Abstract
Background and Purpose
To determine how cognitive function is related to epilepsy classification and comorbid attention deficit hyperactivity disorder (ADHD) in children with newly diagnosed epilepsy of genetic or unknown etiology.
Methods
The medical records of children aged 6-16 years with newly diagnosed epilepsy of genetic or unknown etiology were reviewed retrospectively. The Korean Education Development Institute-Wechsler Intelligence Scale for Children and the Comprehensive Attention Test were used to evaluate intelligence and attention/executive function, respectively.
Results
The data of a total of 149 children, 103 with focal seizures and 46 with generalized seizures, were reviewed. The prevalence of ADHD was 49.2% (59 out of 120 examined patients), and ADHD patients exhibited significantly worse auditory selective attention, flanker test results, and spatial working memory. Patients with generalized seizures exhibited significantly worse auditory selective and sustained attention than patients with focal seizures. In patients with generalized seizures, sustained attention, flanker test findings, and spatial working memory were found to be affected by ADHD, and auditory selective and sustained attention were significantly worse in patients with benign childhood epilepsy with centrotemporal spikes and ADHD than in their counterparts without ADHD.
Epilepsy is one of the most common neurologic childhood disorders.1 Although children with epilepsy frequently present with neuropsychiatric problems during the course of their lifetime, they have only recently been studied systemically.2,3 The prevalence of attention deficit hyperactivity disorder (ADHD), learning disorders, and developmental disorders is higher in children with epilepsy than in normal controls, and approximately half of children with epilepsy require special education programs.1,4,5 Neuropsychiatric impairments in these patients have been attributed to interactions between ongoing seizures, antiepileptic drugs, and underlying causes of symptomatic epilepsy,6,7 but there might also be contributions from the innate properties of epilepsy.8,9,10 Previous studies have established that children with recent-onset epilepsy demonstrate antecedent cognitive impairments or academic underachievement before the first recognized seizure,11 suggesting the presence of common neurobiological mechanisms.
The high comorbid prevalence of ADHD and epilepsy suggests that there is a bidirectional relationship between these disorders.12,13 Cognitive impairment and attentional problems are particularly crucial issues in children with epilepsy who are in a vigorous phase of neurodevelopment. Cognitive impairment is more common in children with epilepsy of structural/metabolic causes than in those with epilepsy of unknown or genetic etiology.14 Children with new-onset epilepsy of unknown or genetic etiology are not influenced by factors that can influence cognitive function, such as brain lesions and drug side effects, which may help evaluate the effects of innate epilepsy on cognitive function.10
The different innate neurobiological characteristics of children with epilepsy and the bidirectional relationship between ADHD and epilepsy were investigated by exploring intelligence and attention and working memory according to type of epilepsy, and the presence or absence of comorbid ADHD.
The medical records of children aged 6-16 years with newly or recently diagnosed epilepsy of genetic or unknown etiology at the Asan Medical Center Children's Hospital between 2008 and 2011 were reviewed retrospectively. Children with an intelligence quotient (IQ) of <70, underlying brain lesions, or chronic illness that limited their daily activities were excluded. Epilepsy type was classified by a board-certified Korean pediatric neurologist based on electroencephalography and clinical findings and in accordance with the classifications of the International League Against Epilepsy.15 The first routine electroencephalography records at diagnosis were selected for this process. Patients were classified based on this electroclinical evidence as having generalized or focal seizures. They were further classified according to the total number of seizures since the first event (single vs. multiple) and the presence or absence of comorbid ADHD. ADHD was diagnosed according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) by a pediatric psychiatrist. The data of patients with well-established electroclinical syndromes or benign childhood epilepsy with centrotemporal spikes (BCECTS) were analyzed separately.
The Korean Education Development Institute-Wechsler Intelligence Scale for Children (KEDI-WISC) was determined to be an appropriate tool with which to evaluate this group of patients, and was used to measure intelligence, determine verbal performance, and assess full-scale IQ.16 The Comprehensive Attention Test (CAT), which was developed to evaluate the attention of Korean children and adolescents in ADHD research trials,17 was used to measure attention and working memory. The time delay between the diagnosis of epilepsy and psychometric analysis was a maximum of 4 months. The CAT comprises five attention tasks and one spatial working-memory task.
The attention tasks employed in this study included the following: visual selective attention, auditory selective attention, sustained attention to response, flanker (interference), and divided attention tasks. Two outcome measures were quantified for each task: omission errors (failure to respond to a target) and commission errors (erroneously responding to a nontarget). For spatial working-memory tasks, forward and backward memory spans and correct responses were measured. All scores were adjusted for age and sex, with higher scores indicating better attention. Licensed clinical psychologists administered all tests.
All analyses were performed using SPSS (version 18.0 for Windows, IBM, USA). A nonparametric Mann-Whitney test was used to compare CAT and KEDI-WISC scores between seizure classifications and between patients with multiple or single seizures. The psychometric data of the patients with and without ADHD were compared using Student's t-test. Correlations between age and psychometric scores were analyzed using Spearman correlation analysis.
