Abstract
Background and Purpose
Childhood absence epilepsy (CAE) is one of the most common types of pediatric epilepsy. It is generally treated with ethosuximide (ESM), valproic acid (VPA), or lamotrigine (LTG), but the efficacy and adverse effects of these drugs remain controversial. This study compared initial therapy treatment outcomes, including VPA-LTG combination, and assessed clinical factors that may predict treatment response and prognosis.
Methods
Sixty-seven patients with typical CAE were retrospectively enrolled at the Korea University Medical Center. We reviewed patients' clinical characteristics, including age of seizure onset, seizure-free interval, duration of seizure-free period, freedom from treatment failure, breakthrough seizures frequency, and electroencephalogram (EEG) findings.
Results
The age at seizure onset was 7.9±2.7 years (mean±SD), and follow-up duration was 4.4±3.7 years. Initially, 22 children were treated with ESM (32.8%), 23 with VPA (34.3%), 14 with LTG (20.9%), and 8 with VPA-LTG combination (11.9%). After 48 months of therapy, the rate of freedom from treatment failure was significantly higher for the VPA-LTG combination therapy than in the three monotherapy groups (p=0.012). The treatment dose administrated in the VPA-LTG combination group was less than that in the VPA and LTG monotherapy groups. The shorter interval to loss of 3-Hz spike-and-wave complexes and the presence of occipital intermittent rhythmic delta activity on EEG were significant factors predicting good treatment response.
Typical absences are brief generalized seizures of sudden onset and termination and usually start in childhood or adolescence.1 Childhood absence epilepsy (CAE) is common form of idiopathic generalized epilepsy with frequent, complete loss of consciousness, abrupt onset. CAE typically begins between 4 and 10 years of age, with the highest incidence in 5-7 year olds.23 Among the epilepsy syndromes, CAE generally has a favorable prognosis. Nonetheless, it is important to predict the treatment response, because a long-term follow-up study found that only 58% of patients with absence seizures remain in remission.4
Ethosuximide (ESM), valproic acid (VPA), and lamotrigine (LTG) are the most commonly used first-line therapies for treating absence epilepsy.56 Several studied have identified the efficacy and adverse effects associated with these drugs. VPA is typically regarded as being more effective than LTG,7 but patients often stop taking VPA due to adverse effects such as nausea, vomiting, weight gain, hair loss, and amenorrhea.8 LTG is associated with a high risk of skin rash and thus requires a relatively long titration phase before a therapeutic level in serum, and moreover its effect on seizure control diminishes over time.9 Difficulties have been experienced prescribing ESM because its domestic production and importation were temporarily stopped in 2010.
The aims of our study were to compare the outcomes for initial treatments of CAE with ESM, VPA, and LTG monotherapies and with VPA-LTG combination therapy, and to assess clinical factors that predict treatment response and prognosis.
Sixty-seven patients with electroencephalogram (EEG) findings of generalized, synchronous 3-Hz spike-and-wave activity were evaluated. All patients were treated at the Korea University Medical Center between January 2005 and March 2014. This investigation was approved by each of the Institutional Review Boards of the three Korea University-affiliated hospitals.
The following inclusion criteria were applied: patients had typical childhood absence seizures as frequent, brief, and severe impairment of consciousness with childhood onset. Ictal EEG showed a bilateral synchronous, symmetric spikeand-wave complex that lasted at least 3 s on top of the normal background activity.
Patients were excluded if they had any of the following: a history of afebrile seizures (e.g., afebrile generalized tonicclonic seizure or myoclonic seizures) other than typical absence seizures, clinical signs and symptoms consistent with a diagnosis of juvenile absence epilepsy or juvenile myoclonic epilepsy, a history of received treatment with anti-epileptic drugs (AEDs), evidence of a progressive or causative cerebral lesion, or a history of mental retardation.
We retrospectively reviewed the medical records of the patients to determine the age at absence seizure onset, sex, febrile seizure history, family history of epilepsy, occipital intermittent rhythmic delta activity (OIRDA) on EEG, type and dose of AEDs, and total medication duration for each therapy. We also evaluated treatment responses with regards to the seizure-free interval, duration of the seizure-free period, breakthrough seizure frequency, and freedom from treatment failure. We aimed to determine the relationship between these factors and the treatment response, which was defined as good if the treatment was terminated successfully within 3 years or if the patient remained seizure free for 18 months. The rate of freedom from treatment failure was defined that the percentage of patients who remained on the primary drugs initiated at the start of treatment or who finished the treatment as a first drug before 48 months. We constructed curves of the time to treatment failure over the 48-month period.
