Abstract
Background and Purpose
The relationship between contingent negative variation (CNV), which is an event-related potential, and cognition in multiple sclerosis (MS) has not been examined previously. The primary objective of the present study was thus to determine the association between CNV and cognition in a sample of MS patients.
Methods
The subjects of this study comprised 66 MS patients [50 with relapsing-remitting MS (RRMS) and 16 with secondary progressive MS (SPMS)] and 40 matched healthy volunteers. A neuropsychological battery was administered to all of the subjects; CNV recordings were made from the Cz, Fz, and Pz electrodes, and the amplitude and area under the curve (AUC) were measured at each electrode.
Results
RRMS patients exhibited CNVs with lower amplitudes and smaller AUCs than the controls at Pz. SPMS patients exhibited CNVs with lower amplitudes and smaller AUCs than the controls, and CNVs with a smaller amplitude than the RRMS patients at both Cz and Pz. After correcting for multiple comparisons, a lower CNV amplitude at Pz was significantly associated with worse performance on measures of speed of information processing, verbal fluency, verbal learning, and verbal recall.
Reportedly 45-60% of multiple sclerosis (MS) patients suffer from cognitive deficits1 that have a detrimental effect on quality of life2 that is independent of their physical disability.3 The most commonly impaired cognitive domains are memory, processing speed, and executive funtions.4 Cognitive deficits have been reported in all stages of the disease, and early diagnosis of cognitive dysfunction in MS patients is important.5 Research shows that the presence of cognitive dysfunction early in the disease predicts a faster rate of disease progression,6 which may aid patients in their decision-making regarding acceptance of disease-modifying treatments.7
Event-related potentials (ERPs) are evoked potentials that are used primarily in the evaluation of cognitive functioning and are thought to be associated with a person's cognitive activity.8 One of these, the contingent negative variation (CNV), is a negative deviation in the electroencephalography recording induced by an imperative stimulus requiring a motor response following a cue stimulus. It is assumed to represent awareness, attention, decision-making, planning, conation, and readiness for a motor response.9,10 CNV has been used to study dementia, migraine, alcoholism, Parkinson's disease, and schizophrenia.8 Findings from such studies have primarily revealed lower CNV amplitudes in neurological populations when compared to controls. For example, patients with Parkinson's disease exhibit a lower CNV amplitude that rebounds following L-3,4-dihydroxyphenylalanine infusion.9 Similarly, patients with complex partial seizures with and without secondary generalization demonstrate a lower CNV amplitude and a smaller area under the curve (AUC) compared to controls.10 There are also inconsistent findings; for example, early studies revealed lower CNV amplitudes in Alzheimer's disease and in mild cognitive impairment, but a recent study was unable to confirm these findings.11
Despite its promise as a marker for cognitive dysfunction in other neurological disorders, there has been no study of the association between CNV and multiple domains of cognition in MS. The primary aim of this study was therefore to confirm the differences in CNV between MS patients and controls. We hypothesized that MS patients would demonstrate a lower CNV amplitude and a smaller AUC when compared to normal controls. A secondary aim was to determine the association between CNV and neuropsychological test performance among patients with MS. We hypothesized that a lower CNV amplitude and smaller AUC would be associated with worse performance on neuropsychological tests.
Patients with definite MS diagnosed according to the revised McDonald criteria12 were enrolled consecutively during a 3-month period. All of the patients were followed at the Demyelinating Diseases Outpatient Clinic at Dokuz Eylul University Hospital, Izmir, Turkey. Patients with the relapsing-remitting and secondary progressive MS types (RRMS and SPMS, respectively) aged 17-55 years were included after evaluation by two neurologists (E.I. and S.O.) with experience in demyelinating diseases. Patients with a history of systemic, psychiatric, or neurological diseases other than MS, such as hypertension, diabetes mellitus, myocardial infarction, major depression, or psychosis, a history of concussion with loss of consciousness of more than 20 min, and taking antidepressant, antipsychotic, or sedative medications, or with a history of exacerbation or corticosteroid use in the preceding 4 weeks were not included. The Expanded Disability Status Scale (EDSS) was used to assess disability.13 Healthy controls were enrolled by verbal advertising to patients' relatives during the patient enrollment process; Department of Neurology staff, hospital employees, residents, and medical students were also recruited. All possible candidates were interviewed by the first author to ascertain their eligibility and potential age and education match with the enrolled patients. The exclusion criteria for the controls were a history of systemic, psychiatric, or neurological diseases such as hypertension, diabetes mellitus, myocardial infarction, major depression, psychosis, Parkinson's disease, dementia/cognitive impairment, or epilepsy, a history of concussion with loss of consciousness of more than 20 min, and taking antidepressant, antipsychotic, or sedative medications. Neither the patients nor the healthy controls received reimbursement for their participation in the study.
