Abstract
Background and Purpose
Acute disseminated encephalomyelitis (ADEM) is an inflammatory demyelinating disorder that predominantly affects children. Previous studies have mostly involved children in Western developed countries.
Methods
This study retrospectively reviewed the clinical profiles of ADEM in adult Chinese patients.
Results
ADEM occurred during summer and autumn in about two-thirds of the 42 included patients. Prior infection was found in five patients and no preimmunization was recorded. The most frequent clinical presentations were alterations in consciousness (79%) and behavior changes (69%), followed by motor deficits (64%) and fever (50%). About one-quarter (26%) of the patients showed positive results for oligoclonal bands, and about half of them exhibited increases in the IgG index and 24-hour IgG synthesis rate. Magnetic resonance imaging showed white- and gray-matter lesions in 83% and 23% of the patients, respectively. Steroids were the main treatment, and full recovery occurred in 62% of the patients, with residual focal neurological deficits recorded in a few patients. After a mean follow-up period of 3.4 years, two patients exhibited recurrence and one patient exhibited a multiphasic course. One patient was diagnosed with multiple sclerosis (MS).
Conclusions
With the exception of the seasonal distribution pattern and prior vaccine rate, the clinical profiles of ADEM in adult Chinese patients are similar to those in pediatric populations. No specific markers are available for distinguishing ADEM from MS at the initial presentation. Careful clinical evaluations, cerebrospinal fluid measurements, and neuroradiological examinations with long-term follow-up will aid the correct diagnosis of ADEM.
Acute disseminated encephalomyelitis (ADEM) is an inflammatory demyelinating disorder of the central nervous system. It is normally preceded by viral infections or vaccinations and it is more common in children than in adults.1 Since there are no specific biological markers for ADEM, it is diagnosed based on a combination of clinical features, cerebrospinal fluid (CSF) measurements, and neuroradiological findings. In contrast to multiple sclerosis (MS), which is characterized by relapse and remission, ADEM usually appears as a monophasic process. Although rare, some patients presenting with recurrence or a multiphasic course have been reported, indicating diagnostic difficulties.23 Previous studies have mostly involved pediatric populations,4 with relatively few studies involving adult patients.5 Here we present a series of 42 adult patients in Zhengzhou City, China with the purpose of identifying the clinical manifestations and laboratory and neuroimaging features of this disease in an adult population, and presenting the short-term outcomes of these patients for comparison with other studies.
The patients in this study were selected based on medical records kept at Henan Provincial People's Hospital of Zhengzhou University in Henan Province, People's Republic of China. Patients who were diagnosed with ADEM between January 2003 and December 2013 were reviewed retrospectively. Approval for the study was obtained from the human research ethics committees of Zhengzhou University.
Clinical records were carefully reviewed by experienced investigators (H.-Q.Y. and W.-M.Y.) in order to ensure accurate diagnoses. Demographic data, the results of clinical presentations, physical examinations, and laboratory studies, neuroimaging findings, and treatment and clinical outcomes were extracted from medical records using a standardized form.
For laboratory examinations, microbiological data were extracted from laboratory reports and progress notes in the individual records. To ascertain the diagnosis of a clinical infectious condition, the patient history, medical history, and results of physical examinations and microbiological tests were carefully reviewed. For neuroimmunology examinations, the results for oligoclonal bands (OCB) were defined as positive when they were present in CSF but absent in serum. The IgG index and 24-hour IgG synthesis rate were also measured in the CSF. Brain magnetic resonance imaging (MRI) was carried out using a uniform protocol that included the acquisition of axial T1-weighted, T2-weighted, sagittal T1-weighted, and fluid-attenuated inversion recovery (FLAIR) images. Spinal cord MRI was performed when necessary. Contrast images were obtained in some patients after administering a single dose of gadolinium. During hospitalization in the acute phase, short-term MRI was repeated when the patient exhibited clinical deterioration. MRI was also repeated whenever possible if the patient exhibited clinical improvement. A senior neuroradiologist (Y.-L.L.) who was blinded to the study design reviewed the MRI findings.
