This article has been corrected. See "Erratum to: Feasibility of Using a Mobile Application for the Monitoring and Management of Stroke-Associated Risk Factors" in Volume 11 on page 295.
Abstract
Background and Purpose
Recent advances in information technology have created opportunities for advances in the management of stroke. The objective of this study was to test the feasibility of using a smartphone software application (app) for the management of vascular risk factors in patients with stroke.
Methods
This prospective clinical trial developed a smartphone app, the 'Korea University Health Monitoring System for Stroke: KUHMS2,' for use by patients with stroke. During a 6-month follow-up period, its feasibility was assessed by measuring the changes in their vascular risk-factor profiles and the number of days per patient with data registration into the app. The effect of the app on the achievement rate of risk-factor targets was assessed by classifying subjects into compliant and noncompliant groups.
Results
At the end of the trial, data on 48 patients were analyzed. The number of days on which data were registered into the app was 60.42±50.17 (mean±standard deviation). Among predefined vascular risk factors, the target achievement rate for blood pressure and glycated hemoglobin (HbA1c) improved significantly from baseline to the final measurement. The serial changes in achievement rates for risk-factor targets did not differ between the compliant and noncompliant groups.
Stroke is one of the most common causes of mortality and disability, and represents a huge socioeconomic burden.1 Despite the development of therapeutic strategies and other efforts to reduce the risk of stroke, the efficacy of secondary prevention is often unsatisfactory.1,2 Current main strategies for preventing stroke recurrence comprise medications including antithrombotics, and interventions to modify the vascular risk factors.3 Unfortunately, the optimal management of vascular risk factors is often difficult and complicated because different stroke patients can exhibit diverse demographic characteristics and comorbidities.
Recent advances in information technology (IT) have in turn led to advances in the management of patients, and especially elderly patients with chronic illnesses.4 IT has also been adopted for the management of stroke, and software applications (apps) for mobile devices (especially smartphones) have proven efficacious in the detection of neurological symptoms and in the diagnosis of stroke.5,6,7 The present study conducted a clinical trial to test the feasibility of using a smartphone application (app) for the management of vascular risk factors, which has rarely been studied in patients with stroke. The primary focus of this study was the feasibility of mobile apps, and their efficacy for management of vascular risk factors was also assessed.
The study design was a prospective, single-center, single-arm, open-label clinical trial, and the study was conducted between February 2013 and January 2014. The participants were selected from among patients visiting the outpatient clinic of a tertiary university hospital. They included patients with prior stroke who were aged 20-80 years and had one or more vascular risk factors such as hypertension, diabetes mellitus, smoking, abdominal obesity, or a sedentary lifestyle. Patients who could fully understand the use of an Android-based smartphone were considered as eligible for this study. Patients with severe disability (modified Rankin Scale score>3) were excluded from the study.
At the baseline visit, the status of the patients' baseline risk factors, including blood pressure (BP), waist circumference, weight, and height, were established through medical history-taking, physical examination, and serological tests (Table 1). All patients were requested to visit the outpatient clinic at 90 and 180 days thereafter for repeat testing of BP, waist circumference, weight, and height. The study protocol was approved by the Institutional Review Board (approval KUGH12028) and registered at the Clinical Research Information Service Registry (URL: https://cris.nih.go.kr/cris/en/search/basic_search.jsp; unique identifier: KCT0001045). Written informed consent to participate was obtained from each patient.
A mobile app named 'Korea University Health Monitoring System for Stroke: KUHMS2' was developed for the purpose of patient self-reinforcement through the daily acquisition of risk factor parameters. The details and structure of the app are described in the Supplementary Methods and Fig. 1 in the online-only Data Supplement.
All patients were provided with an instruction manual and instructed regarding the use of KUHMS2 by a trained nurse or physician, and provided with a home BP monitoring device (Omron HEM-7203, Omron Healthcare, Kyoto, Japan). They were asked to record their morning BP data and waist circumference data into KUHMS2 every day. In addition, they were taught how to register information regarding blood sugar, smoking, exercise, and drug adherence. All registered data were synchronized automatically and collected by the server computer at the Data Mining and Information Systems Laboratory via a wireless mobile connection to the Internet. If the registered data exceeded predefined levels, an automated alarm message was sent to the user.
The primary performance figure was adherence, which was defined as the number of days recorded on the KUHMS2 during the study period (range, 1-180 days). The number of days was incremented by 1 day when the patients entered at least one data value for the risk factors on a given day. The secondary end point was the efficacy of the device for managing risk factors, and was evaluated using the achievement rates of the following parameters: target BP, target glycated hemoglobin (HbA1c), target waist circumference, and smoking-free rate. The number of days on which the patient exercised moderately during the previous month and the number of days of adherence to their drug regimen during the previous month were also included as secondary endpoints. The definition of each outcome is given in the Supplementary Methods in the online-only Data Supplement.
