Abstract
Background and Purpose
It has been shown that erythropoietin is neuroprotective in animal models of neurodegenerative diseases including amyotrophic lateral sclerosis (ALS). The aim of this study was to determine the safety and feasibility of repetitive high-dose recombinant human erythropoietin (rhEPO) therapy in ALS patients.
Methods
Two consecutive studies were conducted. We first recruited 26 subjects for an initial single-arm safety study. After a lead-in period of 3 months to assess the disease progression, rhEPO was infused intravenously (35,000 IU) once per month for 3 months, and the subjects were followed for an additional 3 months. The ALS Functional Rating Scale-Revised (ALSFRS-R) was used for clinical assessment. After confirming the safety of rhEPO, 60 subjects were recruited for the second controlled study (rhEPO and control groups), which involved a total of 6 infusions at a rate of 1/month.
Results
There were no serious adverse events in the first study. The mean rate of decline in the ALSFRS-R score was lower during the treatment period than during the lead-in period (mean±SD: 2.6±1.8 and 3.7±2.6, respectively; p=0.02). However, the rate of decline during the subsequent 3 months returned to that observed in the lead-in period. In the second study, the mean rate of decline in ALSFRS-R score was significantly lower in the rhEPO group than in the control group (during months 0-3, 1.8±1.7 vs. 3.1±2.3, p=0.03; during months 4-6, 2.1±2.2 vs. 3.5±2.3, p=0.02).
Amyotrophic lateral sclerosis (ALS) is a rapidly progressing and devastating neurodegenerative disorder that leads to death within 3-5 years of diagnosis.1,2 Despite promising preclinical studies, most treatments have failed to improve clinical outcomes.3 Riluzole, a glutamate antagonist, is currently the sole medication approved by the United States Food and Drug Administration for this disorder,4 but its effects on survival are minimal.5
Erythropoietin (EPO) is a well-known hematopoietic cytokine. In vivo and in vitro studies have shown that it might be neuroprotective in various neurological disorders, including Alzheimer's disease,6,7 Parkinson's disease,8 multiple sclerosis, 9 traumatic head injury,10 schizophrenia,11,12 and ALS.13 EPO not only has neurotrophic features14 but it is also an endogenous agent that protects against neurodegeneration.15 The recent evidence for decreased EPO levels in the cerebrospinal fluid of ALS patients16 supports the idea that extrinsic supplementation with EPO could have a therapeutic effect in ALS.
Several studies of the non-hematopoietic effects of EPO have found no serious adverse events even when EPO was administered as a high-dose infusion.17,18 Therefore, we hypothesized that high-dose EPO is neuroprotective in ALS. As a first step, we performed a safety study in which three consecutive monthly infusions were delivered, and we observed the clinical changes after cessation of the EPO injections. We then performed a second case-control study to determine whether EPO could slow the disease progression over the course of 6 months.
All of the subjects were recruited from Hanyang University Hospital between September, 2006 and February, 2010. The inclusion criteria were as follows: 1) diagnosis of either probable or definite ALS based on the El Escorial criteria of the World Federation of Neurology,19 2) age between 29 and 75 years, 3) ALS Functional Rating Scale-Revised (ALSFRS-R) score of ≥20 points, 4) forced vital capacity of ≥50%, and 5) symptom duration of ≤3 years. The exclusion criteria were the presence of 1) hemoglobin at ≥16 g/dL, 2) a baseline blood pressure of ≥150/90 mm Hg, 3) concomitant inflammatory disorders, 4) malignancies, 5) allergies against recombinant human EPO (rhEPO), and 6) history of myocardial infarction or angina. During the treatment and follow-up periods, complete blood cell counts were assessed monthly, and subjects whose hemoglobin increased to more than 15% above the baseline level were excluded from the study.
The study timelines are presented in Fig. 1. Protocols and consent forms were approved by the Institutional Review Board for Human Investigation of Hanyang University Hospital. All patients provided written informed consent to participate prior to the start of the study, which was conducted according to the provisions of the Helsinki Declaration.
