Abstract
Background and Purpose
There is conflicting evidence for whether or not the incidence of stroke is influenced by the daily temperature. The association between daily temperature and incidence of stroke is largely unknown in Korea. This study attempted to evaluate whether the maximum or minimum daily temperature is associated with increased numbers of strokes and stroke subtypes among Seoul residents.
Methods
We obtained the maximum and minimum daily temperatures in Seoul from the Korean Meteorological Administration between January 2005 and December 2014. Consecutive patients with acute stroke were registered who visited the emergency room or outpatient clinic in Soonchunhyang University Hospital, Seoul. The residential addresses of cases were restricted to within a 2-kilometer radius of this hospital. The stroke events were prospectively recorded with onset time, and were classified by subtypes. The categories of daily temperature were divided by 10℃ from the mean temperature. The mean daily number of strokes was calculated during the study period. One-way analysis of variance and Duncan's post-hoc test were applied to compare the number of strokes among the temperature groups.
Results
In total, 2,313 acute strokes were identified during the period: 1,643 ischemic strokes and 670 hemorrhagic strokes. The number of cases was significantly higher when the maximum daily temperature was >32℃ or ≤3℃ (p=0.048) or the minimum daily temperature was ≤-11.0℃ (p=0.020). The lowest maximum daily temperature was associated with increased instances of intracerebral hemorrhage (p=0.029) and small-vessel occlusion (p=0.013), while the highest maximum daily temperature was associated with an increased instance of large-artery atherosclerosis (p=0.045).
Stroke is a leading cause of death and disability in Korea, with approximately 105,000 Korean citizens experiencing a new or recurrent stroke annually.1 Environmental factors crucially affect the incidence of stroke, and the meteorological conditions might also significantly influence the seasonal and daily variations of the incidence of stroke. To reduce the burden of stroke, it is crucial to identify modifiable risk factors. However, the association between daily temperature and the incidence of stroke has been largely unknown in Korea.
Several studies have found changes in meteorological parameters and seasonal variation to be associated with stroke worldwide. Most previous studies have focused on the relationship between the incidence of stroke and seasonal variations, and demonstrated that the incidence of stroke increases in winter and spring.23456 Other studies have found no associations between weather and the incidence of stroke.78 However, all of the studies have described differences in temperature between the dates with and without stroke. There have been few reports on stroke incidence according to daily meteorological characteristics, or on the relationship between daily temperature and stroke subtypes. One report described that the incidence of ischemic stroke was significantly higher during summer and early autumn, whereas hemorrhagic stroke was more common in spring and winter in Korea.9 However, the influence of daily temperature on the incidence of stroke or on stroke subtypes has not been reported previously.
This study aimed to determine whether daily temperatures increase the short-term number of stroke patients and stroke subtypes in Seoul, Korea. Data on the daily meteorological conditions around our hospital over a 10-year period were collected, and the number of strokes was compared in different temperature groups.
Meteorological parameters were obtained from the Korean Meteorological Administration. The variables included the maximum and minimum daily temperatures, mean daily temperature, daily temperature range, day-to-day temperature differential, and average humidity for all days between January 1, 2005 and December 31, 2014 in Seoul (n=3,652 days). Seoul experiences four distinct weather patterns during the seasons of spring, summer, autumn, and winter.
The categories of daily temperature were divided by 10-degree Celcius (℃) from the mean temperature. The daily temperatures in Seoul did not conform to a normal distribution, this ensured that the number of days in the highest temperature group were similar to those in the corresponding lower temperature group, which was divided by 5℃.