Each of the subjects provided written informed consent to participate prior to the commencement of the study. The study was approved by the Institutional Review Board of Dokuz Eylul University. Approval for the analysis of de-identified data was given by the University of Missouri-Kansas City Office of Research Services.
Cognitive performance was assessed using a battery of tests that have been validated for use in Turkish subjects and that measure information processing speed, memory, and executive functioning;14,15,16 these domains were chosen for the investigation because they are the most commonly impacted areas of cognition in MS.17
The oral version of the Paced Serial Addition Test (PASAT) assesses attention and speed of information processing. Participants were presented aurally with a series of 61 single-digit numbers every 3 s, and were asked to add each number that they heard to the preceding number. The participant's score was taken as the number of correct responses, with a maximum score of 60.15
The Stroop Test assesses processing speed and executive functions.18 Participants performed the following three tasks: 1) to quickly name the colors of a string of rectangles, 2) to read the names of three colors (blue, red, and green) printed in black ink, and 3) to state the color of the inks that differed from the names of the colors. A speed score corresponds to the average time for each of the first two noninterference tasks,19 and an interference score is calculated by subtracting the time for the third task from the time measured for the second task. This test was validated for the Turkish population by Umaç.14
The Controlled Oral Word Association Test (COWAT) measures executive functioning and verbal fluency.20 In the Turkish version, subjects are asked to produce as many words beginning with K, A, and S in 60 s for each letter. Proper names, numbers, and multiple forms of the same word were not accepted in the present study, and the dependent variable was the sum of all of the accepted words across the three trials.14
The Rey Auditory Verbal Learning Test (RAVLT) measures verbal learning and memory. The RAVLT includes 5 learning trials during which a 15-word list is read aloud to the participant. After each trial, the participant was asked to say all of the words that they could remember. The dependent variables in the present study were the number of words recalled over the learning trials and the number of words recalled after a 20-min delay.14
Contingent negative variation recordings were made using an evoked-potential/EMG recording system (Neuropack MEB-2200 K, Nihon Kohden, Tokyo, Japan) at the Neurophysiology Laboratory, Department of Neurology, Dokuz Eylul University on the same day that the patient received the neuropsychological test battery. Participants were seated in a reclining armchair in a dimly lit and quiet room with optimal room temperature. They were asked to avoid blinking, swallowing, chewing, yawning, and any facial movement, and to make any absolutely necessary such movements only after a motor response. EEG was recorded by using silver/silver-chloride electrodes placed at Fz, Cz, and Pz and referenced to linked mastoids. Impedances were kept below 5 kΩ and the bandpass filter was set at 0.03-100 Hz. All subjects exhibited at least 20 good trials. The CNV paradigm consisted of a warning stimulus (S1, comprising a pure tone of 1,000 Hz at 75 dB SPL and of 50 ms duration) followed 2 s later by an imperative stimulus (S2, comprising a series of light flashes from LED goggles). The participants were asked to interrupt the S2 stimulus by pressing a button with their dominant hand (or nondominant hand if it had better motor control). Trials were automatically excluded if the button was pressed between two stimuli. Intertrial intervals varied randomly from 5 to 10 s. Trials with artifact, false-response errors, or omissions were automatically rejected from the ERP averaging.
Contingent negative variation amplitude was measured from the highest point between 500 ms after S1 and 200 ms prior to S2, and referenced to the baseline tracing before S1. The AUC of the response was calculated automatically using QP-213BK Event Related Potentials Software (Nihon Kohden, Tokyo, Japan) to measure the area between the negative deflection and the baseline (Fig. 1).22 Amplitude and AUC measures of the CNV wave from the Fz, Cz, and Pz electrodes were the dependent variables for the present study.