The patients were dichotomized according to their level of compliance with entering data into KUHMS2 into compliant and noncompliant groups (with numbers of days with data registration of ≥47 and <47, respectively).
Two major principles of analysis followed on from the purpose of the present trial, which was to test the feasibility of using the developed app in patients with stroke: 1) the data of all patients who entered data into KUHMS2 at least one time were analyzed and 2) data analyzed for secondary endpoints were obtained directly during visits to the outpatient clinic and not by accumulation of data recorded by the patients themselves on the KUHMS2 app.
Data are presented as mean±SD (continuous variables) or n (%) values (categorical variables). The primary endpoint is presented using descriptive statistics. For the secondary endpoints, the McNemar and repeated-measures analysis of variance (ANOVA) were applied. Thereafter, the baseline characteristics were compared between the two groups and serial changes in BP, waist circumference, and body mass index (BMI) were investigated. All statistical analyses were carried out using the Statistical Analysis System software (version 9.2, SAS Institute, Cary, NC, USA), and the threshold for statistical significance was set at p<0.05.
During the study period, 51 patients were screened and 48 patients completed the study protocol; the 3 patients were excluded from the analysis because of lack of follow-up (n=2) or withdrawal of consent (n=1). During the study period, one subject had an episode of transient neurological symptoms without permanent deficit, and brain images revealed no acute lesion. Alarm messages in response to data that exceeded predefined thresholds were sent to 3 patients due to hypoglycemia, to 16 patients due to systolic hypertension [systolic BP (SBP) >160 mm Hg], and to 4 patients due to diastolic hypertension [diastolic BP (DBP) >120 mm Hg].
The patient group comprised 36 males (75.0%) and 12 females aged 52.65±10.25 years. The time between the onset of the index stroke and screening date was 723.0±797.4 days (median, 477 days; interquartile range, 226-1,075 days). The vascular risk factors and baseline measures are presented in Table 1. The only baseline characteristics that differed between the compliant and noncompliant groups were the prevalence of diabetes (29.2% and 70.8%, respectively; p=0.004) and the level of HbA1c.
The number of days with data registration was 60.42±50.17 (median, 47 days; range, 1-180 days) (Table 2). The distribution of the number of days with data registration was skewed to the left (Supplementary Fig. 2 in the online-only Data Supplement). The secondary endpoint was achieved for BP in 33 (68.8%) patients, HbA1c in 13 (54.2%) patients, waist circumference in 37 (77.1%) patients, and nonsmoking in 33 (68.8%) at the final visit. Among these endpoints, significant changes from baseline were found for BP (p=0.031) and HbA1c (p=0.012). Moderate-intensity exercise and drug adherence in the previous month were noted on 10.40±9.92 and 29.25±1.76 days, respectively.
A repeated-measures ANOVA test for SBP, DBP, waist circumference, and BMI revealed a significant effect of time (Fig. 1, Table 3), such that all four parameters were lower at 90 days than at baseline; none of these parameters differed between 90 days and 180 days (Table 3). There was no interaction between measured time and compliance for all parameters (p=0.189 for SBP, p=0.108 for DBP, p=0.636 for waist circumference, and p=0.586 for BMI) (Fig. 1).
The target achievement rates for the measured parameters did not differ significantly between the compliant and noncompliant groups (Table 4).
This clinical trial tested the feasibility of the clinical application of mobile communication technology, based on the concept of a mobile app for the special needs of patients with stroke. The main finding of this study is that despite some hurdles, the developed app for patients with stroke appears to be feasible in the clinical setting, with its implementation resulting in improved risk-factor profiles. The management of vascular risk factors such as hypertension, diabetes, and dyslipidemia is the mainstay of prevention of recurrent stroke or vascular accident in patients with stroke,3 with lifestyle modification being an important aspect of secondary prevention.3 In the present study, despite low compliance, the use of the mobile app was associated with meaningful improvements in risk-factor profiles, paralleling the results of previous studies of ubiquitous health-care systems.8,9,10 Motivation of self-monitoring, lifestyle-modification-supported frequent feedback, or continuing education may explain the improvements in risk-factor profiles among users of health-monitoring systems.10