In total, 3,480 consecutive patients with acute (<7 days) ischemic or hemorrhagic stroke were admitted to Soonchunhyang University Hospital during the study period. This center is a tertiary hospital centrally located in Seoul. We determined the area within which the emergency medical service system (119) transports patients to our center. The district includes 21 neighborhoods in Yongsan-gu, Jung-gu, west Seongdong-gu, north Seocho-gu, and north Gangnam-gu. The nearest tertiary hospital is located 4.6 kilometers east of our hospital. Therefore, to minimize selection bias, we excluded patients whose residential addresses were outside a 2-kilometer radius of this hospital. The population included 562,513 adult inhabitants (aged >19 years) based on the Korean population census in 2015. Cases of medical emergencies in selected areas are obliged to be transferred to our center according to the 119 guidelines, and can normally reach our center within 10 minutes by car. About 350 patients with acute ischemic stroke are admitted to our center each year, and the area distribution of patients is similar across years. Patients who experienced a stroke outside the study area (n=661), were referred from other districts (n=82), or with missing address information (n=47) were excluded from this study. Transient ischemic attack was excluded from this study due to the uncertainty of diagnosis for the stroke or its subtype (n=116).
The onset time of stroke was accurately prospectively recorded in all cases, and the median time between the last normal time and first abnormal time was regarded as the stroke onset in unclear cases. Cases for which the time between the last normal time and first abnormal time was >24 hours were excluded from the analysis (n=261). Finally, 2,313 cases were analyzed. The mean daily number of strokes was calculated during the study period of 3,652 days. The study design was approved by the Soonchunhyang University Hospital institutional review board before the investigations commenced (IRB No. 2016-04-019).
Stroke subtypes were assessed by a magnetic resonance imaging (MRI)-based algorithm10 with extensive workups including MRI/angiography, echocardiography, and Holter monitoring in all patients. Ischemic stroke subtypes were determined by the TOAST classification as follows: large-artery atherosclerosis (LAA), small-vessel occlusion (SVO), cardioembolic stroke (CE), stroke of undetermined etiology (SUE), and stroke of other determined etiology (SOE).11 Hemorrhagic stroke were classified into intracranial hemorrhage (ICH) and subarachnoid hemorrhage (SAH). Posttraumatic or nontraumatic subdural or epidural hemorrhages were not enrolled in this stroke registry.
Descriptive statistical methods were used to characterize the meteorological parameters. One-way analyses of variance (ANOVA) were applied to compare the number of cases among the temperature groups. The mean number of cases for each stroke subtype according to the maximum and minimum daily temperatures was analyzed by ANOVA and Duncan's post-hoc test. The cutoff for statistical significance was defined as p<0.05. All statistical analyses were performed using SPSS (version 18.0 for Windows, SPSS Inc., Chicago, IL, USA).
In total, 2,313 acute stroke cases whose residential addresses were within a 2-kilometer radius of the hospital were identified during the period: 1,643 ischemic strokes and 670 hemorrhagic strokes. The 1,643 ischemic stroke subjects comprised 675 with LAA (41.1%), 248 with SVO (15.1%), 213 with CE (13.0%), 342 with SUE (20.8%), and 49 with SOE (3.0%). The 670 hemorrhagic stroke subjects comprised 326 with ICH (48.7%) and 344 with SAH (51.3%). The meteorological parameters in Seoul between January 2005 and December 2014 are outlined in Table 1. The maximum and minimum daily temperatures were 17.1±10.8℃ (mean±SD) and 9.0±10.7℃, respectively. The mean number of total strokes daily was 0.63.
The mean numbers of stroke cases in each maximum daily temperature group are presented in Table 2. The mean number of stroke cases daily was 0.77 for >32.0℃ (n=124 days), 0.61 for 27.1℃ to 32.0℃ (n=720 days), 0.61 for 17.1℃ to 27.0℃ (n=1,138 days), 0.64 for 7.1℃ to 17.0℃ (n=829 days), 0.63 for -2.9℃ to 7.0℃ (n=731 days), and 0.82 for ≤-3.0℃ (n=110 days). The mean number of total strokes was maximal in the highest and lowest groups of maximum daily temperature (p=0.048). The mean number of ischemic strokes was maximal for the highest maximum daily temperature (p=0.040). The mean number of hemorrhagic strokes did not differ significantly among the maximum daily temperature groups (p=0.082).
The mean numbers of stroke cases in each minimum daily temperature group are presented in Table 3. The mean number of stroke cases daily was 0.75 for >25.0℃ (n=89 days), 0.64 for 19.1℃ to 25.0℃ (n=771 days), 0.60 for 9.1℃ to 19.0℃ (n=1,044 days), 0.64 for -0.9℃ to 9.0℃ (n=927), 0.62 for -10.9℃ to 1.0℃ (n=748 days), and 0.92 for ≤-11.0℃ (n=74 days). The mean numbers of total strokes and hemorrhagic strokes were maximal in the lowest minimum daily temperature group (p=0.020 and 0.020 in each). The mean number of ischemic strokes did not differ significantly among the minimum daily temperature groups (p=0.127).
For maximum and minimum daily temperatures, the mean numbers of stroke subtypes are presented in Table 4 and 5. The highest maximum daily temperature was associated with a significantly increased number of LAA cases (p=0.045), and the lowest maximum daily temperature was associated with significantly increased numbers of cases of SVO (p=0.013) and ICH (p=0.029). The distributions of the other subtypes were not significantly affected by the maximum daily temperature. The highest minimum daily temperature was also associated with a higher number of LAA cases (p=0.006), and the lowest minimum daily temperature was associated with a higher number of ICH cases (p=0.019). The other stroke subtypes showed no differences in the mean numbers of cases according to the minimum daily temperature.