Statistical analyses were performed using SPSS for Windows (release 19.0, SPSS Inc., Chicago, IL, USA). Nonparametric multivariate analysis of variance (MANOVA) was used to compare CNV and neuropsychological measures between the groups to reduce the risk of a type I error. This approach is consistent with our prior work and is preferred over parametric approaches when there is a violation of the equal covariance matrix assumption.23,24 Follow-up Kruskal-Wallis and Mann-Whitney U tests were conducted as appropriate to further examine between-group differences. The cutoff for statistical significance for these analyses was set at p<0.05.
Correlations between neuropsychological and neurophysiological measures were determined using the Pearson r statistic. To reduce the number of correlational analyses, only CNV and neuropsychological measures that differed significantly between MS patients and controls were examined. Spearman rho correlations were employed if violations of parametric statistics were uncovered. Bonferroni correction was employed to reduce the risk of a type I error in these correlational analyses, which meant that results were considered statistically significant at p<0.002. Follow-up partial correlations controlling for disease characteristics were conducted to ensure that the obtained correlations were not due to secondary factors (e.g., depression) or general disease progression.
In total, 66 patients (50 RRMS, 16 SPMS) were included in the study. The mean age and years of education of the RRMS patients (33 females) were 39.52±10.41 years (mean±SD) and 12.34±3.19 years, respectively; these values for the SPMS patients (11 females) were 43.81±7.47 years and 12.69±2.82 years, respectively. As expected, SPMS patients had a longer disease course (13.94±5.80 years vs. 9.08±6.65 years; [t(64)=2.62, p<0.05] and higher EDSS scores [5.78±1.08 vs. 1.83±1.07; t(64)=12.86, p<0.001] than RRMS patients. The healthy controls (n=40; 27 females) were 37.03±10.43 years old and had 12.78±3.38 years of education. Age, education, and gender did not differ significantly between the healthy controls, RRMS patients, and SPMS patients.
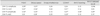
We hypothesized that the MS patients would demonstrate a lower CNV amplitude and smaller AUC relative to healthy controls. Nonparametric MANOVA revealed significant CNV differences between RRMS patients, SPMS patients, and healthy controls (χ2=50.40, df=15, p<0.005). Table 1 lists the descriptive and between-group differences for CNV amplitude and AUC at Fz, Cz, and Pz. RRMS patients exhibited a lower CNV amplitude and smaller AUC than the controls at Pz. SPMS patients exhibited a lower CNV amplitude and smaller AUC than the controls at both Cz and Pz; they also exhibited a lower CNV amplitude than the RRMS patients at both of these locations.
Stepwise logistic regression was conducted with disease course entered as the dependent variable and CNV values as covariates. CNV indicators shown to be significantly different between SPMS and RRMS patients were entered in block one. Only the CNV amplitude at Cz predicted unique variance in the disease course (p=0.008). A receiver operating characteristic curve revealed a high level of sensitivity to SPMS as 0.94 when the Cz amplitude was <11.15 µV, but its specificity was only 0.50.
To reduce the number of correlational analyses, we decided a priori to only examine CNV variables that differentiated between MS patients and controls. Higher EDSS scores were associated with a lower amplitude and smaller AUC at Cz (r=-0.40, p=0.001 and r=-0.27, p=0.028, respectively). Longer disease duration was associated with a lower Cz amplitude (r=-0.28, p=0.021), and older MS patients exhibited a smaller AUC at Pz (r=0.31, p=0.012). Patients' scores on the BDI, and for education and sex were not significantly associated with CNV measures.
We hypothesized that MS patients with a lower CNV amplitude and smaller AUC would perform worse in the neuropsychological tests. Table 2 provides descriptive statistics for the neuropsychological test performance according to the group. As expected, MS patients performed significantly worse on measures of information processing speed, memory, and executive functioning. Table 3 lists the correlations between CNV and neuropsychological measures. Increased amplitude at Pz was significantly associated with better scores in the PASAT, COWAT, and RAVLT after correcting for multiple comparisons. Increased amplitude at Cz was associated with faster processing speed in the PASAT and Stroop Test after correcting for multiple comparisons. Partial correlations controlling for EDSS, disease duration, BDI score, and age continued to show significant associations between CNV Pz amplitude and PASAT (r=0.41, p=0.001), COWAT (r=0.39, p=0.002), RAVLT Learning (r=0.39, p=0.002), and RAVLT Delayed Recall (r=0.40, p=0.002). Partial correlations controlling for EDSS, disease duration, BDI score, and age continued to show a significant association between CNV Cz amplitude and PASAT (r=0.29, p=0.024).