Prior to receiving rhEPO, the natural course of the enrolled patients was assessed over the course of 3 months (lead-in period) using the ALSFRS-R. After this 3 month lead-in period, rhEPO (35,000 IU, Epoetin alpha, Dong-A, Seoul, South Korea) mixed with normal saline (50 mL) was infused intravenously once per month for 3 months. We monitored the ALSFRS-R scores of the subjects for an additional 3 months thereafter to evaluate the effects of discontinuing rhEPO. None of the subjects was allowed to change the dosage of riluzole during the 9 month study period. The ALSFRS-R raters were blinded to both the rhEPO treatment regimen and the clinical history of the subjects.
The primary outcome measures were the differences in the mean changes in the ALSFRS-R scores during the lead-in, treatment, and follow-up periods. The immediate responses and adverse events were evaluated by monitoring the initial 15 subjects at 1 week intervals for 3 months after the initial rhEPO injections using the ALSFRS-R; all individual functional changes after receiving rhEPO were documented.
The safety of the regimen was assessed by evaluating the adverse events related to rhEPO at each visit. Body weight, blood pressure, electrocardiography (ECG) findings, and concomitant medication were documented. Complete blood cell counts, blood urea nitrogen, creatinine, electrolyte, glucose, and liver function tests were checked monthly during the treatment period.
After demonstrating in study I that a regimen comprising three successive monthly bolus infusions of rhEPO was safe and that their effect disappeared after discontinuation, we designed a case-control extended study that comprised a regimen of six injections. The selection criteria and the treatment regimen were the same as for study I, but there was no lead-in period, the experimental group were administered six injections at a rate of one per month (rhEPO group), and a control group was included.
The baseline patient characteristics and demographics were documented at the initial visit. The control and rhEPO groups used the same criteria and were age- and symptom-duration-matched; subjects were included if their delta FS [progression rate was calculated as ratio, 48-ALSFRS-R score at "time of inclusion"/duration from onset to inclusion (month)] was between 0.3 and 1.3.
The efficacy of extended rhEPO treatment was evaluated by comparing the mean changes in the ALSFRS-R scores between the controls and the rhEPO group during the first (0-3 months) and second-half (4-6 months) periods. During the trial, the subjects in the rhEPO group were asked about adverse events, and routine laboratory tests (as described for study I) were carried out.
In study I, as a pilot study, the Wilcoxon signed rank test was used to compare the mean changes in the ALSFRS-R scores during the three periods (lead-in, treatment, and follow-up). In study II, the baseline demographic and clinical characteristics were compared between the two groups using the Mann-Whitney U-test for continuous variables and the chi-square test for categorical variables. A statistically significant change in the ALSFRS-R score between the two groups was determined using the Mann-Whitney U-test. Wilcoxon signed-rank tests were used to assess changes in the laboratory safety parameters.
All reported probability values were two-tailed, and the cutoff for statistical significance was set at p<0.05. Statistical Analysis System (SAS) 9.2 (SAS Institute Inc., Cary, NC, USA) was used for all of the statistical analyses.
The 26 participants included 17 males, and 8 participants had bulbar onset. Their ages ranged from 39 to 73 years (mean=55.2 years), and the mean ALSFRS-R score at 0 months (i.e., immediately before the rhEPO injection) was 34.0 (range, 23-45 points; Supplementary Table 1).
No serious adverse events were noted. There were no significant changes in the patients' laboratory test results or ECG findings. One subject developed a transient palpitation immediately after receiving the second rhEPO dose that lasted for 3 hours, but there were no other significant ECG findings.
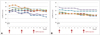
Changes in the ALSFRS-R scores were analyzed. The over-all rate of decline in the ALSFRS-R score decreased during the treatment period (2.6±1.8 vs. 3.7±2.6, mean±SD p=0.02) (Fig. 2A), but reverted to 3.5±2.0 during the follow-up period.