Data processing and analysis were performed with SPSS (version 20, SPSS, Chicago, IL, USA). The chi-square test and Fisher's exact tests were used to compare nominal data according to medication. ANOVA and post hoc test were used to compare the variables between primary medication groups; the results are presented in Table 1. A stepwise multivariate logistic regression model was used to evaluate the predictive ability of independent variables and their association with outcome measurements. Rates of freedom from failure were compared using Fisher's exact test for the pairwise comparisons between the treatments. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated.
Sixty-seven children with CAE were included in the study. They exhibited a skewed sex distribution: 43 were girls and 24 were boys. The age at seizure onset was 7.9±2.7 years (mean±SD), and the follow-up duration was 4.4±3.7 years. The first EEG monitoring was performed in the 67 subjects at 1.79±1.45 months after treatment, and the first clinic follow-up for seizure monitoring was performed at 1.40±0.62 weeks. Thereafter the patients were followed up every 1-2 months depending on how well the seizures were controlled.
Clinical features and EEG findings according to the choice of first drug are summarized in Table 1. Of the 67 patients, 22 were initially treated with ESM (32.8%), 23 with VPA (34.3%), 14 with LTG (20.9%), and 8 with a VPA-LTG combination (11.9%). Twelve patients (17.9%) experienced febrile seizures prior to the absence seizures. Five patients (7.5%) had a family history of epilepsy, and this differed significantly between the groups (p=0.033). The LTG dose used in the VPA-LTG combination group was significantly lower than the dose used when LTG was applied as a monotherapy (2.51± 1.23 vs. 4.14±1.70 mg/kg/day; p=0.037).
The breakthrough seizure frequency and interval to the loss of interictal 3-Hz spike-and-wave complexes differed significantly between the groups (p=0.024 and p=0.015, respectively) (Table 1). In the additional analysis, the breakthrough seizure frequency was significantly higher for LTG than for ESM and VPA [p=0.03 and p=0.029, respectively, in ANOVA with post hoc pairwise Tukey honestly significant difference (HSD)]. The interval to the loss of interictal 3-Hz spike-and-wave complexes was also longer for LTG than for ESM and VPA (p=0.018 and p=0.03, respectively, in ANOVA with post hoc pairwise Tukey HSD). There was no significant differences in the treatment response.
There was no significant differences between the four treatment groups in the interval to reach a seizure-free state from the finish of medication titration, or in the total period during which the seizure-free status was maintained, which was closely correlated with the treatment response. Three of the eight patients who were treated with the VPA-LTG combination were classified into the poor treatment response group. In two of these patients the seizures were controlled by increasing the dose increment after the relapse, while in the third patient the medication had to be continued without change due to intermittent seizure episodes. A good response to treatment was exhibited by 45 (67.2%) of the patients, of which 28.9% were boys and 71.1% were girls. The relationships of treatment response with sex, febrile seizure history, family history, EEG findings, and medication were assessed in order to identify the factors that significantly affected the treatment response (Table 2). The independent variables were tested by multivariate logistic regression analysis with backward stepwise selection of variables. The obtained data demonstrated that a longer interval to the loss of 3-Hz spike-and-wave complexes was an unfavorable prognostic factor (OR= 1.17; 95% CI=1.06-1.30, p=0.002). The presence of OIRDA a favorable predictors for treatment response for patients with CAE (OR 27.90; 95% CI 1.03-757.50, p=0.048).
While some patients maintained their primary regimen, other patients switched from their primary regimen to another regimen owing to poor treatment responses and/or adverse events (Supplementary Fig. 1 in the online-only Data Supplement). Most of these patients were well treated with the first or second drug. In particular, VPA (16/23, 69.6%) and the VPA-LTG combination (8/8, 100%) provided effective seizure control and were maintained as the first regimen. Patients who changed their medication to the VPA-LTG combination and VPA as the second regimen finished the treatment successfully without any further changes. The ESM (12/22, 54.5%) and LTG (8/14, 57.1%) groups had lower maintenance rates for the first drug, with 45.5% and 42.9% of them changing to the second drug, respectively, and 9.1% and 7.1% of them changing to the third drug.
After 48 months of therapy, 43 (64.2%) of the patients exhibited freedom from treatment failure. The rate of freedom from treatment failure was higher in the VPA-LTG combination group than in the three monotherapy groups (p=0.012) (Fig. 1). The OR for freedom from treatment failure for the VPA-LTG combination group was 2.197 vs. ESM (95% CI=1.392-3.472, p=0.010), 1.277 vs. VPA (95% CI=1.029-1.584, p=0.291), and 2.00 vs. LTG (95% CI=1.184-3.378, p=0.022). Eighteen patients in the VPA group who showed freedom from treatment failure continued the primary drug during the first 48 months, after which two of them changed to ESM as the secondary drug due to relapse.