There has been growing interest in radiological and neurophysiological correlates of cognitive dysfunction in MS. Reports on other ERPs such as P300 or mismatch negativity in MS patients can be found in the literature,25,26,27 but there has been a paucity of research on CNV in this patient group.28 To the best of our knowledge, this is the first study to examine the association between CNV and neuropsychological functioning in MS patients, and the first to examine CNV differences between RRMS and SPMS patients. This study yielded some important findings and confirmed significant differences in the CNV amplitude and AUC between MS patients and controls for measurements at the Cz and Pz electrodes. The CNV amplitude was lower and the AUC was smaller in RRMS patients than in controls at Pz. SPMS patients exhibited a lower CNV amplitude and smaller AUC than controls at Cz and Pz; they also exhibited a lower CNV amplitude than RRMS patients at Cz and Pz. Moreover, significant correlations were found between neuropsychological test performance and amplitude at Cz and Pz, even after correcting for multiple comparisons and disease characteristics.
A recent study in which an attentional visual-spatial task was implemented with Posner's central cue paradigm to explore benign MS patients (BMS), RRMS patients, and healthy controls found CNV changes in patients with MS.29 Specifically, BMS patients exhibited lower CNV amplitudes at central and parietal sites compared to controls. Interestingly, there was higher negative amplitude in the central phase of CNV in RRMS patients at frontocentral sites compared to controls. The authors suggested that this could reflect reduced activation of orientation and cue-preparation mechanisms in BMS patients and increased attention at the beginning of the preparation stage or greater task motivation in RRMS patients. These findings partially contrast with the results obtained in the present study, which revealed no significant differences between RRMS patients and controls at frontal and central sites. However, our RRMS patients had a longer disease course and slightly lower EDSS score than the patients in their study, suggesting the presence of differences between the patient characteristics and that some of our RRMS patients might be similar to the BMS patients in the study of Gonzalez-Rosa et al.29 Furthermore, other limiting factors such as methodological differences (differences in stimulus paradigms, interstimulus durations, or in the methods used to analyze waveforms), and a small number of patients in the latter study may account for the discrepant findings. In another recent study, Vázquez-Marrufo et al.30 reported that CNV amplitudes were significantly lower in RRMS patients than in controls in central and frontal electrodes during an Attention Network Test using central and spatial cueing; they found a trend toward decreased amplitude that did not reach to statistical significance when a cue was not used. They interpreted these results as impairment in the central cueing mechanism and also a worse orienting response.30
The amplitude and AUC values were preserved at the Fz and Cz electrodes in RRMS patients, but significantly lower values at Cz were found for SPMS patients. It is somewhat difficult to compare our findings with those of other studies because we did not use a special paradigm dedicated to attention. Our results showing preserved CNV values in frontocentral electrodes in RRMS patients could be due to secondary increases in frontal activation that compensate for MS-related functional and/or structural abnormalities. These cognitive compensatory mechanisms were suggested by Bonnet et al.31 and have been described using functional MRI (fMRI) in early MS and RRMS patients, revealing additional activation of cerebral structures such as the prefrontal, dorsofrontal, and medial frontal cortices.32,33 It is postulated that this increased involvement of the frontal areas helps patients to compensate for the cognitive declines associated with the progression of MS. Nevertheless, effective compensation seems to be limited by the accumulation of tissue damage and the introduction of highly demanding cognitive tasks.34 The limited frontal compensatory cortical activation seen in fMRI studies could explain why the CNV measures differed significantly in each group between the Pz electrode, which is located posteriorly, and the Fz electrode. Put simply, our findings may show a posterior-to-anterior signal deterioration in CNV among MS patients as their disease progresses; however, an insensitivity of CNV to frontal pathology in MS could also be argued.
Another possible explanation for the lower CNV amplitude and smaller AUC could be widespread cortical and subcortical gray-matter volume loss along with disconnection between the generators of CNV. As a sensory gateway with multiple efferent and afferent connections, the thalamus may play an especially important role. Intracranial recordings and fMRI studies conducted with simultaneous CNV recordings show widespread generators of the CNV involving both cortical and subcortical areas, including the primary sensorimotor area, supplementary motor area, cingulate gyrus, orbitofrontal cortex, prefrontal area, dorsolateral and orbital prefrontal cortices, premotor and motor cortices, temporal cortex, amygdalohippocampal complex, insula, posterior parietal cortices, basal ganglia, and thalamus.35,36 There is a well-known relationship between thalamic pathology in early MS,37,38 subtle damage to afferent projections to the thalamus with effects on cognitive status,39,40 and thalamic atrophy in SPMS.41 It is possible that the lower posterior CNV amplitude observed in MS reflects damage to the thalamus or its projections that requires compensation and additional cortical activity in the frontal systems.
