Abstract
Background
Paraneoplastic neurological syndromes are rare, and although they are frequently associated with gynecological malignancies, cervical cancer is a rare cause. The symptoms of anti-Ma2 encephalitis are diverse and often present prior to the diagnosis of malignancy.
Case Report
We report a case of a 37-year-old woman with a history of cervical cancer presenting with unexplained weight gain and vertical supranuclear gaze palsy. Magnetic resonance imaging of the brain revealed lesions within the bilateral hypothalami and midbrain. Anti-Ma2 antibodies were eventually found in the serum, prompting a search for malignancy. Recurrent metastatic cervical cancer was found in the retroperitoneal lymph nodes.
Conclusions
This is the first report of cervical cancer in association with anti-Ma2 encephalitis, and highlights the need for a high degree of suspicion in patients with a cancer history presenting with neurological symptoms. The symptoms associated with anti-Ma2 encephalitis are diverse and typically precede the diagnosis of cancer in patients, and should trigger a search for an underlying malignancy.
Paraneoplastic neurological syndromes (PNS) are rare regardless of the causal cancer, and while gynecological malignancies (particularly ovarian carcinoma) are the most commonly associated tumors, cervical cancer is a very rare cause. Most PNS present before the discovery of the malignancy, often allowing for diagnosis of a potentially curable neoplasm. Moreover, the neurological syndrome may be far more disabling than the cancer itself. The initial features of PNS can be diverse, and making a diagnosis typically depends on the discovery of "paraneoplastic antibodies" and their immunological target. Ma2 proteins are widely distributed throughout the normal brain,1 and anti-Ma2 encephalitis can present with various clinical symptoms. We report herein on a female patient with hypothalamic and brainstem encephalitis, and anti-Ma2 antibodies associated with recurrent metastatic squamous cell carcinoma of the cervix.
A 37-year-old woman (gravida 3, para 3) with a history of type 2 diabetes presented with the acute onset of difficulty looking downward. She described that this predominantly occurred during driving, noticing that when she looked up into the rear view mirror she was unable to look back down to the dashboard. Other complaints included new daily holocephalic headaches and a 30-pound weight gain over 3 months, without an obvious increase in appetite. She reported fatigue, but no excessive sleepiness. Her medical history was significant for stage IB1 squamous cell carcinoma of the cervix diagnosed 7 years prior to the onset of neurological symptoms. She was treated with a radical hysterectomy and pelvic lymphadenectomy. Pathology revealed a poorly differentiated tumor with a greatest thickness of 1.5 cm and a total cervical thickness of 1.7 cm, and extensive lymphovascular invasion. She received pelvic radiation with weekly cisplatin followed by brachytherapy, and was then lost to follow-up.
Neurological complaints began approximately 7 years after completing the above-mentioned treatment. Comprehensive neurological examination was normal with the exception of vertical supranuclear gaze palsy with absent voluntary vertical saccades or pursuit. Downward gaze was more affected than upward gaze. Oculocephalic maneuvers showed full ocular range of motion. Horizontal gaze was unaffected. Brain magnetic resonance imaging (MRI) revealed T2 hyperintensities with contrast enhancement of the hypothalami extending into the mesial temporal lobes and midbrain (Fig. 1). Significant laboratory studies included an elevated serum alkaline phosphatase level of 138 U/L (normal range, 39-117 U/L) and an erythrocyte sedimentation rate of 21 mm/h. Cerebrospinal fluid (CSF) exhibited a white blood cell count of 15/µL, a red blood cell count of 10/µL, a protein level of 31 mg/dL (normal range, 15-45 mg/dL), and a glucose level of 106 mg/dL (normal range, 40-80 mg/dL). Cytological analysis of the CSF yielded no malignant cells. Commercial paraneoplastic antibody testing revealed that the following antibodies were absent from the serum and CSF: antineuronal nuclear autoantibody types 1, 2, and 3; Purkinje cell cytoplasmic autoantibody types 1, 2, and Tr; amphiphysin; antiglial nuclear antibody type 1; and collapsin response-mediator protein 5 IgG. Serum striational (striated muscle), P/Q-type calcium channel, N-type calcium channel, acetylcholine receptor (neuronal and muscle), and voltage-gated potassium channel antibodies were also absent. Ma antibodies were absent in initial serum and CSF samples evaluated at a separate commercial laboratory using immunoblot testing (reference value: negative). Anti-Ma2 antibodies were eventually found in the serum during an evaluation at an independent laboratory using immunofluorescence (reference value: negative).
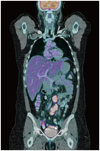
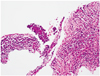
These findings prompted a systemic search for an occult cancer versus a recurrence of her cervical cancer. Positron-emission tomography (PET) and computed tomography (CT) scans revealed enlarged retroperitoneal and common iliac lymph nodes with avid 18-F fluoro-2-deoxyglucose uptake, consistent with an active malignancy (Fig. 2). During staging the patient received intravenous corticosteroids (1 g of methylprednisolone per day for 3 days). Her headaches resolved without a significant change in her vertical gaze paresis. She subsequently underwent a retroperitoneal lymph-node biopsy that revealed squamous cell carcinoma, consistent with her known malignancy of the cervix (Fig. 3). She was treated with docetaxel and carboplatin along with directed radiation therapy to the involved lymph nodes. Follow-up MRI of the brain revealed significant improvement of the previously observed abnormal contrast enhancement and T2 hyperintensity (Fig. 1), although her neurological findings were unchanged. Follow-up PET/CT revealed new metabolically active retroperitoneal lymph nodes. The patient elected to enroll in a phase I study with the multitargeted kinase inhibitor crizotinib. She completed two cycles of the study protocol, with subsequent progression of disease and evidence of new liver and lung metastases. The patient died 3 months later, 1 year after the presentation of neurological deficits. No autopsy was performed.