The application of IT in clinical medicine has recently been associated with beneficial effects in the control of BP and hyperglycemia.9,10,11 Recent guidelines on the management of hypertension recommend the use of home BP measurement using memory-equipped devices, and comment that the use of telemonitoring and smartphone apps for home BP monitoring may be even more advantageous.12 However, the efforts to apply IT to secondary stroke prevention have been limited. Recognition of stroke symptoms, prehospital care, emergency stroke evaluation in the hospital, or neurological examination exemplify IT apps in the stroke field.13 These studies adopted cellular phones (but not smartphones) or specially produced devices for measuring parameters and data collection. In contrast to previous studies, the smartphone was adopted as the primary instrument in the present study. The smartphone provides several advantages over the use of specially designed devices. First, most users of smartphones carry one with them most of the time, and hence they are very familiar with how to handle these devices. Second, various sensors in a smartphone can provide expandability for secondary purposes. For example, mobile-device-based apps currently provide remote consultation,14 telerehabilitation,15 assessments of neurological status,5,16 and diagnosis in these patients.17 Third, ownership of smart devices is rapidly increasing among the elderly population in Korea, and familiarity with these new devices is increasing.18 However, studies using mobile devices for the care of patients with stroke have focused on the role of the mobile device as an aid for the physician rather than for the stroke patient. This limitation could be caused by the stroke population comprising largely of elderly patients who are not familiar with these new devices. In light of this situation, the present study can provide meaningful data on the feasibility of the use of mobile devices by and for patients with stroke.
The primary goal of this study was to test the feasibility of a mobile app for stroke patient care by employing adherence as a primary endpoint, as in previous studies. However, the adherence to data registration, which was the primary endpoint of the study, was disappointing. It may be that the method of data registration was inconvenient to the users in this study, resulting in reduced compliance, since the development of health-care apps has been led by programmers without the involvement of health-care professionals.13 Therefore, improvements to the human-device interface might be expected to improve the compliance rate.
In the present study, risk-factor profiles were shifted toward improvement in all subject groups, although the secondary outcomes did not differ between the compliant and noncompliant groups. The improvement in the risk-factor profile was accomplished during the first 3 months, and was simply maintained over the last half of the trial. The KUHMS2 app might be helpful for controlling the risk factors in various ways, such as by enhancing motivation, changing the method of self-monitoring, and managing risk factors. However, it is possible that the improvement in the risk-factor profile was attributable to the observer effect (Hawthorne effect), which refers to improvements due solely to the subject's knowledge that he or she is being studied.19 Long-term studies are required to prove the existence of a real association between improved risk-factor profiles and a risk-factor monitoring system. Although the long-term effects of a Web-based glucose monitoring system yielded favorable results for controlling glucose,8 the optimal interval for measuring specific parameters needs to be investigated.
In this study the proportion of subjects with diabetic comorbidity was significantly higher in the noncompliant group than in the compliant group. Since blood sugar must be recorded four times per day, subjects with diabetes could regard the use of this system as troublesome. An automatic data transfer system could improve the degree of compliance among its users.
This study was subject to several limitations. First, because the purpose of this study was to test the feasibility of the KUHMS2 app in a clinical situation, the study was designed as a single-arm and open-label clinical trial, which requires cautious interpretation of the results. The lack of a placebo limits the generalizability of the data. Further studies should be designed as controlled clinical trials with both active and control arms. Second, the effects of drug adjustment during the study were not analyzed. The main parameters of this study, such as hypertension and diabetes, are under the influence of medication; however, the parameters that were not related to drug therapy, such as weight and waist circumference, were also improved in a pattern similar to those of BP and blood sugar, which implies an effect not due to the medication. Third, the population included in this study was relatively young and active compared to the general population with stroke. However, there was no difference in age between the compliant and noncompliant groups. Fourth, subjects with severe neurological deficits were not included in this study, limiting the generalizability of the obtained data. For the general use of this system, a more convenient and easy-to-use human-device interface should be developed to compensate for possible user disability. Fifth, the timescale of the study was short, and so the results may have been skewed by observer effects. Long-term effects of the use of mobile devices for risk-factor control should therefore be sought in future studies to validate this approach. Finally, there is no guarantee as to the reliability or reproducibility of the measurements made by individual patients, which is why only the values measured by investigators at the clinic were used rather than those measured and registered on the app by the individual subjects themselves.
In conclusion, the direct application of mobile apps to stroke management and patient care still faces many hurdles. Nevertheless, after the adoption of the KUHMS2 app, the risk profiles of the present patients with stroke moved in a favorable direction, shedding light on its future prospects in the clinical setting.
Figures and Tables
 | Fig. 1Serial changes in systolic blood pressure (SBP), diastolic blood pressure (DBP), waist circumference, and body mass index (BMI). Comparisons were made using repeated-measures ANOVA. A significant effect time was found for SBP, DBP, waist circumference, and BMI at 90 days compared with the respective baseline measures. However, the serial changes in each measure did not differ between the compliant and noncompliant groups. ANOVA: analysis of variance. |
Table 1
Characteristics of the study population

