Abstract
Background and Purpose
This study analyzed the number of patients with ischemic strokes recorded in the Austrian Stroke-Unit Registry with the aim of projecting this number from 2012 to 2075 and to highlight that the Austrian health system will face a dramatic increase in older patients within the next few decades.
Methods
Current demographic information was obtained from EUROSTAT, and information on age- and sex-stratified 1-year incidence rates of ischemic stroke were obtained from the Austrian Stroke-Unit Registry. Sensitivity analysis was performed by analyzing the projections based on predicted ageing, main, and growth population scenarios, and with stratification by age and gender.
Results
The total number of ischemic strokes recorded in the Austrian Stroke-Unit Registry was 8,690 in 2012 and is expected to increase to 15,826, 15,626, or 18,134 in 2075 according to the ageing, main, and growth scenarios, respectively. The corresponding numbers of patients are projected to increase or decrease within different age strata as follows (100%=number of registered ischemic strokes in 2012): 0–40 years, 100%/99% (males/females); 40–50 years, 83%/83%; 50–60 years, 98%/97%; 60–70 years, 126%/119%; 70–80 years, 159%/139%; 80–90 years, 307%/199%; and 90+ years, 894%/413%.
Conclusions
The ageing population in Austria will result in the number of patients increasing considerably from 2012 to 2075, to 182%, 180%, or 208% (relative to 100% in 2012) according to the ageing, main, and growth scenarios, respectively; the corresponding value among those aged 80+ years is 315%, 290%, or 347%. These figures demonstrated the importance of improving primary preventive measures. The results of this study should provide a basis for discussions among health-care professionals and economists to face the future large financial burden of ischemic stroke on the Austrian health system.
Stroke is the third leading cause of death and the main cause of long-term disability in Western societies.1 About 15 million people worldwide suffer from stroke annually.2 The increasing longevity of the populations in developed countries will cause far-reaching socioeconomic and social problems and seriously affect their health-care systems. This will result in the burden of diseases with an age-dependent incidence increasing markedly over the next few decades worldwide. In the 27 European Union (EU) countries, the total annual cost of stroke was estimated to be €27 billion as at 2009,3 with €18.5 billion (68.5%) for direct costs and €8.5 billion (31.5%) for indirect costs.4 An additional €11.1 billion was estimated as the cost of informal care.4 Including informal care in the total amount changes the percentage contributions of direct, indirect, and informal care costs to 48.6%, 22.3%, and 29.1%, respectively.3 However, the cost per stroke patient in Austria is difficult to estimate. The following estimates are given in EURO purchasing power parity (PPP) which is an international measure to be able to compare economic data between countries by adjusting for the relative purchasing power in the respective countries. These estimates range from EUR PPP 9,634 in 20105 to EUR PPP 20,784 in 2004.6
Population projections predict a considerable increase in the older population throughout Europe. From 2012 to 2075 the number of residents older than 75 years will increase by 70%, 75%, 91%, 104%, 153%, 161%, and 162% in Germany, Spain, Italy, France, the UK, Denmark, and Austria, respectively.7 The estimated population pyramids in Austria in 2012, 2050, and 2075 stratified by sex are illustrated in Fig. 1.
The elderly population throughout the EU is predicted to increase by 103% overall.7 This huge ageing of the population will have various consequences for the EU's health and social systems that must be addressed, especially for diseases with age-dependent incidence rates such as stroke.
Several studies have clearly demonstrated that the incidence of ischemic stroke increases with age: about 50% of strokes occur in people older than 70 years and nearly 25% of them are in people older than 85 years.8910 Combining the age dependency of stroke with the expected demographic developments stimulated us to formulate the following research question: "How will the numbers of registered patients with ischemic stroke change within the next few decades, especially with respect to their sex and age?" Hence, it is the aim of this study was to project the number of ischemic strokes recorded in the Austrian Stroke-Unit Registry from 2012 to 2075.
Two different data sources and one assumption were used to project the total numbers of patients with registered ischemic stroke into the next few decades. The information in these data sources is freely available in the public domain, and hence no informed consent, trial registration, or ethics committee approval was necessary.
Current demographic information on the number of Austrian inhabitants and population projections from 2012 to 2075 was obtained from EUROSTAT,7 which is one of the Directorates-General of the European Commission. Lower and upper bounds for the projections were derived from three scenarios: 1) an ageing scenario that reflects low fertility, low immigration, and high life expectancy (lower bound), 2) the main (and most likely) scenario that reflects mean fertility, mean life expectancy, and mean immigration, and 3) the growth scenario that reflects high fertility, high life expectancy, and high immigration (upper bound).
Our scenarios were based on the assumption that the incidence of ischemic stroke would remain constant over time, meaning that the analysis ignored factors that might increase or decrease the incidence, such as cardiovascular diseases, hypercholesterolemia, nicotine abuse, alcohol abuse, and malignant tumors. All estimations and projections were calculated for the ageing, main, and growth scenarios, and stratified by age (into 0–40, 40–50, 50–60, 60–70, 70–80, 80–90, and 90+ years) and sex.
The population of Austria was 8.4 million in 2012, and this is estimated to increase to 8.0 million, 9.4 million, and 11.6 million in 2075 according to the ageing, main, and growth scenarios, respectively. The total number of registered ischemic strokes was 8,690 in 2012, and is expected to increase to 15,826, 15,626, or 18,134 in 2075 according to the three scenarios. Fig. 2 provides a detailed overview of the projected numbers of patients with ischemic stroke between 2012 and 2075.
