabilitation with restoration of the maximum function of the affected limb is the ultimate goal. However, severe pain following BPI can be a major limiting factor for rehabilitation, and this can result in a poor outcome.8 Moreover, NeuP manifesting after BPI makes iteven more difficult to treat, causing a significant impact on a person's quality of life.
We used the Thai version of the DN4 questionnaire to screening the NeuP characteristics, since this questionnaire has been systematically translated and validated and is also simple to apply in clinical setting.910 The DN4 questionnaire has good sensitivity and specificity, but there is no single gold standard diagnostic test that provides a definite diagnosis of NeuP. Because of the lack of a specific diagnostic tool, the NeuPSIG (Special Interest Group on NeuP) has developed a revised definition with an algorithm for diagnosing NeuP, defining this using five levels of certainty.11 Neurological examinations based on this grading system indicated that all of our patients had definite NeuP. Electromyography and nerve conduction studies were performed to support the diagnosis. Further, a confirmatory diagnosis was performed using standard CT myelography to determine the location and severity of injury, since certain limitations and pitfalls are associated with electrophysiological studies.12 Our study showed that 82.7% of the patients with BPI who were referred to the pain clinic had NeuP. This prevalence of painful neuropathy after traumatic peripheral nerve injury is similar to the findings of other studies,1314 suggesting that most patients are likely to manifest NeuP after such an injury.
More than half of the patients in our study developed various associated co-morbid conditions during the follow-up period. These patients were more likely to experience severe persistent pain than those without co-morbidity. The higher pain intensity and the poor response to medication in this group may be due to the manifestation of other painful conditions (such as CRPS, myofascial pain, and phantom limb pain) or psychiatric co-morbidities. A relatively high percentage of patients reported insomnia as one of the co-morbid conditions. It is evident from the literature that there are moderate positive correlations between pain intensity and sleep disorders causing a significant reduction in the quality of life.1516 Insomnia in chronic pain is under-reported and under-treated. With the currently available medication achieving only limited success, early non-pharmacological interventions are essential before it becomes difficult to treat insomnia when it occurs in association with chronic painful conditions.
Psychiatric morbidity in terms of depression, anxiety, and PTSD further exaggerates the chronic pain disorders. NeuP itself is a risk factor for the manifestation of depressive symptoms, and several studies have highlighted the association of emotional liability and lack of sleep with specific NeuP conditions.17 Patients suffering with post-herpetic neuralgia reportedly experience physical and psychological impairments that are correlated with higher pain intensity.18 Likewise, painful diabetic polyneuropathy significantly affects various aspects of the quality of life, including sleep disorders.19 Similar to these studies, we observed a statistically significant change in pain severity after the 2-year follow-up in patients who manifested co-morbid illness compared to those who did not manifest a comorbidity. Therefore, the physician should be vigilant and regularly screen these high-risk patients for depression or other psychiatric illness, especially when a change in pain symptoms or functional impairment is noticed.
Antiepileptic and/-or antidepressant agents were used as first-line drugs to treat NeuP in both of the present study groups, while tramadol was added in combination with these agents only when pain was persistent. The findings from a recent meta-analysis of pharmacotherapy for NeuP also suggest using antiepileptic/antidepressant as a first-line treatment and tramadol as a second-line treatment in painful neuropathy. 20 Moreover, combining an opioid with antiepileptic and/-or antidepressant agents for NeuP may improve the analgesic efficacy.21 However, no beneficial effect was observed in our patients who presented with co-morbidities. Significantly, more patients with co-morbidities required tramadol, and the pain was still severe in this group. An inadequate response to tramadol could be attributed to the associated co-morbid illness itself, which might have aggravated the pain, making the addition of tramadol ineffective.
An interesting finding in this study was the occurrence of CRPS in the co-morbid group, with five patients (21%) manifesting it during the course of the 2-year follow-up. The diagnosis of CRPS was based on clinical criteria,22 and patients received a stellate ganglion block with local anesthesia to confirm the diagnosis. A positive response to a sympathetic block revealed the presence of sympathetic dysfunction in these patients. Due to the direct injury of brachial plexus, all our patients had fulfilled the criteria of type II CRPS. Nevertheless, it is difficult to differentiate NeuP from CRPS clinically because most of the clinical features are common to both conditions. The involvement of peripheral nerve injury in CRPS II means that, it also fulfills the new definition of NeuP. A recent study found that, ultrasound scans of muscle could be used to distinguish between these two entities, since the normal myoarchitecture was preserved in NeuP, while loss of muscle structure was observed in the CRPS group.23 Those authors found that the degree of disability was greater in CPRS than inNeuP, making this differentiation essential. This could be one of the reasons for the persistent pain experienced by the present patients manifesting CRPS.
One of the limitations of this study was that its design as a retrospective review made it impossible to explore how the quality of life changed over a period of time. However, our findings do indicate that further prospective clinical trials should be conducted in patients with BPI and NeuP to show how associated other painful conditions or co-morbidities influence the quality of life.
In conclusion, the pain intensity was more severe in patients developing NeuP after BPI manifesting other painful conditions or co-morbidities than in those without co-morbidities during a 2-year follow up. Since a co-existing painful condition or co-morbidities can worsen the pain and quality of life, an effective interdisciplinary management plan should focus on treating co-morbid conditions as early as possible, in addition to treating the pain itself.
Figures and Tables
Fig. 1
Mean pain scores on the numerical rating scale for patients with and without a co-morbid condition during the 2-year follow-up. *p<0.01.
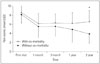
Table 1
Pain characteristics among patients with and without co-morbid conditions

