Abstract
Background and Purpose
Methods
Results
Figures and Tables
Fig. 1
BRSS in PDOH and MSA-POH (5.04±0.66 ms/mm Hg vs. 4.78±0.64 ms/mm Hg; p value=0.54) was not different in the two disorders (A) but BRSVM-PIV from phase IV of VM in PDOH was significantly lesser than MSA-POH (0.03±0.07 ms/mm Hg vs. 2.86±2.39 ms/mm Hg; p value=0.004) (B) even though the BRSVM-PII from phase II of VM was not different in PDOH and MSA-POH (0.96±0.75 ms/mm Hg vs. 1.34±1.51 ms/mm Hg; p value= 0.76) (C). BRSS: spontaneous baroreflex sensitivity, BRSVM-PII: baroreflex sensitivity from phase II of Valsalva, BRSVM-PIV: baroreflex sensitivity from phase IV of Valsalva, MSA-POH: multiple-system atrophy of the Parkinsonian type with orthostatic hypotension, PDOH: Parkinson's disease patients with orthostatic hypotension.

Fig. 2
LF and HF indices of the heart rate variability in PDOH and MSA-POH are not different between the two disorders (1.78±0.21 ms2 vs. 1.67±0.14 ms2; p value=0.66 and 1.45±0.18 ms2 vs. 1.64±0.17 ms2; p value=0.47 respectively) (A and B) and the LF/HF ratio shows a higher trend in PDOH as compared to MSA-POH (2.36±1.06 vs. 1.77±1.97; p value=0.05) (C). HF: high frequency, HRV: heart rate variability, LF: low frequency, MSA-POH: multiple-system atrophy of the parkinsonian type, PDOH: Parkinson's disease patients with orthostatic hypotension.

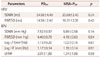
Table 1
Demographic data

Only male patients without the history of any co-morbid conditions were chosen for the procedure. Special care was taken to rule out patients of MSA-C and PD patients with severity of IV and V on the Hoehn and Yahr scale.
NIDDM: non insulin dependent diabetes mellitus, MSA-P: multiple-system atrophy of the parkinsonian type, OH: orthostatic hypotension, PD: Parkinson's disease.
Table 2
Patients of PDOH and MSA-POH did not differ in the time domain parameters of heart rate variability and time domain as well as frequency domain parameters of blood pressure variability
BPV: blood pressure variability, HF: high frequency, HRV: heart rate variability, LF: low frequency, MSA-POH: multiple-system atrophy of the Parkinsonian type with orthostatic hypotension, PDOH: Parkinson's disease patients with orthostatic hypotension, RMSSD: square root of the mean squared differences of successive NN intervals, SDNN: Standard Deviation of the NN interval.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download