Of the initial 15 subjects who were monitored weekly to evaluate the immediate responses and safety, 2 subjects could not be followed weekly because of travel problems. Among the remaining 13 subjects, 7 experienced subjective functional improvement and an increased sense of well-being that commenced on the second day post-injection. Three subjects exhibited improvements in upper- and lower-limb function (range of motion and motor strength); in addition, two subjects had improved bulbar function and two subjects had improved bulbar and limb function. These changes increased the mean ALSFRS-R score by 1.14 points and appeared to be more pronounced during the first 2 weeks post-rhEPO injection (Fig. 3); however, the effect was not statistically significant. Decreases in fasciculation and drooling, as well as improved respiration, sleep, and muscle tone were also noted. The remaining six subjects did not experience any improvement in ALSFRS-R score, despite reporting improved muscle tone and fasciculation. No acute or chronic serious adverse events were noted in any of the 13 patients.
Sixty ALS subjects were recruited for study II. Three patients (one in the rhEPO group and two in the control group) withdrew prematurely due to travel problems, and another subject in the rhEPO group was excluded because the hemoglobin level had increased to more than 15% above baseline, without other adverse events. Hence, 56 subjects completed the study.
The subjects in the experimental and control groups were matched for age and symptom duration, and their baseline characteristics, such as the symptom duration, delta FS, area of onset, body weight, and use of riluzole, were similar (Table 1). The mean ALSFRS-R scores in the two groups were comparable at baseline, but the mean decrement of ALSFRS-R scores was significantly less in the rhEPO group than in the control group (Fig. 2B). This slowing effect of the disease progression rate continued during the first and second 3 month periods (for months 0-3, 1.8±1.7 vs. 3.1±2.3, p=0.03; for months 4-6, 2.1±2.2 vs. 3.5±2.3, p=0.02).
There were no serious adverse events in the rhEPO group. Two subjects experienced mild headaches, which resolved spontaneously within 2 days. Blood pressure, hemoglobin and platelet counts did not increase in response to the rhEPO injections; other laboratory results also remained within the normal ranges (see follow-up items for safety assessment in Supplementary Table 2).
The administration of a monthly high-dose (35,000 IU) intravenous infusion of rhEPO was safe and feasible in ALS patients. Our results suggest that further studies are warranted to confirm the efficacy of this treatment and to investigate different dose schedules via long-term follow-up.
The dose of rhEPO was chosen on the basis of two previous human EPO trials.17,18 An rhEPO dose of 100,000 IU for 3 days in acute ischemic stroke had no ill effects;17 in acute myocardial infarction, 300 µg of darbepoetin alfa (as a single bolus intravenous infusion), which is equivalent to 60,000 IU of rhEPO, also did not lead to adverse hemodynamic or thrombotic events.18 The dose we employed (35,000 IU) corresponds to one-third of the maximal single dose of rhEPO (i.e., 1,800 IU/kg, 108000 IU in a 60-kg subject). However, due to concerns about the potential thrombotic and hypertensive effects of successive rhEPO treatments, we delivered 3 monthly injections to evaluate the safety in the first study and then extended the duration of the treatment period to 6 months in the second study. Despite its established tolerability and safety, rhEPO is known to have serious adverse effects, including reactive polycythemia,20 thrombocythemia,21 malignant hypertension,22 and thrombotic events.23 However, most complications have been attributed to elevated hematocrit and platelet counts and occur mainly during chronic rhEPO treatment.18