Patients who met the following criteria were included in this study:6 1) polysymptomatic, acute, or subacute onset in the clinical presentation, 2) presence of encephalopathy defined by either alterations in consciousness or behavior changes, 3) focal or multifocal lesions in MRI, predominantly involving white matter, and 4) no MRI evidence of previous destructive white-matter changes.
The following patients were excluded from the investigations performed in the present study: 1) younger than 18 years, 2) suspicious diagnosis of ADEM, 3) no CSF examination, 4) no cranial MRI scan, 5) incomplete clinical data, or 6) loss to follow-up.
An appointment for the follow-up was made prior to discharge from hospital. At the follow-up, any neurological symptoms that had developed during the intervening period were documented, and a clinical evaluation was performed. Follow-up MRI was carried out in some cases. Complete recovery was defined as total resolution of the initial clinical symptoms.
Various types of relapse were defined as described below.6
If a relapse occurred within 4 weeks of tapering steroid treatment or within the first 3 months from the initial event, this early relapse was considered to be temporally related to the same acute monophasic condition. Treatment-related fluctuations were not considered a relapse.
Recurrent ADEM was defined as a new ADEM event with recurrence of the initial symptoms and signs at least 3 months after the first ADEM event and at least 4 weeks after completing steroid therapy, and showing the same clinical presentation and affecting the same areas on MRI as the initial ADEM episode.
Multiphasic ADEM was defined as ADEM followed by a new clinical event also meeting the criteria for ADEM, but involving new anatomic areas of the CNS as confirmed by the medical history, neurological examination, and neuroimaging. The subsequent event must have occurred at least 3 months after the initial ADEM attack and at least 4 weeks after completing steroid therapy.
A diagnosis of MS was made when two or more demyelinating episodes subsequently occurred at least 30 days after the initial attack, fulfilling the 2005 McDonald criteria7 for dissemination in time and space.
Of the 82 potential patients initially diagnosed with ADEM, 42 were included in this study after careful clinical evaluation. The 40 patients were excluded for the following reasons: younger than 18 years (n=11), suspicious diagnosis (n=7), incomplete clinical data (n=13), and loss to follow-up (n=9).
The 42 ADEM patients comprised 16 males and 26 females, giving a male:female ratio of approximately 1:1.6. The age at presentation was 33.5±8.6 years (mean±SD), and ranged from 18 to 66 years. About two-thirds (27/42) of patients were admitted in summer and autumn. No prior vaccinations were recorded. Four patients were identified as having prior upper respiratory tract infection, and one had a digestive tract infection. The mean duration of symptoms before admission was 9.6 days (range, 2–40 days), the mean time interval from initial neurological symptom presentation to maximum was 6.3 days (range, 1–15 days), and the mean length of hospital stay was 14.1 days (range, 1–34 days).
Thirty-three patients (79%) presented with alternations in consciousness such as somnolence, lethargy, and coma, while 69% of patients exhibited behavior changes such as confusion, excessive irritability, and impaired orientation. Twenty-seven patients (64%) showed motor deficits including hemiplegia, paraplegia, or single-limb weakness. Half of the patients presented with fever, which lasted from 5 to 26 days. Sensory deficits and cranial-nerve impairment was observed in 42% of patients. Seizures were recorded in nine patients (21%), with one developing status epileptics. Spinal cord involvement was reported in 20 patients (48%); the frequencies of other presenting symptoms are listed in Table 1.