Treatment failure occurred in 24 (35.8%) patients during the follow-up period. The most common reason for treatment failure was a lack of seizure control (16 of 24, 66.6%); this occurred in six subjects in the ESM group, four in the VPA group, six in the LTG group, and none in the VPA-LTG combination group. Three subjects had to change their first medication owing to adverse effects: one subject each in the ESM, VPA, and LTG groups, with none in the VPA-LTG combination group. These adverse effects included rash and abdominal pain (n=2) and nausea and vomiting (n=1). Four subjects had to change their medication due to sustained interictal electrical seizure activities: two subjects in the ESM group, one in the VPA group, one in the LTG group, and none in the VPA-LTG combination group. The drug was replaced in one patient due to the stop in 2010 of the production of ESM temporarily. The frequency of treatment failures due to either adverse effects or EEG seizure activity did not differ significantly among the treatment groups.
The relapse rate after remission was 13.6% (3 of 22) in the ESM group, 8.7% (2 of 22) in the VPA group, 35.7% (5 of 14) in the LTG group, and 25.0% (2 of 8) in the VPA-LTG combination group.
All seven patients who switched to VPA as the second regimen maintained that regimen. Eight of the ten (80%) patients who changed to LTG as the second regimen maintained that regimen: one patient switched to ESM and one patient switched to VPA. The single patient who changed the second drug to the VPA-LTG combination therapy maintained that medication.
The purpose of this study was to compare the treatment outcomes of four first-line therapies for childhood absence seizures, and to determine factors associated with their prognosis. The initial therapy outcomes as evaluated according to freedom from treatment failure were superior in patients who received VPA monotherapy or VPA-LTG combination therapy. Our results also showed that children who had a shorter interval to the loss of 3-Hz spike-and-wave complexes and the presence of OIRDA on EEG had a good prognosis.
Absence epilepsy is a common form of pediatric idiopathic generalized epilepsy, and accounts for a relatively high proportion (60-70%) of seizures in girls.10 Most of the available data suggest that ESM, VPA, and LTG are predominantly used as the primary therapeutic drugs for CAE, with a wide range of reported remission rates (33-79%).1112 Most (84%) of the absence-seizure patients in one study stopped taking their medication within 3 years, although some showed a poor reaction to the medication or had other types of seizures during treatment, which made their conditions more difficult to treat.10 Absence seizures have recently been associated with a deficit in cognitive and language skills and behavior disorders, despite seizure control, which highlights the importance of determining factors associated with prognosis. 1314 Our study suggests that a shorter interval to the loss of 3-Hz spike-and-wave complexes and the presence of OIRDA are predictors for a good treatment response. Consistent with these findings, Guilhoto et al.15 reported that it was possible to control seizures more effectively in patients with OIRDA, and thus proposed this a good prognostic factor in absence seizures. In contrast, Dlugos et al.16 reported that freedom from failure at 16-20 weeks after treatment was not affected by the presence or absence of OIRDA. In the study, the presence of OIRDA appeared to be a highly significant factor suggesting a good prognosis; further research on its prognostic utility is clearly needed.
The LTG group, which showed a lower rate of freedom from treatment failure, had a significantly longer interval to the loss of interictal 3-Hz spike-and-wave complexes. According to Li et al.,17 an interictal 3-Hz spike-and-wave complex on EEG is associated with characteristic signal changes on functional MRI, which differ from that for an ictal 3-Hz spike-and-wave complex. Thus, a shorter interval to the loss of the interictal 3-Hz spike-and-wave complex may be clinically used to predict better outcomes of absence seizures.
It is possible that absence seizures appearing first in either childhood or adolescence, followed by myoclonic jerks and generalized tonic clonic seizures, will develop into juvenile myoclonic epilepsy or juvenile absence epilepsy and have a poor prognosis.1 Also, the commonly known factors predicting prognosis are the age at which seizures first started, an abnormal background rhythm or polyspikes on EEG readings, mental retardation, a history of absence status, a positive family history, and a history of febrile convulsions.1118 We suspect that the inclusion of more patients would have allowed more conclusive prognostic factors to be identified in the present study.