As shown in Fig. 2A (study I), the mean rate of decline of the ALSFRS-R score was significantly lower during the treatment period than during the lead-in period, and this beneficial effect disappeared after the discontinuation of EPO treatment. The results of study II were consistent with those of study I: the clinical progression of ALS was significantly delayed in the rhEPO group compared with the controls. We doubt that these outcomes were the result of increased oxygen delivery. As indicated by Supplementary Table 1 and 2, the successive monthly rhEPO infusions did not increase hemoglobin levels. Moreover, although the data were based on only a few patients, the functional improvements were first noted on day 2 after receiving rhEPO (Fig. 3); it is not feasible for a single bolus of rhEPO to increase the red cell mass within only 2 days.24 Thus, we suggest that rhEPO slows the disease progression via other mechanisms, such as anti-inflammation and anti-apoptotic actions, which have previously been demonstrated in animal models of ALS.13 EPO exhibits various cellular functions, including anti-oxidant,25 anti-inflammatory,26 anti-apoptotic, and neurotrophic effects.27 The cause of the neurodegeneration in ALS appears to be neuronal death following oxidative stress and inflammation, which suggests that EPO could be neuroprotective. In addition, previous studies have shown that EPO can prevent neuronal cell death in animal models of neurodegenerative disorders,26,28,29,30 including ALS.13,31
It is interesting that there was an immediate functional improvement in several subjects, although the presence of a placebo effect cannot be excluded. Since this improvement was maintained for 2 weeks, the interval between injections to 2-3 weeks may be decreased in subsequent studies. Although we did not collect data on the short-term immediate responses in all subjects, this information could help to identify the optimal responders to rhEPO. We were unable to establish the factors underlying the differences between the responders and the non-responders. Future studies should attempt to identify the key features of rhEPO responders versus non-responders since this would make it possible to selectively deliver rhEPO to this subgroup.
In contrast to a previous report,32 we demonstrated the potential efficacy of rhEPO in slowing the progression of ALS, although we cannot completely exclude observer bias; however, the second study enrolled a relatively large number of subjects and confirmed the efficacy of rhEPO using the ALSFRS-R scores. Furthermore, we blinded the scorers to the clinical history of the subjects in order to exclude observer bias. The discrepancy in the clinical results between the previous study32 and the present study might arise from differences between the study protocols; the statistical methods used to evaluate the efficacy were different, and that previous study included fewer subjects. The main limitations of our results were that the study did not have a blinded or randomized design and the lack of a placebo in study II. We plan to confirm the efficacy and safety of rhEPO by increasing the frequency of injections in subsequent studies. In addition, we will seek further evidence of the efficacy of this treatment through randomized, double-blind controlled studies and will assess its impact on survival via long-term follow up.
Figures and Tables
 | Fig. 1Study timelines. Study I: a single-limb safety and efficacy study. Study II: a case-control extended study.  : time to rhEPO injection, : time to rhEPO injection,  : time to clinical assessment, ▵: time to measure ALSFRS-R to evaluate primary outcome. ALSFRS-R: amyotrophic lateral sclerosis Functional Rating Scale-Revised, rhEPO: recombinant human erythropoietin. : time to clinical assessment, ▵: time to measure ALSFRS-R to evaluate primary outcome. ALSFRS-R: amyotrophic lateral sclerosis Functional Rating Scale-Revised, rhEPO: recombinant human erythropoietin. |
 | Fig. 2Efficacy assessment in studies I and II. A (study I): Comparison of the rates of decline (change in the ALSFRS-R scores over 3 months) during the lead-in (-3-0 months prior to 1 months), treatment (0-3 months), and follow-up (4-6 months) periods. During the treatment period, the rate of decline in the ALSFRS-R score decreased. B (study II): Comparison of the rates of decline in the ALSFRS-R scores in the controls and the rhEPO recipients. The mean rate of decline in the ALSFRS-R score was lower for the rhEPO recipients than for the controls. ALSFRS-R: amyotrophic lateral sclerosis Functional Rating Scale-Revised, rhEPO: recombinant human erythropoietin. |
 | Fig. 3Disease progression for 13 subjects as messured by ALSFRS. Of the 13 subjects, 7 displayed sufficient improvements in their functional abilities such that their scores were affected (A), whereas 6 subjects reported only minimal subjective changes that did not affect their scores (B). |
Table 1
Baseline characteristics of the controls and the rhEPO recipients in study II