Corticosteroid treatment was applied in 35 patients (83%), and immunoglobulin was injected intravenously in 7 patients. About 62% of these patients experienced full recovery, and residual focal neurological deficits occurred in five patients. The neurological sequelae were hemiparesis in two patients, and mental handicap, numbness, and visual impairment in one patient each.
Infection complication was reported in 10 patients, with the diagnoses confirmed by sputum smear and serum examinations. These infections involved the respiratory and urinary tracts in eight and two patients, respectively.
CSF findings were normal in 13 patients. Increased protein levels were recorded in 20 patients (48%), with a highest concentration of 1.39 g/L. Eighteen patients (43%) were found to have elevated levels of white blood cells, with lymphocytes being the predominant cell type. The glucose level in CSF varied from 2.16 to 7.58 mmol/L, with mean of 4.2 mmol/L. Eleven patients (26%) showed positive OCB results, while 21 patients (50%) showed an increased IgG index and 24 patients (57%) showed an increased 24-hour IgG synthesis rate. The IgG index indicated disturbance of the blood-brain barrier in 19 patients (45%). Mean serum and CSF levels of myelin basic protein and neuron-specific enolase were within the normal ranges.
Thirty-five patients (83%) presented with white-matter lesions, which were distributed in the frontal (48%), temporal (31%), parietal (24%), and occipital (24%) lobes. The lesions are frequently identified using T2-weighted and FLAIR sequences as large and patchy lesions with poorly defined margins and increased signal intensities. Most of patients showed multiple lesions and they were usually distributed asymmetrically, with variable extension to the subcortical white matter. Other frequently involved areas are listed in Table 2, and representative MRI findings are shown in Fig. 1.
The administration of gadolinium enhanced the T1-weighted sequences in 9 of 20 patients (45%), with different patterns of enhancement. The lesions were completely enhanced in five patients and partially enhanced in the other four patients. Patchy, nodular, ring-shaped, and linear enhancement types were observed in seven, six, six, and five patients, respectively.
A follow-up MRI scan was performed in 15 patients, which revealed 6 patients with completely normal findings and 9 patients with only partially resolved lesions.
The mean follow-up period was 3.4 years (range, 0.8–5.6 years), and two patients exhibited recurrence and one patient exhibited a multiphasic course. One patient was finally diagnosed with MS.
One of the patients with recurrence initially presented with somnolence and hemiplegia in the left limbs as a result of lesions in the brainstem and right temporal and occipital lobes. Six months later he presented with hemiplegia and hypoesthesia, with MRI indicating that the lesions were in the same areas as when he was first admitted.
The other patient with recurrence initially presented with fever, disorientation, urinary and fecal incontinence, and left hemiparesis. MRI showed multiple lesions in the cerebellum and the frontal and parietal lobes. Thirteen months later she visited the emergency department with lethargy, left hemiparesis, and urinary incontinence. Repeated MRI again showed multiple lesions in the cerebellum and the frontal and parietal lobes.
The patient with the multiphasic form of ADEM initially presented with fever, headache, somnolence, disorientation, and urinary incontinence. MRI showed multiple lesions of various sizes in the cerebellum, brainstem, cerebral cortex, subcortex, and upper-cervical spinal cord. The OCB results were positive. Four months later, just 40 days after discontinuing steroids therapy, she presented with ataxia, diplopia, and vision loss in the right eye. At this presentation she was slightly lethargic, confused, and denied symptoms of dysautonomia. MRI showed new lesions in the temporal and occipital lobes bilaterally. Both the size and distribution of these lesions differed from those present at the first attack. The OCB results were negative, and neuromyelitis optica (NMO)/IgG measurements were negative. She fulfilled the definitions of multiphasic disseminated encephalomyelitis.