While ESM, LTG, and VPA are the most commonly used primary drugs of choice in the treatment of absence seizures, their efficacy is the subject of considerable debate. In a 2005 review, Posner reported that ESM, VPA, and LTG are all effective first-line therapies for absence seizures, with no distinct differences in their efficacies.19 According to Wheless20 ESM is the primary drug of choice for the treatment of CAE, while VPA and LTG are those for the treatment of JAE. Glauser et al.8 reported that cases of a high incidence of patients substituting a first-line drug with a second-line drug were due to adverse effects such as weight gain, hair loss, and vomiting. Both LTG and VPA have been found to have similar incidence rates of mild adverse effects, including fatigue, headache, and changes in appetite, but the incidence of serious adverse effects, such as vomiting, insomnia, and hyperactivity, has been lower for LTG than for ESM and VPA.21 However, the slow titration period required by LTG due to the risk of skin rash means that it takes longer to reach effective therapeutic levels in serum, and LTG is known to have a lower capability to control seizures.8 The availability of ESM was restricted by its production being temporarily stopped in 2010. Thus, the present study focused on evaluating the efficacy of VPA-LTG combination therapy for the treatment of newly diagnosed absence epilepsy.
We found that the rate of freedom from failure at 48 months was higher for VPA-LTG combination therapy than for the other three therapies. Additionally, the treatment dose administered in the VPA-LTG combination group was less than that administered in the VPA and LTG monotherapy groups. Several previous studies have found that VPA-LTG combination therapy is effective at regulating seizures.22 Pisani et al.23 applied VPA-LTG combination therapy to 13 patients who were refractory to VPA or LTG monotherapy, and found that this change controlled the seizures in 4 patients and decreased their frequency in another 4 (62-78%). The treatment dose and serum drug level were significantly lower in patients taking the VPA-LTG combination regimen than in those taking VPA or LTG only. In a recent retrospective study by Moeller et al.,24 35 patients (25 with generalized epilepsy and 10 with partial epilepsy) who were refractory to single-drug therapy were treated with a combination of VPA and LTG. The results showed that 62.8% of the patients exhibited an improved response to the VPA-LTG combination regimen: 18 patients remained completely seizure free, 4 were improved, and 13 exhibited no response. It is generally accepted that VPA can potentiate the effects of LTG by inhibiting LTG hepatic glucuronidation, thereby increasing the plasma half-life of LTG.123 Consistent with our own results, these findings also support the suitability of VPA-LTG combination therapy as a primary treatment for absence seizures.
During the primary treatment regimen, adverse effects were seen in 4.5% (1 of 22) of those in the ESM group, 4.3% (1 of 23) in the VPA group, 7.1% (1 of 14) in the LTG group, and 0% (0 of 8) in the VPA-LTG combination group. The risk of adverse effects generally increases with the AED dose; however, fewer adverse effects were seen in VPA-LTG combination therapy, which we attribute to each drug in the VPA-LTG combination therapy being administered at a lower dose than when applying it as a monotherapy. In addition, the rate of treatment interruption due to side effects of AEDs in the VPA-LTG combination group might be expected to decrease. Pisani et al.23 suggested that the benefits of VPA-LTG combination therapy outweigh the adverse effects when compared to single-drug therapy. However, it is difficult to make comparisons between their study and the present one since the former included only a small number of patients who had received the VPA-LTG combination therapy, and these patients had also previously been treated with multiple other drugs.
One limitation of the present study is that it applied a retrospective analysis, and so there was no systemically planned titration phase, regular follow-up period, or EEG monitoring interval. The AED dose was titrated in a stepwise manner in our medical center. The target dose was 2-7 mg/kg/day for LTG and 10-30 mg/kg/day for VPA; these doses are lower than those normally used in other countries.21 In the present retrospective study, the first seizure monitoring was performed at 1.40±0.62 weeks after treatment, the patients were usually followed up every 1-2 months thereafter (except for the first clinic follow-up from treatment) depending on how well the seizures were controlled. The follow-up interval for evaluating the treatment response and the increase in the dose differ for the previous study, and so the evaluation results for the treatment may vary. Further, the small amount of data made it difficult to assess the treatment responses exactly, including the seizure frequency and adverse effects. A prospective or randomized controlled clinical trial would be expected to yield more reliable results.
Figures and Tables
Fig. 1
Freedom from treatment failure in the four medication groups. After 48 months of therapy, the rate of freedom from treatment failure differed significantly between medication groups (p=0.012). The rates of freedom from treatment failure were 100% and 45.5%, respectively. The odds ratio for freedom from treatment failure for the VPA-LTG combination group was 2.20 vs. ESM [95% confidence interval (CI)=1.39-3.47, p=0.010], 1.28 vs. VPA (95% CI=1.03-1.58, p=0.291), and 2.00 vs. LTG (95% CI=1.18-3.38, p=0.022). ESM: ethosuximide, LTG: lamotrigine, V+L: valproate+lamotrigine, VPA: valproate.
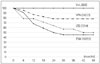
Table 1
Comparison of clinical characteristics among patient groups according to the first antiepileptic drug