The data of 149 children [76 males and 73 females; age at evaluation, 10.0±3.1 years (mean±SD)] were reviewed. Of this population, 103 patients (69%; age, 9.5±3.1 years) presented with focal seizures, and 46 (31%; age, 11.1±3.0 years) presented with generalized seizures. The prevalence of ADHD was 45.7% in the patients with focal seizures (37 patients with a diagnosis of ADHD out of 81 patients evaluated by a psychiatrist), 56.4% in patients with generalized seizures (22 of 39 patients); the difference was not statistically significant (p=0.271; χ2 test). In the psychometric evaluation, 26 patients (17.4%) had experienced a single seizure episode and all others had experienced multiple seizure episodes (Table 1). Verbal IQ, performance IQ, and full-scale IQ scores did not differ significantly between patients with focal and generalized seizures (Table 1). IQ scores were not affected by age, number of seizures, electroclinical syndromes, antiepileptic drugs, or comorbid ADHD.
Attention deficit hyperactivity disorder patients demonstrated significantly lower scores for the auditory selective attention commission error (97.6±18.7 vs. 104.6±10.1; p<0.020), flanker task omission error (87.6±22.0 vs. 96.7±18.0; p=0.031), spatial working-memory forward span (86.0±20.9 vs. 100.4±20.3; p=0.007), and backward memory span (93.5±16.9 vs. 100.7±17.2; p=0.006) (Fig. 1). The correlation between psychometric data and age at seizure onset was also analyzed. The scores for auditory selective attention omission error (r=-0.63; p<0.001), auditory selective attention commission error (r=-0.42; p<0.001), and visual selective attention omission error (r=-0.19; p=0.033) were significantly and negatively correlated with age (Fig. 2). Regarding seizure classification, patients with focal seizures demonstrated a significantly higher scores for the auditory selective attention omission error (109.0±14.6 vs. 103.5±11.6; p=0.004) and auditory selective attention commission error (101.3±16.9 vs. 98.0±12.1; p=0.007; Mann-Whitney test) (Table 2). There was no significant difference between patients with BCECTS and patients with other focal seizures in this regard.
When psychometric data were separated according to seizure type, patients with generalized seizures demonstrated significant differences in comorbid ADHD. Omission error scores on sustained attention (p=0.050) and flanker tasks (p=0.003), and forward and backward working-memory scores on the spatial working-memory task (p=0.025 for forward memory; p=0.035 for backward memory) were lower in patients with generalized seizures and ADHD than in their non-ADHD counterparts (Fig. 3). Among BCECTS patients, the commission error scores on the auditory selection task (p=0.004) and omission error scores on the sustained attention task (p=0.039) were lower in BCECTS patients with ADHD than in their non-ADHD counterparts.
Children with epilepsy commonly develop neuropsychiatric problems. The high prevalence of mood disorders, autism, and ADHD in these patients is well recognized. These problems were historically considered as secondary findings; however, seizures and neurobehavioral presentations are now considered to be different biological components of specific types of epilepsy.13,18 Accordingly, the diagnosis and management of these neurobehavioral comorbidities are strongly emphasized in the treatment of epilepsy.5 The neurobehavioral phenotypes that are unaffected by pathological brain lesions, treatment, or seizure burden were determined by focusing on new or recent-onset epilepsy due to unknown/genetic etiology. Despite having a normal intelligence, children with epilepsy may demonstrate attention deficits.19 The prevalence of attention deficits in pediatric patients with epilepsy has been reported to be as high as 77%.20,21 Moreover, a recent study found similar working-memory deficits in patients with epilepsy-related ADHD or developmental ADHD, which strongly suggests the existence of a common underlying neurobehavioral pathophysiology between ADHD with and without epilepsy.22
The present study found that the incidence of ADHD was high (45.7%) in children with epilepsy of unknown or genetic etiology, and that this disorder was significantly associated with poor performances on auditory selection attention, interference, and spatial working memory. This is consistent with previous studies involving pediatric patients, and demonstrates clearly that children with ADHD and epilepsy demonstrate poorer auditory attention and working memory than either epileptic children without ADHD19 or ADHD children without epilepsy.23 Patients with ADHD exhibit difficulties in working-memory performance,24,25 which ties in closely with the impaired working memory identified in the epileptic patients with ADHD reviewed in the present study.
The patients in this study with generalized seizures demonstrated worse auditory selective attention than patients with focal seizures. Intrinsic attention deficits and some differences in attention between patients with generalized seizures and patients with focal seizures have also been found in studies involving small groups of children with epilepsy.7,19 However, the exact mechanisms underlying any differences in neuropsychiatric impairments across epilepsy classifications remain unclear.
The dichotomic seizure classification used in the present study inevitably resulted in heterogeneity among the epilepsy patients included in each group. The patients with generalized seizures mostly included patients previously diagnosed with idiopathic generalized epilepsy (IGE), a cluster of syndromes that includes childhood absence epilepsy, juvenile absence epilepsy, and juvenile myoclonic epilepsy.15 Children with generalized epilepsy exhibit greater hyperactivity and emotional and conduct problems than healthy controls or children with benign focal epilepsy.26 It has also been reported that children with IGE demonstrate decreased sustained attention27 and a decreased ability to assemble objects28 compared with children with focal seizures. Considering that the impaired executive control associated with IGE is suggestive of frontal network involvement,29 the presence of low auditory attention in patients with generalized seizures could be associated with disrupted attentional processes due to abnormal diffuse neural circuitry activation.