Impaired attentional cue-orienting mechanisms were suggested in different stages of MS,28 raising the possibility that CNV findings vary with the paradigm and stage of the disease. A lower CNV amplitude and a smaller AUC at the Cz electrode may indicate failure of the compensatory mechanisms as the disease progresses. Therefore CNV, which is a relatively inexpensive and easy test to perform, should be further explored as a measure of disease progression in MS. In addition, logistic regression analysis revealed that the lower CNV amplitudes measured at the Cz electrode were associated with the SPMS course. However, caution is necessary regarding the utility of this parameter for predicting the disease course due to limitations such as the smallness of the sample. Future confirmative studies with larger samples and more scalp coverage are needed.
As expected, MS patients performed worse than the controls in neuropsychological tests. The neuropsychological test battery employed in the present study focused on the frontal and medial temporal systems, which are known to be differentially impacted in MS. Furthermore, the cognitive test battery employed herein would not fully address the functional and structural integrity of the brain regions located near the Cz and Pz electrodes. Future structural neuroimaging studies should be conducted in conjunction with CVN to shed more light on the neuroanatomical and functional underpinnings of the present findings.
Two previous studies have analyzed CNV in MS patients using attention-specific paradigms. To the best of our knowledge, the present study is the first to examine the association between CNV and different domains of neuropsychological functioning in MS patients. The findings implicate a possible future role of CNV in assessing the mechanisms underlying cognitive impairment and disease progression. The results showed moderate-to-strong correlations between CNV and measures of processing speed, verbal fluency, and memory. These findings support possible value for CNV in detecting and better understanding the mechanisms underlying the cognitive dysfunction in MS. However, certain limitations must first be considered. First, the present sample of SPMS patients was small. Second, CNV was measured from only three electrodes rather than with extensive scalp coverage; however, the method used would be more reflective of a potential daily clinical use of CNV as a potential screen for cognitive dysfunction and disease progression, rather than using more complex CNV paradigms and extensive coverage, which would require labor-intensive analysis and higher skill levels that may not be widely available. Third, CNV is not routinely used in clinical practice for MS, and its sensitivity, validity, and normative values have not been confirmed. Fourth, this study was not prospective, and as such its findings are limited with regard to changes in CNV associated with disease progression. Fifth, we did not perform concomitant MRI studies during the study period for each patient to correlate CNV findings with lesion loads. Future prospective studies that employ greater scalp coverage and structural imaging should be conducted with the aim of determining the optimal array of coverage for detecting cognitive dysfunction, correlations of CNV and neuroimaging characteristics, and disease progression in MS.
Larger prospective studies with discriminant analysis should also be conducted to determine whether measurements of CNV amplitudes at Pz and Cz truly hold promise as an objective tool with which to differentiate between SPMS and RRMS patients or to evaluate disease progression in MS. Moreover, the decreased amplitude at the Pz electrode was significantly correlated with cognitive impairment in MS patients, even after correcting for multiple comparisons and removing the variance associated with disease-specific factors. Integrating these findings with structural and other forms of functional data may lead to an improved understanding of the neural mechanisms responsible for cognitive decline and disease progression in MS. Future prospective studies with larger samples and wider scalp coverage that correlate CNV with neuroimaging data are needed to confirm and extend these findings.
Figures and Tables
 | Fig. 1CNV recording of a patient with RRMS. Red marks (x) are reference points used for the AUC calculation. AUC: area under the curve, CNV: contingent negative variation, RRMS: relapsing-remitting multiple sclerosis. |
Table 1
Group differences in CNV between health controls, RRMS patients, and SPMS patients