Table 2
Clinical and EEG factors that predict treatment response

Results are reported as mean±SD, or number (%).
*p<0.05 using multivariate regression analysis.
ESM: ethosuximide, F/Hx: family history, LTG: lamotrigine, mo: month, n: number, OIRDA: occipital intermittent rhythmic delta activity, P/Hx: past history, sz: seizure, V+L: valproate+lamotrigine, VPA: valproate.
References
1. Panayiotopoulos CP. Treatment of typical absence seizures and related epileptic syndromes. Paediatr Drugs. 2001; 3:379–403.

2. Jallon P, Latour P. Epidemiology of idiopathic generalized epilepsies. Epilepsia. 2005; 46:Suppl 9. 10–14.

3. Hirsch E, Panayiotopoulos CP. Childhood absence epilepsy and related syndromes. In : Roger J, Bureau M, Dravet C, Genton P, Tassinari CA, Wolf P, editors. Epileptic syndromes in infancy, childhood and adolescence. 4th ed. Montrouge: John Libbey Eurotext;2005. p. 315–335.
4. Trinka E, Baumgartner S, Unterberger I, Unterrainer J, Luef G, Haberlandt E, et al. Long-term prognosis for childhood and juvenile absence epilepsy. J Neurol. 2004; 251:1235–1241.

5. Posner EB, Mohamed K, Marson AG. Ethosuximide, sodium valproate or lamotrigine for absence seizures in children and adolescents. Cochrane Database Syst Rev. 2005; (4):CD003032.