A 34-year-old woman presented with slurred speech, dysphagia, salivation, and unresponsiveness. She also showed positive OCB results and increased intrathecal IgG synthesis. MRI showed multiple lesions in white matter of the frontal and temporal lobes bilaterally. Nine months later she presented with unilateral optic neuritis. Repeated MRI showed multiple lesions with enhancement. A CSF examination showed positive OCB results. The diagnosis of MS was suspected and she gradually recovered after the administration of steroids. At a 2-year follow-up she was relapse-free.
ADEM appears to be more common in children, and most previous studies have involved pediatric populations. Although some researchers have reported no gender predominance,28 female predominance was found in two pediatric studies,49 with male:female ratios of 1:1.2 and 1:1.6. In our series of 42 ADEM adult patients the male:female ratio was 1:1.6, similar to the previous results in adults5 and pediatric patients.49 The patients here predominantly exhibited ADEM during the summer and autumn months, as opposed to previous reports of its occurrence in children predominating in winter and spring.89 We speculate that this difference is related to a high rate of prior vaccinations in pediatric patients, since some regional cases may be linked to specific vaccines, and no preceding vaccinations or prior immunization were recorded in our adult patients. The rate of prior infection in the present study was much lower than in a pediatric population.10 This reinforces the concept that infection or immunization is not a prerequisite for the diagnosis of ADEM, especially in adult populations.
The presence of encephalopathy was one of the inclusion criteria applied in this study,6 which resulted in high rates of alternations in consciousness and behavior changes being recorded in the patients (78% and 69%, respectively). Other frequent symptoms in this population were motor deficits (64%) and fever (50%). The reported frequency of fever is high in pediatric populations, ranging from 38.5% to 52%,91112 and lower in adults.6 We also found spinal cord involvement and seizures in 47% and 22% of the included patients, respectively; these frequencies are very similar to those reported previously in pediatric patients,1112 whereas incidence rates of 15% and 4%, respectively, were found in an adult population.5 Besides differences in geographical characteristics and enrollment criteria, we found no reasons for these discrepancies in clinical profiles.
Eleven patients (26%) recorded positive OCB results in the present study. This proportion has varied greatly between different research groups, with Lu et al.13 and Schwarz et al.6 reporting rates of 12% and 56%, respectively, in adult patients, and other researchers finding rates ranging from 0% to 29% in pediatric patients.24911 Some researchers have found positive OCB results in as many as 92% of included MS patients.14 An elevated IgG index and the presence of OCB were observed more often in children who developed MS.15 About half of our patients showed an increased IgG index and 24-hour IgG synthesis rate, but its significance in ADEM diagnosis and prognoses still needs to be clarified since there are relatively few data available on ADEM. Positive OCB results and cerebral white-matter lesions at the initial presentation in ADEM suggest a higher risk of developing MSm.16 It is also necessary to clarify the circumstances in which the presence of OCB cannot be used to discriminate ADEM from MS.2513 The reported risk of developing MS after ADEM has varied widely, fro 0%4 to 28%17 and even 35%.5 There is currently no immunological marker for the development of MS from initial demyelinating events.
MRI is extremely useful in both ADEM diagnosis and the differential diagnosis of ADEM and MS. Thirty-three patients (92%) in the present study exhibited bilateral asymmetric lesions. These radiological features are similar to previous reports.4511 Two patients (6%) presented with periventricular lesions, which are difficult to distinguish from MS. Schwarz et al.5 reported periventricular involvement in 54% and 86% of ADEM and MS cases, respectively. To solve this problem, a MRI criterion18 capable of distinguishing ADEM from MS at onset was applied in the present study. It is claimed that any two of the following features supports an MS diagnosis: 1) absence of a diffuse bilateral lesion pattern, 2) presence black holes, and 3) presence of two or more periventricular lesions. This two-feature criterion is most useful for differentiating a first attack of MS from monophasic ADEM with 81% sensitivity and 95% specificity.19