We report herein a patient with recurrent squamous cell carcinoma of the cervix with Ma2-antibody-positive encephalitis characterized predominantly by vertical supranuclear gaze palsy and inexplicable weight gain. While hypothalamic obesity and brainstem encephalitis are not considered "classical" PNS, this combination is suggestive of an anti-Ma2-positive PNS. Accordingly, paraneoplastic antibodies were searched for in the serum and eventually found. Although this case fits a "definite" PNS as defined by Graus et al.,2 an unequivocal diagnosis can only be made by finding the Ma2 antigen in the patient's tumor. This case is unusual not only due to the rarity of cervical cancer being reported in association with PNS, but also because it was associated with recurrent disease.
The syndrome was first described by Ahern et al.3 in 1994. Anti-Ma2 antibodies were originally reported in a small cohort of predominantly young men presenting with limbic or brainstem encephalitis and testicular cancer.1 Anti-Ma2 antibodies have subsequently been reported with increased frequency in women in association with a variety of tumor types.4,5 Dalmau et al.4 reported on 38 patients with anti-Ma2-associated encephalitis; more than 95% of these patients exhibited involvement of the limbic system, diencephalon, or brainstem, and most of them had combined areas of involvement. Most (60%) of the patients with brainstem involvement and eye-movement abnormalities had vertical gaze paresis, as in the present case. Other common symptoms reported include short-term memory dysfunction, excessive daytime sleepiness, diplopia, dysarthria, ataxia, parkinsonism or hypokinesia, and narcolepsy, with low CSF hypocretin-1 levels.4,6 Our patient also had a significant unexplained weight gain; hypothalamic obesity has been described in the spectrum of this disorder.4,7
Multifocal involvement observed on MRI, as seen in our patient, likely reflects the widespread distribution of Ma proteins throughout the brain as well as the diverse symptoms seen in anti-Ma encephalitis. In the study of Dalmau et al.,4 almost 75% of patients developed abnormal MRI findings, with more than one area being involved in 62% of these patients. Only 21% had neurological stabilization, with improvement in only one-third of those patients treated with immunotherapy or tumor-directed treatment.4 Our patient had significant improvement of her MRI findings after treatment with corticosteroids, chemotherapy, and radiation, but remained symptomatically stable.
A recent study tested the sensitivity and specificity of Ma2 antibodies sent to three European commercial laboratories.8 Using immunoblotting, one laboratory achieved a sensitivity of 88% and a specificity of 100%. A second laboratory reported a sensitivity of 100% but a specificity of only 89%. In the third laboratory, the sensitivity and specificity were 94% and 100%, respectively. Immunochemistry performed in one laboratory identified neuronal nucleolar staining in 16 of 17 patients, but in 3 the pattern was weak and appeared only in isolated neurons. Thus, although usually highly sensitive and specific, false-negative and occasional false-positive results do occur. In our patient the antibody was not found in a commercial laboratory, but in the academic laboratory of Dr. Josep Dalmau. Curiously, the CSF was negative, an unusual finding in a patient with a PNS of the central nervous system where the titer in the CSF is often substantially higher than that in serum.
Cervical cancer is a common malignancy among women, but it is rarely associated with PNS.9,10,11 The tumors most often associated with anti-Ma2 encephalitis include testicular, lung, breast, gastrointestinal cancer, and non-Hodgkin lymphoma.4 To the best of our knowledge, this is the first reported case of squamous cell carcinoma of the cervix associated with anti-Ma2-associated encephalitis. Interestingly, the syndrome occurred at the time of tumor recurrence. Since there was initial concern regarding a second malignancy, the patient underwent a biopsy which provided pathological confirmation of recurrent cervical cancer. In rare cases PNS can herald the relapse of a known malignancy.12,13 In the present case, the presence of anti-Ma2 antibodies prompted cancer screening, and PET/CT scans revealed active malignancy. This case is otherwise consistent with the clinical features of anti-Ma2 encephalitis, as patients may have a wide range of clinical presentations and tumor types.5
PNS are rare. Neurological symptoms typically precede the diagnosis of the underlying malignancy, and therefore patients often present to physicians other than oncologists. Due to the diffuse nature of the presenting symptoms, anti-Ma2 encephalitis is probably largely underrecognized and physicians should have a high degree of suspicion for the diagnosis. PET and CT scans remain important for the early diagnosis of malignancy in patients with PNS.13 A combination of two independent laboratory assays may be necessary when searching for underlying autoantibodies.8 The presentation of our patient was consistent with symptoms of hypothalamic involvement as well as brainstem encephalitis with prominent vertical gaze paresis, a common presentation for this disorder. Unfortunately, her neurological symptoms did not improve markedly, but did allow for further therapy aimed at palliation of the recurrent cancer.
Figures and Tables
 | Fig. 1Postgadolinium T1 (A) and fluid-attenuated inversion recovery (FLAIR) (B) sequences obtained upon presentation. Postgadolinium T1 (C) and FLAIR (D) sequences after treatment with high-dose steroids, chemotherapy, and directed radiation to the involved pelvic lymph nodes. |
Acknowledgements
The authors are grateful to Jerome Posner, M.D. of Memorial Sloan-Kettering Cancer Center and Rebecca Fisher, M.D. of Beth Israel Medical Center for their critical review of this manuscript. We also wish to thank Josep Dalmau, M.D., Ph.D. of the University of Pennsylvania for testing for antibodies.
References
1. Voltz R, Gultekin SH, Rosenfeld MR, Gerstner E, Eichen J, Posner JB, et al. A serologic marker of paraneoplastic limbic and brain-stem encephalitis in patients with testicular cancer. N Engl J Med. 1999; 340:1788–1795.