The present evaluations revealed that the prevalence of ADHD was similar regardless of the type of epilepsy. However, several subsets of attention were found to be affected by ADHD in patients with generalized seizures and BCECTS. Among the patients with generalized seizures, the ADHD cases demonstrated significantly worse sustained attention, interference, and spatial working memory than their counterparts without ADHD. There were no differences between children in this cohort with focal seizures regardless of ADHD, and those with BCECTS and ADHD demonstrated significantly worse auditory attention and sustained attention compared with the children in this series without ADHD. The affected domains were found to differ between epilepsy classifications, possibly due to the interactions between ADHD and epilepsy.
In general, attention is associated with cognitive processing speed, which is in turn related to activity in the anterior cingulate cortex, prefrontal cortex, and striatothalamic pathway.29 Interference involves mainly the ventrolateral prefrontal cortex and the left anterior prefrontal cortex,30 and working-memory functions are scattered over large parts of the cortex including the prefrontal cortex.31 The pathways involved in attention, interference, and working memories are also hypothetically associated with ADHD,32 and the generation of generalized spikes and waves in IGE reportedly involve the "fronto-insular-thalamic network".33,34 Thus, the comorbid presentation of epilepsy, generalized seizures, and ADHD may interfere with broader areas of the cognitive network and result in selective decrements in sustained attention, interference, or spatial working memory in comparison to patients without ADHD.
The BCECTS patients in the present series comprised one-third of the cases with focal seizures, and were analyzed separately from the other patients with focal seizures. Other cases with focal seizures may also include patients with various foci, and this complicated situation may be an obstacle to identifying specific cognitive findings in these patients. Although BCECTS appears benign, it has frequently been associated with neuropsychiatric impairments such as ADHD.35 Previous studies have shown that children with BCECTS exhibit difficulties in impulse control36 and that children with ADHD exhibit a frequency of rolandic spikes that is higher than that expected from epidemiological data.37 The complex network that incorporates attention, impulsivity, and rolandic spikes38,39 may underlie the difficulties in auditory selective attention and sustained attention that were observed in BCECTS patients with ADHD in the present study.
A significant negative correlation was found in this analysis between auditory and visual selective attention and age at onset, which we regard as innate characteristics of epilepsy. Early onset could also include epilepsy with a more benign nature, such as BCECTS and childhood absence epilepsy, and late-onset epilepsy may include juvenile myoclonic epilepsy or juvenile absence epilepsy, thereby explaining the relatively poor level of attention in these categories.
The limitations of this study include its retrospective design, the analysis of data obtained from a relatively small number of patients from a single institution, the lack of normal controls without epilepsy, and the time delay between the diagnosis and psychometric evaluation. However, the analyses have provided information on cognitive problems in children with epilepsy of unknown/genetic etiology, and the findings suggest that epileptic seizure classification and ADHD can influence cognitive function in this population. The pretreatment cognitive data collected from epileptic children may explain the poor school performance associated with epilepsy. Proper characterization of these impairments could be useful in early interventions in the disease course. Further prospective studies with additional patients will help clinicians to better treat children with epilepsy and cognitive impairments in the future.
Figures and Tables
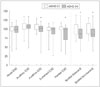 | Fig. 1Attention and spatial working memory scores according to comorbid ADHD in the study children with unknown/genetic epilepsy. ADHD patients demonstrated significantly lower auditory selective attention commission errors (P<0.020), flanking test omission errors (p=0.031), and spatial working memory forward (p=0.007) and backward memory spans (p=0.006). p values were obtained using the Student's t test. *p<0.05. ADHD: attention deficit hyperactivity disorder, CE: commission errors, OE: omission errors. |
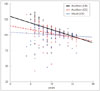 | Fig. 2Correlation between attention scores and age in children with epilepsy. The auditory selective attention omission error (OE) (r=-0.63, p<0.001), auditory selective attention commission error (CE) (r=-0.42, p<0.001), and visual selective attention OE (r=-0.19, p=0.033) demonstrated a significant and negative correlation with age according to the Spearman correlation analysis. Scores <40 were excluded to show the approximate data that correlated with the Spearman analysis. |
 | Fig. 3Attention and spatial working memory scores according to seizure classification and ADHD in the study cohort. Children with generalized seizures and ADHD demonstrated significantly lower scores for sustained attention, interference, and spatial working memory than those without ADHD. p values were obtained using the Mann-Whitney test. *p<0.05 compared to children with generalized seizure without ADHD. ADHD: attention deficit hyperactivity disorder, OE: omission errors. |
Table 1
Clinical characteristics and psychometric analysis of the study population according to the epilepsy classification