While corpus callosum involvement is less common in ADEM,20 this was present in four of our patients (13%). Liu et al.21 clinically analyzed 12 ADEM patients with corpus callosum lesions, and found an adult male predominance and intracranial infective signs in CSF; all of the four patients in the present study were also male. It has also been found that corpus callosum lesions appear to be associated with a higher risk of clinical conversion to MS in the short term.22 Schwarz et al.6 reported corpus callosum involvement in 23% of cases, but the outcomes of those patients were not reported. It seems that corpus callosum involvement in ADEM may not be rare, and future studies should attempt to confirm the role of the corpus callosum in ADEM pathogenesis.
Relapse in ADEM has often been confused with MS in previous studies. There are no practical diagnostic criteria for differentiating a first episode of MS from monophasic ADEM. For example, 4 cases of relapse11 and 10 cases of biphasic disease4 in pediatric ADEM could not be definitively differentiated from MS. A patient who has experienced more than three attacks of CNS demyelization is difficult to distinguish from MS.3 We reported one patient diagnosed finally with MS, and this prevalence is much lower than in another study involving adults, which found that 35% of patients initially diagnosed ADEM were finally diagnosed with definite MS.5 A careful clinical evaluation and MRI features18 may help in establishing a correct diagnosis. For example, gray matter is often involved in ADEM but rarely in MS. In addition, encephalopathy is seldom seen in MS but is necessary for the definition of ADEM. Moreover, MS is characterized by disease relapse and incomplete remission, and usually has stepwise progressive outcomes, while ADEM often shows a relative good recovery in the long term even though residue deficits may exist.
This study was subject to some limitations. These include the relatively small number of patients and the short follow-up period. Nine patients who were lost to follow-up were excluded from the study. It is quite common for such patients to visit other hospitals if they experience further neurological events, which may at least partially explain why the MS conversion rate was lower in the present study. There is also a possibility of other diagnoses and an unknown future prognosis. Since we did not measure AQP-4 antibodies, which is a specific test for NMO spectrum disorder, the possibility of this disorder in our cohort cannot be excluded.23
Collectively, except for the seasonal distribution pattern, prior vaccine rate, and increases in IgG index and 24-hour IgG synthesis rate in half of our patients, the clinical profiles of ADEM in adult Chinese patients are similar to those in pediatric populations in Western countries. The pathogenesis of ADEM is not clear and it shares many similarities with MS. Since the prognoses of these two conditions are dramatically different, it is particularly important to be able to differentiate them. However, no specific biomarker is yet available for definitively distinguishing ADEM from MS, and so careful clinical evaluations, CSF measurements, repeated MRI scanning, and long-term follow-up (spanning years or even decades) may be necessary to differentiate ADEM from MS.
Figures and Tables
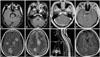 | Fig. 1Representative MRI findings in ADEM patients. The figure shows various lesions involving the brainstem (A), brachium pontis (B), cerebellum (C), frontal, temporal, and parietal lobes (D-F), and spinal cord (G) in ADEM patients. The inset picture in the sagittal view of the spinal cord lesion (G) shows an axial sequence. FLAIR (A, B, and E) and axial T2-weighted (F and G) images show lesions of various sizes. Nodular, patchy (C and D), and ring-shaped (H) enhancement types were observed following the administration of gadolinium. ADEM: acute disseminated encephalomyelitis. |
Table 1
Frequencies of presenting clinical features in ADEM