Data are mean±SD or n values.
*Chi-square test, †Delta FS: the progression rate of the ALSFRS-R (equal to 48-the ALSFRS-R score at the time of inclusion).
ALSFRS-R: amyotrophic lateral sclerosis Functional Rating Scale-Revised, delta FS: difference of ALSFRS-R, rhEPO: recombinant human erythropoietin.
Acknowledgements
This study was supported by a grant from the Korean Health Technology R&D Project, the Ministry for Health, Welfare & Family Affairs, Republic of Korea (no. A120182).
References
1. Cleveland DW, Rothstein JD. From Charcot to Lou Gehrig: deciphering selective motor neuron death in ALS. Nat Rev Neurosci. 2001; 2:806–819.

3. de Carvalho M, Costa J, Swash M. Clinical trials in ALS: a review of the role of clinical and neurophysiological measurements. Amyotroph Lateral Scler Other Motor Neuron Disord. 2005; 6:202–212.

4. Bensimon G, Lacomblez L, Meininger V. ALS/Riluzole Study Group. A controlled trial of riluzole in amyotrophic lateral sclerosis. N Engl J Med. 1994; 330:585–591.

5. Miller RG, Mitchell JD, Lyon M, Moore DH. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Amyotroph Lateral Scler Other Motor Neuron Disord. 2003; 4:191–206.

6. Assaraf MI, Diaz Z, Liberman A, Miller WH Jr, Arvanitakis Z, Li Y, et al. Brain erythropoietin receptor expression in Alzheimer disease and mild cognitive impairment. J Neuropathol Exp Neurol. 2007; 66:389–398.

7. Maiese K, Chong ZZ, Hou J, Shang YC. New strategies for Alzheimer's disease and cognitive impairment. Oxid Med Cell Longev. 2009; 2:279–289.
8. Xue YQ, Zhao LR, Guo WP, Duan WM. Intrastriatal administration of erythropoietin protects dopaminergic neurons and improves neurobehavioral outcome in a rat model of Parkinson's disease. Neuroscience. 2007; 146:1245–1258.

9. Ehrenreich H, Fischer B, Norra C, Schellenberger F, Stender N, Stiefel M, et al. Exploring recombinant human erythropoietin in chronic progressive multiple sclerosis. Brain. 2007; 130(Pt 10):2577–2588.

10. Akdemir Ozisik P, Oruckaptan H, Ozdemir Geyik P, Misirlioglu M, Sargon MF, Kilinc K, et al. Effect of erythropoietin on brain tissue after experimental head trauma in rats. Surg Neurol. 2007; 68:547–555. discussion 555.

11. Ehrenreich H, Hinze-Selch D, Stawicki S, Aust C, Knolle-Veentjer S, Wilms S, et al. Improvement of cognitive functions in chronic schizophrenic patients by recombinant human erythropoietin. Mol Psychiatry. 2007; 12:206–220.

12. Krebs M, Leopold K, Hinzpeter A, Schaefer M. Neuroprotective agents in schizophrenia and affective disorders. Expert Opin Pharmacother. 2006; 7:837–848.

13. Koh SH, Kim Y, Kim HY, Cho GW, Kim KS, Kim SH. Recombinant human erythropoietin suppresses symptom onset and progression of G93A-SOD1 mouse model of ALS by preventing motor neuron death and inflammation. Eur J Neurosci. 2007; 25:1923–1930.

14. Konishi Y, Chui DH, Hirose H, Kunishita T, Tabira T. Trophic effect of erythropoietin and other hematopoietic factors on central cholinergic neurons in vitro and in vivo. Brain Res. 1993; 609:29–35.