Table 2
Demographic and injury profiles of the patients

Table 3
CT myelography, root level involved, and surgical profile of the patients

Table 4
Treatment received by the patients during the 2-year follow-up

References
1. Wilbourn AJ. Brachial plexus disorders. In : Dyck PJ, Thomas PK, editors. Peripheral neuropathy. 3rd ed. Philidelphia: WB Saunders;1993. p. 911–950.
2. Ferrante MA. Brachial plexopathies: classification, causes, and consequences. Muscle Nerve. 2004; 30:547–568.

3. Mullins GM, O'Sullivan SS, Neligan A, Daly S, Galvin RJ, Sweeney BJ, et al. Non-traumatic brachial plexopathies, clinical, radiological and neurophysiological findings from a tertiary centre. Clin Neurol Neurosurg. 2007; 109:661–666.

4. Giuffre JL, Kakar S, Bishop AT, Spinner RJ, Shin AY. Current concepts of the treatment of adult brachial plexus injuries. J Hand Surg Am. 2010; 35:678–688. quiz 688.

5. Bruxelle J, Travers V, Thiebaut JB. Occurrence and treatment of pain after brachial plexus injury. Clin Orthop Relat Res. 1988; (237):87–95.

6. Ranalli NJ, Kline DG, McGarvey ML, Boulis NM, Zager EL. Clinical problem-solving: brachial plexus closed injury and reconstruction. Neurosurgery. 2008; 62:1330–1338. discussion 1338-1339.
7. Geisser ME, Roth RS, Theisen ME, Robinson ME, Riley JL 3rd. Negative affect, self-report of depressive symptoms, and clinical depression: relation to the experience of chronic pain. Clin J Pain. 2000; 16:110–120.

8. Terzis JK, Kostopoulos VK. The surgical treatment of brachial plexus injuries in adults. Plast Reconstr Surg. 2007; 119:73e–92e.

9. Chaudakshetrin P, Prateepavanich P, Chira-Adisai W, Tassanawipas W, Leechavengvongs S, Kitisomprayoonkul W. Cross-cultural adaptation to the Thai language of the neuropathic pain diagnostic questionnaire (DN4). J Med Assoc Thai. 2007; 90:1860–1865.
10. Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005; 114:29–36.

11. Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 2008; 70:1630–1635.

12. Koo YS, Cho CS, Kim BJ. Pitfalls in using electrophysiological studies to diagnose neuromuscular disorders. J Clin Neurol. 2012; 8:1–14.

13. Tantigate D, Wongtrakul S, Vathana T, Limthongthang R, Songcharoen P. Neuropathic pain in brachial plexus injury. Hand Surg. 2015; 20:39–45.

14. Ciaramitaro P, Mondelli M, Logullo F, Grimaldi S, Battiston B, Sard A, et al. Traumatic peripheral nerve injuries: epidemiological findings, neuropathic pain and quality of life in 158 patients. J Peripher Nerv Syst. 2010; 15:120–127.

15. Stiefel F, Stagno D. Management of insomnia in patients with chronic pain conditions. CNS Drugs. 2004; 18:285–296.

16. Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. 2004; 8:119–132.

17. Nicholson B, Verma S. Comorbidities in chronic neuropathic pain. Pain Med. 2004; 5:Suppl 1. S9–S27.

18. Mauskopf J, Austin R, Dix L, Berzon R. The Nottingham Health Profile as a measure of quality of life in zoster patients: convergent and discriminant validity. Qual Life Res. 1994; 3:431–435.

19. Dermanovic Dobrota V, Hrabac P, Skegro D, Smiljanic R, Dobrota S, Prkacin I, et al. The impact of neuropathic pain and other comorbidities on the quality of life in patients with diabetes. Health Qual Life Outcomes. 2014; 12:171.

20. Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015; 14:162–173.

21. Moulin D, Boulanger A, Clark AJ, Clarke H, Dao T, Finley GA, et al. Pharmacological management of chronic neuropathic pain: revised consensus statement from the Canadian Pain Society. Pain Res Manag. 2014; 19:328–335.

22. Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. 2nd ed. Seattle: IASP Press;1994.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download