Table 2
Locations of MRI findings in ADEM patients

Acknowledgements
This study was supported by grants from Henan Medical Science and Technology Program (201203130), Key Science and Technology Project of Henan Province (112102310684).
References
1. Tenembaum S, Chitnis T, Ness J, Hahn JS;. Acute disseminated encephalomyelitis. Neurology. 2007; 68:16 Suppl 2. S23–S36.

2. Dale RC, de Sousa C, Chong WK, Cox TC, Harding B, Neville BG. Acute disseminated encephalomyelitis, multiphasic disseminated encephalomyelitis and multiple sclerosis in children. Brain. 2000; 123(Pt 12):2407–2422.

3. Chen S, Wu A, Zhang B, Li J, Zhang L, Lin Y, et al. A case of exacerbated multiphasic disseminated encephalomyelitis after interferon β treatment. J Neurol Sci. 2013; 325:176–179.

4. Tenembaum S, Chamoles N, Fejerman N. Acute disseminated encephalomyelitis: a long-term follow-up study of 84 pediatric patients. Neurology. 2002; 59:1224–1231.

5. Schwarz S, Mohr A, Knauth M, Wildemann B, Storch-Hagenlocher B. Acute disseminated encephalomyelitis: a follow-up study of 40 adult patients. Neurology. 2001; 56:1313–1318.

6. Krupp LB, Banwell B, Tenembaum S;. Consensus definitions proposed for pediatric multiple sclerosis and related disorders. Neurology. 2007; 68:16 Suppl 2. S7–S12.

7. Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol. 2005; 58:840–846.

8. Leake JA, Albani S, Kao AS, Senac MO, Billman GF, Nespeca MP, et al. Acute disseminated encephalomyelitis in childhood: epidemiologic, clinical and laboratory features. Pediatr Infect Dis J. 2004; 23:756–764.

9. Murthy SN, Faden HS, Cohen ME, Bakshi R. Acute disseminated encephalomyelitis in children. Pediatrics. 2002; 110(2 Pt 1):e21.

10. Idrissova ZhR, Boldyreva MN, Dekonenko EP, Malishev NA, Leontyeva IY, Martinenko IN, et al. Acute disseminated encephalomyelitis in children: clinical features and HLA-DR linkage. Eur J Neurol. 2003; 10:537–546.

11. Hynson JL, Kornberg AJ, Coleman LT, Shield L, Harvey AS, Kean MJ. Clinical and neuroradiologic features of acute disseminated encephalomyelitis in children. Neurology. 2001; 56:1308–1312.

12. Likasitwattanakul S, Chiewvit P. Acute disseminated encephalomyelitis in Siriraj Hospital: clinical manifestations and short-term outcome. J Med Assoc Thai. 2012; 95:391–396.
13. Lu Z, Zhang B, Qiu W, Kang Z, Shen L, Long Y, et al. Comparative brain stem lesions on MRI of acute disseminated encephalomyelitis, neuromyelitis optica, and multiple sclerosis. PLoS One. 2011; 6:e22766.

14. Neuteboom RF, Boon M, Catsman Berrevoets CE, Vles JS, Gooskens RH, Stroink H, et al. Prognostic factors after a first attack of inflammatory CNS demyelination in children. Neurology. 2008; 71:967–973.

15. Pohl D, Rostasy K, Reiber H, Hanefeld F. CSF characteristics in early-onset multiple sclerosis. Neurology. 2004; 63:1966–1967.

16. Sharief MK, Thompson EJ. The predictive value of intrathecal immunoglobulin synthesis and magnetic resonance imaging in acute isolated syndromes for subsequent development of multiple sclerosis. Ann Neurol. 1991; 29:147–151.

17. Mikaeloff Y, Suissa S, Vallée L, Lubetzki C, Ponsot G, Confavreux C, et al. First episode of acute CNS inflammatory demyelination in childhood: prognostic factors for multiple sclerosis and disability. J Pediatr. 2004; 144:246–252.

18. Callen DJ, Shroff MM, Branson HM, Li DK, Lotze T, Stephens D, et al. Role of MRI in the differentiation of ADEM from MS in children. Neurology. 2009; 72:968–973.

19. Ketelslegers IA, Neuteboom RF, Boon M, Catsman-Berrevoets CE, Hintzen RQ;. A comparison of MRI criteria for diagnosing pediatric ADEM and MS. Neurology. 2010; 74:1412–1415.

21. Liu JG, Qiao WY, Dong QW, Zhang HL, Zheng KH, Qian HR, et al. [Clinical features and neuroimaging findings of 12 patients with acute disseminated encephalomyelitis involved in corpus callosum]. Zhonghua Yi Xue Za Zhi. 2012; 92:3036–3041.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download