The number of stroke cases did not differ significantly with the mean daily temperature, daily temperature range, day-to-day temperature differential, or daily average humidity (data not shown).
The possibility of a relationship between meteorological conditions and incidence of stroke has not yet been clarified. Despite the lack of strong evidence that weather conditions influence stroke incidence, many clinicians feel that meteorological conditions do impact the onset of stroke. Although there are some reports of no significant relationships between stroke and daily meteorological conditions,3712 other previous studies have found that cold temperature is associated with an increased risk of stroke occurrence.13141516
The present study found that the number of total stroke patients was significantly associated with the maximum daily temperature being less than -3℃ and with the minimum daily temperature being less than -11℃ in Seoul, Korea. The lowest daily temperature was associated with increased ischemic strokes and hemorrhagic strokes, especially SVO and ICH.
Several mechanisms could be responsible for the risk of stroke incidence being increased for the lowest daily temperature. The blood pressure and the levels of serum cholesterol, C-reactive protein, plasma fibrinogen, factor VII clotting activity in plasma, red blood cells, and platelet counts are reportedly higher at low temperatures.171819 The morning increase in the blood pressure is closely associated with the meteorological conditions.13 The increases in systolic blood pressure are also greater at lower temperatures.20 Considering the association of blood pressure and inflammatory markers with SVO2122 and ICH,2324 cold temperature could influence the occurrence of occlusion or rupture of cerebral small vessels.
On the other hand, the highest daily temperature was mainly associated with an increased number of ischemic stroke patients. A previous study suggested that exposure to heat is likely to cause dehydration, increasing the viscosity of the blood.25 Some experiments involving animal models have suggested that the blood supply to the central nervous system decreases during heat exposure.2627 These effects might not result in abnormalities in subjects without vascular disease, but they could increase the likelihood of thromboembolic episodes in patients with vascular disease. These hypotheses are consistent with our study finding that a larger number of cases of LAA was associated with the highest temperature group.
This study had several limitations and strengths. First, selection or information biases could have been present due to the clinical data being obtained retrospectively from a prospective acute stroke registry. Second, this study involved a single center, although this limitation was offset by the study period being longer and the inclusion of more subjects than in previous studies. Our results need external validation to confirm the association between meteorological parameters and incidence of stroke. However, because the same author managed all data of the stroke cases and meteorological parameters, the data obtained in this study should be accurate and consistent. Third, this study only counted the mean numbers of stroke patients, and did not consider vascular risk factors as covariates that could affect stroke incidence. Finally, the study covered a small geographical area, only including patients who resided within a 2-kilometer radius of our hospital. Seoul is one of the largest cities worldwide with one of the highest population densities. Therefore, covering a larger region might result in heterogeneity of the weather and environment characteristics for the sampled population. In addition, because there are many hospitals in Seoul, patients with acute stroke could visit other nearby hospitals. We therefore thought that conducting a single-center-based study covering a restricted region with similar meteorological conditions could be more suitable than a multicenter study for elucidating the effect of temperature on the occurrence of stroke.
In conclusion, the lowest and highest daily temperatures were associated with increased numbers of stroke patients in Seoul, Korea. The lowest temperature was associated with increases in both ischemic and hemorrhagic strokes, especially SVO and ICH, while the highest temperature was associated with increases in ischemic stroke, mainly LAA. Further studies are warranted to further elucidate the associations and pathophysiological mechanisms underlying the relationships between meteorological characteristics and the occurrence of stroke subtypes.
Figures and Tables
Table 1
Meteorological parameters in Seoul between January 2005 and December 2014 (n=3,652 days)