15. Ehrenreich H, Aust C, Krampe H, Jahn H, Jacob S, Herrmann M, et al. Erythropoietin: novel approaches to neuroprotection in human brain disease. Metab Brain Dis. 2004; 19:195–206.

16. Janik P, Kwiecinski H, Sokolowska B, Niebroj-Dobosz I. Erythropoietin concentration in serum and cerebrospinal fluid of patients with amyotrophic lateral sclerosis. J Neural Transm. 2010; 117:343–347.

17. Ehrenreich H, Hasselblatt M, Dembowski C, Cepek L, Lewczuk P, Stiefel M, et al. Erythropoietin therapy for acute stroke is both safe and beneficial. Mol Med. 2002; 8:495–505.

18. Lipsic E, van der Meer P, Voors AA, Westenbrink BD, van den Heuvel AF, de Boer HC, et al. A single bolus of a long-acting erythropoietin analogue darbepoetin alfa in patients with acute myocardial infarction: a randomized feasibility and safety study. Cardiovasc Drugs Ther. 2006; 20:135–141.

19. Brooks BR, Miller RG, Swash M, Munsat TL. World Federation of Neurology Research Group on Motor Neuron Diseases. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000; 1:293–299.

20. Henry DH, Bowers P, Romano MT, Provenzano R. Epoetin alfa. Clinical evolution of a pleiotropic cytokine. Arch Intern Med. 2004; 164:262–276.
21. Stohlawetz PJ, Dzirlo L, Hergovich N, Lackner E, Mensik C, Eichler HG, et al. Effects of erythropoietin on platelet reactivity and thrombopoiesis in humans. Blood. 2000; 95:2983–2989.

22. Maschio G. Erythropoietin and systemic hypertension. Nephrol Dial Transplant. 1995; 10:Suppl 2. 74–79.
23. Smith KJ, Bleyer AJ, Little WC, Sane DC. The cardiovascular effects of erythropoietin. Cardiovasc Res. 2003; 59:538–548.

24. Cheung WK, Goon BL, Guilfoyle MC, Wacholtz MC. Pharmacokinetics and pharmacodynamics of recombinant human erythropoietin after single and multiple subcutaneous doses to healthy subjects. Clin Pharmacol Ther. 1998; 64:412–423.

25. Katavetin P, Inagi R, Miyata T, Shao J, Sassa R, Adler S, et al. Erythropoietin induces heme oxygenase-1 expression and attenuates oxidative stress. Biochem Biophys Res Commun. 2007; 359:928–934.

26. Villa P, Bigini P, Mennini T, Agnello D, Laragione T, Cagnotto A, et al. Erythropoietin selectively attenuates cytokine production and inflammation in cerebral ischemia by targeting neuronal apoptosis. J Exp Med. 2003; 198:971–975.

27. Chong ZZ, Kang JQ, Maiese K. Erythropoietin: cytoprotection in vascular and neuronal cells. Curr Drug Targets Cardiovasc Haematol Disord. 2003; 3:141–154.

28. Agnello D, Bigini P, Villa P, Mennini T, Cerami A, Brines ML, et al. Erythropoietin exerts an anti-inflammatory effect on the CNS in a model of experimental autoimmune encephalomyelitis. Brain Res. 2002; 952:128–134.

29. Cho GW, Koh SH, Kim MH, Yoo AR, Noh MY, Oh S, et al. The neuroprotective effect of erythropoietin-transduced human mesenchymal stromal cells in an animal model of ischemic stroke. Brain Res. 2010; 1353:1–13.

30. Genc S, Akhisaroglu M, Kuralay F, Genc K. Erythropoietin restores glutathione peroxidase activity in 1-methyl-4-phenyl-1,2,5,6-tetrahydropyridine-induced neurotoxicity in C57BL mice and stimulates murine astroglial glutathione peroxidase production in vitro. Neurosci Lett. 2002; 321:73–76.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download