Table 2
Psychometric results for the study population according to epileptic seizure classification

References
1. Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics. 2012; 129:256–264.

2. Elger CE, Helmstaedter C, Kurthen M. Chronic epilepsy and cognition. Lancet Neurol. 2004; 3:663–672.

3. Selassie GR, Viggedal G, Olsson I, Jennische M. Speech, language, and cognition in preschool children with epilepsy. Dev Med Child Neurol. 2008; 50:432–438.

4. Berg AT, Smith SN, Frobish D, Levy SR, Testa FM, Beckerman B, et al. Special education needs of children with newly diagnosed epilepsy. Dev Med Child Neurol. 2005; 47:749–753.

5. Helmstaedter C, Aldenkamp AP, Baker GA, Mazarati A, Ryvlin P, Sankar R. Disentangling the relationship between epilepsy and its behavioral comorbidities - the need for prospective studies in new-onset epilepsies. Epilepsy Behav. 2014; 31:43–47.

6. MacAllister WS, Schaffer SG. Neuropsychological deficits in childhood epilepsy syndromes. Neuropsychol Rev. 2007; 17:427–444.

7. Bhise VV, Burack GD, Mandelbaum DE. Baseline cognition, behavior, and motor skills in children with new-onset, idiopathic epilepsy. Dev Med Child Neurol. 2010; 52:22–26.

8. Jeong MH, Yum MS, Ko TS, You SJ, Lee EH, Yoo HK. Neuropsychological status of children with newly diagnosed idiopathic childhood epilepsy. Brain Dev. 2011; 33:666–671.

9. Mandelbaum DE, Burack GD. The effect of seizure type and medication on cognitive and behavioral functioning in children with idiopathic epilepsy. Dev Med Child Neurol. 1997; 39:731–735.

10. You SJ. Cognitive function of idiopathic childhood epilepsy. Korean J Pediatr. 2012; 55:159–163.

11. Hermann B, Jones J, Sheth R, Dow C, Koehn M, Seidenberg M. Children with new-onset epilepsy: neuropsychological status and brain structure. Brain. 2006; 129(Pt 10):2609–2619.

12. Rappley MD. Clinical practice. Attention deficit-hyperactivity disorder. N Engl J Med. 2005; 352:165–173.
13. Chou IC, Chang YT, Chin ZN, Muo CH, Sung FC, Kuo HT, et al. Correlation between epilepsy and attention deficit hyperactivity disorder: a population-based cohort study. PLoS One. 2013; 8:e57926.

14. Gillis L, Kaye E. Diagnosis and management of mitochondrial diseases. Pediatr Clin North Am. 2002; 49:203–219.

15. Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van Emde Boas W, et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia. 2010; 51:676–685.