Table 2
Primary and secondary endpoints
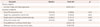
Table 3
Serial changes in SBP, DBP, waist circumference, and BMI
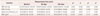
Table 4
Comparison of primary and secondary endpoints between the compliant and noncompliant groups

References
1. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014; 129:e28–e292.
2. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the korean stroke society and clinical research center for stroke. J Stroke. 2013; 15:2–20.

3. Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011; 42:227–276.

4. Touati F, Tabish R. u-Healthcare system: state-of-the-art review and challenges. J Med Syst. 2013; 37:9949.

5. Demaerschalk BM, Vegunta S, Vargas BB, Wu Q, Channer DD, Hentz JG. Reliability of real-time video smartphone for assessing National Institutes of Health Stroke Scale scores in acute stroke patients. Stroke. 2012; 43:3271–3277.

6. Nam HS, Heo J, Kim J, Kim YD, Song TJ, Park E, et al. Development of smartphone application that aids stroke screening and identifying nearby acute stroke care hospitals. Yonsei Med J. 2014; 55:25–29.

7. Demaerschalk BM, Vargas JE, Channer DD, Noble BN, Kiernan TE, Gleason EA, et al. Smartphone teleradiology application is successfully incorporated into a telestroke network environment. Stroke. 2012; 43:3098–3101.

8. Cho JH, Chang SA, Kwon HS, Choi YH, Ko SH, Moon SD, et al. Long-term effect of the Internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care. 2006; 29:2625–2631.

9. Lim S, Kang SM, Shin H, Lee HJ, Won Yoon J, Yu SH, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Diabetes Care. 2011; 34:308–313.

10. Yoo HJ, Park MS, Kim TN, Yang SJ, Cho GJ, Hwang TG, et al. A Ubiquitous Chronic Disease Care system using cellular phones and the internet. Diabet Med. 2009; 26:628–635.

11. Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013; 310:46–56.

12. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013; 34:2159–2219.
13. Nam HS, Park E, Heo JH. Facilitating Stroke Management using Modern Information Technology. J Stroke. 2013; 15:135–143.

14. Kim DK, Yoo SK, Park IC, Choa M, Bae KY, Kim YD, et al. A mobile telemedicine system for remote consultation in cases of acute stroke. J Telemed Telecare. 2009; 15:102–107.

15. Krpič A, Savanovič A, Cikajlo I. Telerehabilitation: remote multimedia-supported assistance and mobile monitoring of balance training outcomes can facilitate the clinical staff's effort. Int J Rehabil Res. 2013; 36:162–171.
16. Shin S, Park E, Lee DH, Lee KJ, Heo JH, Nam HS. An objective pronator drift test application (iPronator) using handheld device. PLoS One. 2012; 7:e41544.

17. Takao H, Murayama Y, Ishibashi T, Karagiozov KL, Abe T. A new support system using a mobile device (smartphone) for diagnostic image display and treatment of stroke. Stroke. 2012; 43:236–239.

18. Korean Internet and Security Agency. 2013 Survey on the smartphone usage [Internet]. Seoul: Korean Internet and Security Agency;2013. updated 2013 Feb 28. cited 2014 Jan. Available from: http://isis.kisa.or.kr/board/index.jsp?pageId=040100&bbsId=7&itemId=801&pageIndex=1.
Supplementary Materials
The online-only Data Supplement is available with this article at http://dx.doi.org/10.3988/jcn.2015.11.2.142.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download