6. Lee JY, Yum MS, Kim EH, Lee EH, Ko TS. Lamotrigine as a first-line monotherapy in children with absence seizures. J Korean Child Neurol Soc. 2011; 19:142–149.
7. Coppola G, Auricchio G, Federico R, Carotenuto M, Pascotto A. Lamotrigine versus valproic acid as first-line monotherapy in newly diagnosed typical absence seizures: an open-label, randomized, parallel-group study. Epilepsia. 2004; 45:1049–1053.

8. Glauser TA, Cnaan A, Shinnar S, Hirtz DG, Dlugos D, Masur D, et al. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy. N Engl J Med. 2010; 362:790–799.

9. Coppola G, Licciardi F, Sciscio N, Russo F, Carotenuto M, Pascotto A. Lamotrigine as first-line drug in childhood absence epilepsy: a clinical and neurophysiological study. Brain Dev. 2004; 26:26–29.

10. Hughes JR. Absence seizures: a review of recent reports with new concepts. Epilepsy Behav. 2009; 15:404–412.

11. Grosso S, Galimberti D, Vezzosi P, Farnetani M, Di Bartolo RM, Bazzotti S, et al. Childhood absence epilepsy: evolution and prognostic factors. Epilepsia. 2005; 46:1796–1801.

12. Wirrell EC. Natural history of absence epilepsy in children. Can J Neurol Sci. 2003; 30:184–188.

13. Matricardi S, Verrotti A, Chiarelli F, Cerminara C, Curatolo P. Current advances in childhood absence epilepsy. Pediatr Neurol. 2014; 50:205–212.

14. Mandelbaum DE, Burack GD, Bhise VV. Impact of antiepileptic drugs on cognition, behavior, and motor skills in children with newonset, idiopathic epilepsy. Epilepsy Behav. 2009; 16:341–344.

15. Guilhoto LM, Manreza ML, Yacubian EM. Occipital intermittent rhythmic delta activity in absence epilepsy. Arq Neuropsiquiatr. 2006; 64(2A):193–197.

16. Dlugos D, Shinnar S, Cnaan A, Hu F, Moshé S, Mizrahi E, et al. Pretreatment EEG in childhood absence epilepsy: associations with attention and treatment outcome. Neurology. 2013; 81:150–156.

17. Li Q, Luo C, Yang T, Yao Z, He L, Liu L, et al. EEG-fMRI study on the interictal and ictal generalized spike-wave discharges in patients with childhood absence epilepsy. Epilepsy Res. 2009; 87:160–168.

18. Wirrell EC, Camfield CS, Camfield PR, Gordon KE, Dooley JM. Long-term prognosis of typical childhood absence epilepsy: remission or progression to juvenile myoclonic epilepsy. Neurology. 1996; 47:912–918.

19. Posner EB, Mohamed K, Marson AG. A systematic review of treatment of typical absence seizures in children and adolescents with ethosuximide, sodium valproate or lamotrigine. Seizure. 2005; 14:117–122.

20. Wheless JW. Acute management of seizures in the syndromes of idiopathic generalized epilepsies. Epilepsia. 2003; 44:Suppl 2. 22–26.

21. Glauser TA, Cnaan A, Shinnar S, Hirtz DG, Dlugos D, Masur D, et al. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy: initial monotherapy outcomes at 12 months. Epilepsia. 2013; 54:141–155.

22. Brodie MJ, Sills GJ. Combining antiepileptic drugs--rational polytherapy? Seizure. 2011; 20:369–375.

Supplementary Materials
The online-only Data Supplement is available with this article at http://dx.doi.org/10.3988/jcn.2016.12.2.160.
Supplementary Fig. 1
Switching of antiepileptic drugs (first, second, and third choices). This graph shows a trend in the used medications. Most of the patients were treated effectively by the first or second drug. In particular, VPA and the VPA-LTG combination provided effective seizure control and were maintained as the first drug [16 of 23 (69.6%) and 8 of 8 (100%) patients, respectively]. The ESM and LTG groups exhibited lower maintenance rates for the first drug [12 of 22 (46.9%) and 8 of 14 (37.5%) patients, respectively]. This graph excludes two patients who were treated with other drugs such as zonisamide. ESM: ethosuximide, LTG: lamotrigine, VPA: valproate.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download