16. Park KS, Yoon JR, Park HJ, Park HJ, Kwon KO. Korean educational developmental institute-Wechsler intelligence scale for children (KEDI-WISC). Seoul: Korean Educational Development Institute;2002.
17. Yoo HK, Lee J, Kang SH, Park EH, Jung J, Kim BN, et al. Standardization of the comprehensive attention test for the Korean children and adolescents. J Korean Acad Child Adolesc Psychiatry. 2009; 20:68–75.
18. Socanski D, Aurlien D, Herigstad A, Thomsen PH, Larsen TK. Epilepsy in a large cohort of children diagnosed with attention deficit/hyperactivity disorders (ADHD). Seizure. 2013; 22:651–655.

19. Liu ST, Tsai FJ, Lee WT, Lee CM, Fan PC, Lin WS, et al. Attentional processes and ADHD-related symptoms in pediatric patients with epilepsy. Epilepsy Res. 2011; 93:53–65.

20. Dunn DW. Attention-deficit hyperactivity disorder, oppositional defiant disorder and conduct disorder. In : Ettinger AB, Kanner AM, editors. Psychiatric aspects of epilepsy: a practical guide to diagnosis and treatment. Baltimore: Lippincott/Williams & Wilkins;2001. p. 111–126.
21. Semrud-Clikeman M, Wical B. Components of attention in children with complex partial seizures with and without ADHD. Epilepsia. 1999; 40:211–215.

22. Bechtel N, Kobel M, Penner IK, Specht K, Klarhöfer M, Scheffler K, et al. Attention-deficit/hyperactivity disorder in childhood epilepsy: a neuropsychological and functional imaging study. Epilepsia. 2012; 53:325–333.

23. MacAllister WS, Vasserman M, Vekaria P, Miles-Mason E, Hochsztein N, Bender HA. Neuropsychological endophenotypes in ADHD with and without epilepsy. Appl Neuropsychol Child. 2012; 1:121–128.

24. Lenartowicz A, Delorme A, Walshaw PD, Cho AL, Bilder RM, McGough JJ, et al. Electroencephalography correlates of spatial working memory deficits in attention-deficit/hyperactivity disorder: vigilance, encoding, and maintenance. J Neurosci. 2014; 34:1171–1182.

25. Kim S, Liu Z, Glizer D, Tannock R, Woltering S. Adult ADHD and working memory: neural evidence of impaired encoding. Clin Neurophysiol. 2014; 125:1596–1603.

26. Dafoulis V, Kalyva E. Factors associated with behavioral problems in children with idiopathic epilepsy. Epilepsy Res. 2012; 100:104–112.

27. Maneshi M, Moeller F, Fahoum F, Gotman J, Grova C. Resting-state connectivity of the sustained attention network correlates with disease duration in idiopathic generalized epilepsy. PLoS One. 2012; 7:e50359.

28. Giordani B, Berent S, Sackellares JC, Rourke D, Seidenberg M, O'Leary DS, et al. Intelligence test performance of patients with partial and generalized seizures. Epilepsia. 1985; 26:37–42.

29. Tian Y, Dong B, Ma J, Zhou S, Zhou N, Wang K. Attention networks in children with idiopathic generalized epilepsy. Epilepsy Behav. 2010; 19:513–517.

30. Nee DE, Jonides J, Berman MG. Neural mechanisms of proactive interference-resolution. Neuroimage. 2007; 38:740–751.

31. Smith EE, Jonides J. Storage and executive processes in the frontal lobes. Science. 1999; 283:1657–1661.

32. Purper-Ouakil D, Ramoz N, Lepagnol-Bestel AM, Gorwood P, Simonneau M. Neurobiology of attention deficit/hyperactivity disorder. Pediatr Res. 2011; 69(5 Pt 2):69R–76R.

33. Aghakhani Y, Bagshaw AP, Bénar CG, Hawco C, Andermann F, Dubeau F, et al. fMRI activation during spike and wave discharges in idiopathic generalized epilepsy. Brain. 2004; 127(Pt 5):1127–1144.

34. Stefan H, Paulini-Ruf A, Hopfengärtner R, Rampp S. Network characteristics of idiopathic generalized epilepsies in combined MEG/EEG. Epilepsy Res. 2009; 85:187–198.

35. Kwon S, Seo HE, Hwang SK. Cognitive and other neuropsychological profiles in children with newly diagnosed benign rolandic epilepsy. Korean J Pediatr. 2012; 55:383–387.

36. Chevalier H, Metz-Lutz MN, Segalowitz SJ. Impulsivity and control of inhibition in Benign Focal Childhood Epilepsy (BFCE). Brain Cogn. 2000; 43:86–90.
37. Holtmann M, Becker K, Kentner-Figura B, Schmidt MH. Increased frequency of rolandic spikes in ADHD children. Epilepsia. 2003; 44:1241–1244.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download