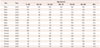
Within different age strata, the corresponding number of patients are projected to increase or decrease as follows (100%=number of patients in 2012): 0–40 years, 100%/99% (males/females); 40–50 years, 83%/83%; 50–60 years, 98%/97%; 60–70 years, 126%/119%; 70–80 years, 159%/139%; 80–90 years, 307%/199%; and 90+ years: 894%/413%. A detailed overview of these changes is presented in Table 1.
The total number of patients registered with ischemic stroke in Austria will increase to 180%, 208%, or 182% from 2012 to 2075 (100%=number of patients in 2012) according to the ageing, main, and growth scenarios, respectively; the corresponding value is 240%, 278%, or 250% in patients aged 80–90 years, and 537%, 683%, or 637% in patients aged 90+ years. These findings indicate that the perioperative costs associated with ischemic stroke due to co-morbidity, perioperative complications, and prolonged postoperative rehabilitation will increase markedly during the forthcoming decades.
The ageing population means that the patient capacity of hospitals and rehabilitation institutions will have to expand markedly or their admission strategies for patients will have to change over the coming decades. Since stroke is usually accompanied by long-term disability, the need for long life care will also increase along with the demand for places in care homes. Furthermore, evidence-based acute and postdischarge procedures are needed that aim at reducing the number of severely disabled stroke patients and eventually to further reduce costs. Such measures have already been studied in randomized controlled trials; for example, intravenous thrombolysis is highly efficacious as a treatment for acute ischemic stroke within the first 3 hours.12 Furthermore, recently reported thrombectomy studies have confirmed the efficacy of neurointervention for recanalization in strokes caused by occlusion of the large cerebral arteries.1314 A broad availability of specialized stroke centers in Austria with full ("24/7") availability of neurointerventions will lessen the burden of ischemic stroke in Austria and help to reduce health-care expenditure.
The increasing number of patients with ischemic stroke will have a major economic burden and effects on health policies in Austria. The results of this study can be used to guide discussions aimed at estimating future costs in the Austrian health system for health-care professionals.
The strengths of this study can be summarized as follows:
- This is the first study to estimate the number of patients with ischemic stroke in Austria during 2012–2075.
- Our projections are based on a well-established stroke register using data collection and variables defined according to best-validated definitions. However, most previous studies are limited to patient recruitment from only one or a few hospitals, which may limit the ability to generalize their results to the national level.
- Sensitivity analysis of the projections was performed to provide realistic lower and upper bounds for the projections.
This study was subject to the following limitations:
- Although the population projections are based on the official population projections of EUROSTAT, such projections are not 100% reliable.
- We assumed that the incidence of stroke is stable over time, based on data from 2009, 2010, 2011, and 2012 indicating incidence rates of 0.09%, 0.11%, 0.11%, and 0.10%. However, it is possible that the 1-year stroke incidence will decrease or increase due to factors such as changes in certain risk factors such as smoking, cardiovascular diseases, hypercholesterolemia, nicotine abuse, alcohol abuse, and malignant tumors that can increase the incidence of stroke. Moreover, there are other factors such as primary prevention measures (e.g., adequate treatment of hypertension, atrial fibrillation, and hypercholesterolemia) and further risk-factor controls that can reduce the incidence of stroke.15 Such a lowering trend has already been detected regarding patients with myocardial ischemia,9 although analogous findings have not been reported regarding stroke prevalence.10 It is for these reasons that we assumed that the incidence of stroke was stable over time.
Political action is required in light of the present high numbers and the expectation of greatly increasing numbers of patients with ischemic stroke. The funding of stroke research must be increased, and continued research into the cost of stroke and related diseases not included in the present study is also warranted.
The total number of registered ischemic strokes will dramatically increase within the next decades due to the ageing population in Austria. These changes will increase the burden on health-care systems. Improvements in effective primary prevention measures, evidence-based acute treatments including neurointervention methods, and postdischarge treatments can reduce the mortality and long-term disability rates associated with stroke and thereby lessen the social and health-care burdens of stroke in the future.
Figures and Tables
 | Fig. 1Population pyramids for Austria in 2012, 2050, and 2075 stratified by sex according to the main scenario.7 |
 | Fig. 2Projected numbers of patients with registered ischemic stroke in Austria between 2012 and 2075 stratified by age and sex. The ageing, main (most likely), and growth scenarios are based on population projections of EUROSTAT and the Austrian Stroke-Unit Registry. Main scenario: mean fertility, mean life expectancy, and mean immigration, middle lines; Growth scenatio: high fertility, high life expectancy, and high immigration, upper lines; Ageing scenario: low fertility, high life expectancy, and low immigration; lower lines. |
Table 1
Projected changes (percentage values, normalized to 100% in 2012) in ischemic strokes recorded in the Austrian Stroke-Unit Registry during 2012–2075 based on the main scenario of population growth
References
1. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006; 367:1747–1757.