Table 2
Mean numbers of stroke patients according to maximum daily temperature groups
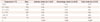
Table 3
Mean numbers of stroke patients according to minimum daily temperature groups
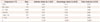
Table 4
Mean numbers of stroke subtypes according to maximum daily temperature groups

Table 5
Mean numbers of stroke subtypes according to minimum daily temperature groups

Acknowledgements
This study was supported by 1) the Soonchunhyang University Research Fund and 2) a grant of the Korea Healthcare technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI10C2020).
References
1. Kim JS. Stroke becomes the 3rd important cause of death in Korea; is it a time to toast? J Stroke. 2014; 16:55–56.

2. Douglas AS, Russell D, Allan TM. Seasonal, regional and secular variations of cardiovascular and cerebrovascular mortality in New Zealand. Aust N Z J Med. 1990; 20:669–676.

3. Jimenez-Conde J, Ois A, Gomis M, Rodriguez-Campello A, Cuadrado-Godia E, Subirana I, et al. Weather as a trigger of stroke. Daily meteorological factors and incidence of stroke subtypes. Cerebrovasc Dis. 2008; 26:348–354.
4. Miah AH, Sutradhar SR, Ahmed S, Bhattacharjee M, Alam MK, Bari MA, et al. Seasonal variation in types of stroke and its common risk factors. Mymensingh Med J. 2012; 21:13–20.
5. Ricci S, Celani MG, Vitali R, La Rosa F, Righetti E, Duca E. Diurnal and seasonal variations in the occurrence of stroke: a community-based study. Neuroepidemiology. 1992; 11:59–64.

6. Wang Y, Levi CR, Attia JR, D'Este CA, Spratt N, Fisher J. Seasonal variation in stroke in the Hunter Region, Australia: a 5-year hospital-based study, 1995-2000. Stroke. 2003; 34:1144–1150.

8. Rothwell PM, Wroe SJ, Slattery J, Warlow CP. Is stroke incidence related to season or temperature? The Oxfordshire Community Stroke Project. Lancet. 1996; 347:934–936.
9. Han MH, Yi HJ, Kim YS, Kim YS. Effect of seasonal and monthly variation in weather and air pollution factors on stroke incidence in Seoul, Korea. Stroke. 2015; 46:927–935.

10. Ko Y, Lee S, Chung JW, Han MK, Park JM, Kang K, et al. MRI-based algorithm for acute ischemic stroke subtype classification. J Stroke. 2014; 16:161–172.

11. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.

12. Cowperthwaite MC, Burnett MG. An analysis of admissions from 155 United States hospitals to determine the influence of weather on stroke incidence. J Clin Neurosci. 2011; 18:618–623.

13. Ohshige K, Hori Y, Tochikubo O, Sugiyama M. Influence of weather on emergency transport events coded as stroke: population-based study in Japan. Int J Biometeorol. 2006; 50:305–311.

14. Feigin VL, Nikitin YP, Bots ML, Vinogradova TE, Grobbee DE. A population-based study of the associations of stroke occurrence with weather parameters in Siberia, Russia (1982-92). Eur J Neurol. 2000; 7:171–178.

15. Low RB, Bielory L, Qureshi AI, Dunn V, Stuhlmiller DF, Dickey DA. The relation of stroke admissions to recent weather, airborne allergens, air pollution, seasons, upper respiratory infections, and asthma incidence, September 11, 2001, and day of the week. Stroke. 2006; 37:951–957.

16. Hong YC, Rha JH, Lee JT, Ha EH, Kwon HJ, Kim H. Ischemic stroke associated with decrease in temperature. Epidemiology. 2003; 14:473–478.

17. Woodhouse PR, Khaw KT, Plummer M, Foley A, Meade TW. Seasonal variations of plasma fibrinogen and factor VII activity in the elderly: winter infections and death from cardiovascular disease. Lancet. 1994; 343:435–439.

18. Keatinge WR, Coleshaw SR, Easton JC, Cotter F, Mattock MB, Chelliah R. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am J Med. 1986; 81:795–800.

19. Gordon DJ, Hyde J, Trost DC, Whaley FS, Hannan PJ, Jacobs DR, et al. Cyclic seasonal variation in plasma lipid and lipoprotein levels: the Lipid Research Clinics Coronary Primary Prevention Trial Placebo Group. J Clin Epidemiol. 1988; 41:679–689.

20. Otsuki T, Ishii N. Association between blood pressure changes during self-paced outdoor walking and air temperature. Clin Physiol Funct Imaging. 2015; 07. 25. [Epub]. DOI: 10.1111/cpf.12280.

21. Elkind MS, Luna JM, McClure LA, Zhang Y, Coffey CS, Roldan A, et al. C-reactive protein as a prognostic marker after lacunar stroke: levels of inflammatory markers in the treatment of stroke study. Stroke. 2014; 45:707–716.
22. Elkind MS, Luna JM, Coffey CS, McClure LA, Liu KM, Spitalnik S, et al. The Levels of Inflammatory Markers in the Treatment of Stroke study (LIMITS): inflammatory biomarkers as risk predictors after lacunar stroke. Int J Stroke. 2010; 5:117–125.

23. Sturgeon JD, Folsom AR, Longstreth WT Jr, Shahar E, Rosamond WD, Cushman M. Hemostatic and inflammatory risk factors for intracerebral hemorrhage in a pooled cohort. Stroke. 2008; 39:2268–2273.

24. Gong C, Hoff JT, Keep RF. Acute inflammatory reaction following experimental intracerebral hemorrhage in rat. Brain Res. 2000; 871:57–65.

25. Berginer VM, Goldsmith J, Batz U, Vardi H, Shapiro Y. Clustering of strokes in association with meteorologic factors in the Negev Desert of Israel: 1981-1983. Stroke. 1989; 20:65–69.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download