2. Graus F, Delattre JY, Antoine JC, Dalmau J, Giometto B, Grisold W, et al. Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry. 2004; 75:1135–1140.

3. Ahern GL, O'Connor M, Dalmau J, Coleman A, Posner JB, Schomer DL, et al. Paraneoplastic temporal lobe epilepsy with testicular neoplasm and atypical amnesia. Neurology. 1994; 44:1270–1274.

4. Dalmau J, Graus F, Villarejo A, Posner JB, Blumenthal D, Thiessen B, et al. Clinical analysis of anti-Ma2-associated encephalitis. Brain. 2004; 127(Pt 8):1831–1844.

5. Hoffmann LA, Jarius S, Pellkofer HL, Schueller M, Krumbholz M, Koenig F, et al. Anti-Ma and anti-Ta associated paraneoplastic neurological syndromes: 22 newly diagnosed patients and review of previous cases. J Neurol Neurosurg Psychiatry. 2008; 79:767–773.

6. Adams C, McKeon A, Silber MH, Kumar R. Narcolepsy, REM sleep behavior disorder, and supranuclear gaze palsy associated with Ma1 and Ma2 antibodies and tonsillar carcinoma. Arch Neurol. 2011; 68:521–524.

7. Darnell RB, Posner JB. Paraneoplastic Syndromes. New York: Oxford University Press;2011.
8. Johannis W, Renno JH, Wielckens K, Voltz R. Ma2 antibodies: an evaluation of commercially available detection methods. Clin Lab. 2011; 57:321–326.
9. Okagbue UE, Wang LY, Cymet T, Rabin B, Erlich RB. A rare case of anti-Hu paraneoplastic neurologic syndrome in association with cervical cancer. Compr Ther. 2008; 34:48–50.
10. Power DG, McVey GP, Delaney DW, Rea D, D'arcy T, Daly PA, et al. Papillary serous carcinomas of the uterine cervix and paraneoplastic cerebellar degeneration: a report of two cases. Acta Oncol. 2008; 47:1590–1593.

11. Sutton GP, Siemers E, Stehman FB, Ehrlich CE. Eaton-Lambert syndrome as a harbinger of recurrent small-cell carcinoma of the cervix with improvement after combination chemotherapy. Obstet Gynecol. 1988; 72(3 Pt 2):516–518.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download