2. WHO publishes definitive atlas on global heart disease and stroke epidemic. Indian J Med Sc. 2004; 58:405–406.
4. Allender S, Scarborough P, Peto V, Rayner M, Leal J, Luengo-Fernandez R, et al. European Cardiovascular Disease Statistics 2008. Brussels: European Heart Network;2008.
5. Gustavsson A, Svensson M, Jacobi F, Allgulander C, Alonso J, Beghi E, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011; 21:718–779.

6. Andlin-Sobocki P, Jönsson B, Wittchen HU, Olesen J. Cost of disorders of the brain in Europe. Eur J Neurol. 2005; 12:Suppl 1. 1–27.

8. Broussalis E, Killer M, McCoy M, Harrer A, Trinka E, Kraus J. Current therapies in ischemic stroke. Part A. Recent developments in acute stroke treatment and in stroke prevention. Drug Discov Today. 2012; 17:296–309.

9. Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, et al. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008; 117:e25–e146.
10. Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003; 2:43–53.

11. Hofer C, Kiechl S, Lang W. [The Austrian Stroke-Unit-Registry]. Wien Med Wochenschr. 2008; 158:411–417.
12. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329.

13. Berkhemer OA, Majoie CB, Dippel DW. MR CLEAN Investigators. Endovascular therapy for ischemic stroke. N Engl J Med. 2015; 372:2363.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download