Different lettered subscripts beside mean rank variables indicate significant group differences (Mann-Whitney tests, p<0.05).
AUC: area under the curve, CNV: contingent negative variation, n.s.: not significant, RRMS: relapsing-remitting multiple sclerosis, SPMS: secondary progressive multiple sclerosis.
Table 2
MS patients perform worse than controls on measures of speeded information processing, memory, and executive functioning

References
1. Rao SM, Leo GJ, Bernardin L, Unverzagt F. Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction. Neurology. 1991; 41:685–691.

2. Rao SM, Leo GJ, Ellington L, Nauertz T, Bernardin L, Unverzagt F. Cognitive dysfunction in multiple sclerosis. II. Impact on employment and social functioning. Neurology. 1991; 41:692–696.

3. Amato MP, Ponziani G, Siracusa G, Sorbi S. Cognitive dysfunction in early-onset multiple sclerosis: a reappraisal after 10 years. Arch Neurol. 2001; 58:1602–1606.

4. Bobholz JA, Rao SM. Cognitive dysfunction in multiple sclerosis: a review of recent developments. Curr Opin Neurol. 2003; 16:283–288.

5. Wishart H, Sharpe D. Neuropsychological aspects of multiple sclerosis: a quantitative review. J Clin Exp Neuropsychol. 1997; 19:810–824.

6. Deloire M, Ruet A, Hamel D, Bonnet M, Brochet B. Early cognitive impairment in multiple sclerosis predicts disability outcome several years later. Mult Scler. 2010; 16:581–587.

7. Benedict RH, Fischer JS, Archibald CJ, Arnett PA, Beatty WW, Bobholz J, et al. Minimal neuropsychological assessment of MS patients: a consensus approach. Clin Neuropsychol. 2002; 16:381–397.

8. Oken BS. Endogenous event-related potentials. In : Chiappa KH, editor. Evoked Potentials in Clinical Medicine. 2nd ed. New York, NY: Raven Press;1990. p. 563–592.
9. Oishi M, Mochizuki Y, Du C, Takasu T. Contingent negative variation and movement-related cortical potentials in parkinsonism. Electroencephalogr Clin Neurophysiol. 1995; 95:346–349.

10. Drake ME Jr, Weate SJ, Newell SA. Contingent negative variation in epilepsy. Seizure. 1997; 6:297–301.

11. van Deursen JA, Vuurman EF, Smits LL, Verhey FR, Riedel WJ. Response speed, contingent negative variation and P300 in Alzheimer's disease and MCI. Brain Cogn. 2009; 69:592–599.

12. Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011; 69:292–302.

13. Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983; 33:1444–1452.

14. Umaç A. Normal deneklerde frontal hasarlara duyarlı bazı testlerde performansa yaş ve eğitimin etkisi [dissertation]. İstanbul: İstanbul Üniversitesi;1997.
15. Ozakbas S, Ormeci B, Akdede BB, Alptekin K, Idiman E. Utilization of the auditory consonant trigram test to screen for cognitive impairment in patients with multiple sclerosis: comparison with the paced auditory serial addition test. Mult Scler. 2004; 10:686–689.

16. Hisli N. Beck Depresyon Envanteri'nin üniversite öğrencileri için geçerliği, güvenirliği. Psikoloji Dergisi. 1989; 7:3–13.
17. Winkelmann A, Engel C, Apel A, Zettl UK. Cognitive impairment in multiple sclerosis. J Neurol. 2007; 254:Suppl 2. II35–II42.

19. Denney DR, Lynch SG. The impact of multiple sclerosis on patients' performance on the Stroop Test: processing speed versus interference. J Int Neuropsychol Soc. 2009; 15:451–458.

20. Benton AL. Development of a multilingual aphasia battery. Progress and problems. J Neurol Sci. 1969; 9:39–48.
21. Mohr DC, Goodkin DE, Likosky W, Beutler L, Gatto N, Langan MK. Identification of Beck Depression Inventory items related to multiple sclerosis. J Behav Med. 1997; 20:407–414.
22. Ashton H, Marsh VR, Millman JE, Rawlins MD, Telford R, Thompson JW. Biphasic dose-related responses of the CNV (contingent negative variation) to I.V. nicotine in man. Br J Clin Pharmacol. 1980; 10:579–589.

23. Bruce JM, Harrington CJ, Foster S, Westervelt HJ. Common blood laboratory values are associated with cognition among older inpatients referred for neuropsychological testing. Clin Neuropsychol. 2009; 23:909–925.

24. Finch H. Comparison of the Performance of Nonparametric and Parametric MANOVA Test Statistics when Assumptions Are Violated. Methodology (Gott). 2007; 1:27–38.

25. Kiiski H, Reilly RB, Lonergan R, Kelly S, O'Brien M, Kinsella K, et al. Change in PASAT performance correlates with change in P3 ERP amplitude over a 12-month period in multiple sclerosis patients. J Neurol Sci. 2011; 305:45–52.

26. Matas CG, Matas SL, Oliveira CR, Gonçalves IC. Auditory evoked potentials and multiple sclerosis. Arq Neuropsiquiatr. 2010; 68:528–534.

27. Ivica N, Titlic M, Pavelin S. P300 wave changes in patients with multiple sclerosis. Acta Inform Med. 2013; 21:205–207.

28. Aminoff JC, Goodin DS. Long-latency cerebral event-related potentials in multiple sclerosis. J Clin Neurophysiol. 2001; 18:372–377.

29. Gonzalez-Rosa JJ, Vazquez-Marrufo M, Vaquero E, Duque P, Borges M, Gomez-Gonzalez CM, et al. Cluster analysis of behavioural and event-related potentials during a contingent negative variation paradigm in remitting-relapsing and benign forms of multiple sclerosis. BMC Neurol. 2011; 11:64.

30. Vázquez-Marrufo M, Galvao-Carmona A, González-Rosa JJ, Hidalgo-Muñoz AR, Borges M, Ruiz-Peña JL, et al. Neural correlates of alerting and orienting impairment in multiple sclerosis patients. PLoS One. 2014; 9:e97226.

31. Bonnet MC, Deloire MS, Salort E, Dousset V, Petry KG, Brochet B, et al. Evidence of cognitive compensation associated with educational level in early relapsing-remitting multiple sclerosis. J Neurol Sci. 2006; 251:23–28.

32. Staffen W, Mair A, Zauner H, Unterrainer J, Niederhofer H, Kutzelnigg A, et al. Cognitive function and fMRI in patients with multiple sclerosis: evidence for compensatory cortical activation during an attention task. Brain. 2002; 125(Pt 6):1275–1282.

33. Forn C, Barros-Loscertales A, Escudero J, Benlloch V, Campos S, Antònia Parcet M, et al. Compensatory activations in patients with multiple sclerosis during preserved performance on the auditory N-back task. Hum Brain Mapp. 2007; 28:424–430.

34. Bonnet MC, Allard M, Dilharreguy B, Deloire M, Petry KG, Brochet B. Cognitive compensation failure in multiple sclerosis. Neurology. 2010; 75:1241–1248.

35. Bares M, Rektor I, Kanovský P, Streitová H. Cortical and subcortical distribution of middle and long latency auditory and visual evoked potentials in a cognitive (CNV) paradigm. Clin Neurophysiol. 2003; 114:2447–2460.

36. Nagai Y, Critchley HD, Featherstone E, Fenwick PB, Trimble MR, Dolan RJ. Brain activity relating to the contingent negative variation: an fMRI investigation. Neuroimage. 2004; 21:1232–1241.

37. Minagar A, Barnett MH, Benedict RH, Pelletier D, Pirko I, Sahraian MA, et al. The thalamus and multiple sclerosis: modern views on pathologic, imaging, and clinical aspects. Neurology. 2013; 80:210–219.

38. Brass SD, Benedict RH, Weinstock-Guttman B, Munschauer F, Bakshi R. Cognitive impairment is associated with subcortical magnetic resonance imaging grey matter T2 hypointensity in multiple sclerosis. Mult Scler. 2006; 12:437–444.

39. Batista S, Zivadinov R, Hoogs M, Bergsland N, Heininen-Brown M, Dwyer MG, et al. Basal ganglia, thalamus and neocortical atrophy predicting slowed cognitive processing in multiple sclerosis. J Neurol. 2012; 259:139–146.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download