Abstract
Background and Purpose
Aggressive treatment of posterior-circulation occlusions is important due to the high rates of morbidity and mortality associated with these infarctions. A large administrative database was evaluated to determine the outcomes of mechanical thrombectomy and intravenous tissue plasminogen activator (IV-tPA) for the treatment of posterior-circulation (vertebrobasilar) strokes. Outcomes were compared across age groups.
Methods
The United States Nationwide Inpatient Sample was used to evaluate the outcomes of patients treated for posterior-circulation acute ischemic stroke between 2006 and 2010. Patients who underwent endovascular mechanical thrombectomy and IV-tPA were selected. Primary outcomes were discharge status and mortality; secondary outcomes were length of stay, rate of intracranial hemorrhage, tracheostomy, and percutaneous endoscopic gastrostomy/jejunostomy tube placement. Outcomes were grouped according to age (i.e., <50, 50-64, and ≥65 years). Chi-squared test and Student's t-test were used for comparisons of categorical and continuous variables, respectively.
Results
During 2006-2010 there were 36,675 patients who had discharge International Classification of Diseases (9th edition) codes indicating posterior-circulation strokes. Of these, 631 (1.7%) underwent mechanical thrombectomy and 1554 (4.2%) underwent IV-tPA. The in-hospital mortality rate for mechanical thrombectomy patients was significantly lower for those aged <50 years than for those aged 50-64 years (30.4% versus 47.4%, p<0.01) and those aged ≥65 years (30.4% versus 43.0%, p≤0.01). Age had no effect on the in-hospital mortality for IV-tPA patients, with an incidence of 22.7% for patients aged <50 years, compared to 25.4% for patients aged 50-64 years (p=0.46) and 23.0% for patients aged ≥65 years (p=0.92).
Conclusions
Patients requiring IV-tPA and/or mechanical thrombectomy for the treatment of posterior-circulation strokes suffer from high mortality rates. Increased age is associated with significantly higher mortality rates among posterior-circulation stroke patients who require mechanical thrombectomy.
Intravenous tissue plasminogen activator (IV-tPA) and mechanical thrombectomy are known to improve the outcomes of acute ischemic stroke among certain patients.1-5 Patients suffering from posterior-circulation (vertebrobasilar) occlusions suffer high morbidity and mortality rates, and previous studies have demonstrated that those with posterior-circulation occlusions have a poor prognosis regardless of the treatment modality used.6-10 It has also been demonstrated that increasing age is associated with worsening morbidity and mortality for acute ischemic stroke patients treated with either IV-tPA or mechanical thrombectomy.11-13 The present study evaluated Nationwide Inpatient Sample (NIS) data from the period 2006-2010 in order to determine the real-world outcomes in patients with posterior-circulation occlusions treated with endovascular clot retrieval (i.e., mechanical thrombectomy) or IV-tPA in the general population. Data were compared across age groups.
The NIS hospital discharge database for the period 2006-2010 were purchased from the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality (Rockville, MD, USA). The NIS is a hospital discharge database that represents 20% of all inpatient admissions to nonfederal hospitals in the USA.
Patients who had an ischemic stroke were identified using International Classification of Diseases (9th edition, ICD-9) codes 433, 434, 436, 437.0, and 437.1. Patients with posterior-circulation occlusions were identified using ICD-9 modifier codes 433.00, 433.01, 433.20, and 433.21 (occlusion of the basilar and vertebral arteries). Separate analyses were performed for patients receiving IV-tPA (ICD-9 procedure code 99.10) and those undergoing endovascular mechanical thrombectomy (ICD-9 procedure code 39.74). Patients who received both IV-tPA and endovascular mechanical thrombectomy were analyzed with the endovascular mechanical thrombectomy group. The patients were stratified into three age groups: <50, 50-64, and ≥65 years. The age of 65 years is commonly used as the cutoff between middle-aged and older patients, and 50 years is the age below which strokes are considered to occur in the young. These cutoffs were defined a priori in order to facilitate age comparisons. Other demographic variables studied included patient gender and race. The Charlson Comorbidity Index (CCI) was calculated for each patient. Other comorbidities studied include diabetes mellitus, hypertension, and cardiac dysrhythmia.
The primary outcomes for this study were in-hospital mortality, discharge to home/short-term facility, and discharge to a long-term facility. Length of stay, intracranial hemorrhage (ICH; ICD-9 diagnosis code 430-432.9), tracheostomy (Clinical Classifications Software procedure code 34), and percutaneous endoscopic gastrostomy/jejunostomy (PEG/PEJ) tube placement (ICD-9 procedure codes 4311 and 4632) were secondary endpoints. Length of stay was reported only for patients who did not suffer in-hospital mortality. A subgroup analysis of mortality and ICH rates was performed for patients receiving mechanical thrombectomy and concomitant IV-tPA versus patients receiving mechanical thrombectomy only and IV-tPA only. A subgroup analysis of mortality rates relating to cardiac dysrhythmia, diabetes mellitus, and hypertension was performed for mechanical thrombectomy and IV-tPA patients.
For the purposes of statistical analysis, the data from 2006-2010 were summed. Chi-square testing was used to compare categorical variables and Student's t-test was used to compare continuous variables. No adjustments were made for multiple comparisons. National estimates were obtained by applying discharge weights. All statistical analyses were performed using the SAS-based statistical package JMP (www.jmp.com). Multivariate logistic regression analysis was performed to determine the variables associated with in-hospital mortality. Separate models were constructed for patients treated with IV-tPA and those treated with mechanical thrombectomy. Independent variables studied included the CCI,14 age group, gender, and race. For patients treated with mechanical thrombectomy, IV-tPA utilization was included in addition to the previously mentioned variables. Diabetes, hypertension, and cardiac dysrhythmia were not included as independent variables in the multivariate analysis, as they are already a component of the CCI.
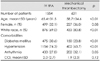
Acute ischemic stroke caused by posterior-circulation occlusion was diagnosed in 36,675 patients between 2006 and 2010, of which 631 (1.7%) were treated with mechanical thrombectomy and 1554 (4.2%) were treated with IV-tPA. 340 (53.9%) of mechanical thrombectomy patients also received IV-tPA. The patients undergoing mechanical thrombectomy were 58.7±34.6 years old (mean±SD) and had a CCI of 1.9±2.3, 227 (36.0%) were female, and 433 (80.8%) were white. The patients receiving IV-tPA were 65.4±31.5 years old and had a CCI of 2.0±2.7; 499 (32.1%) of them were female, and 876 (69.0%) were white. These data are summarized in Table 1.
The in-hospital mortality rate for mechanical thrombectomy patients aged <50 years was 30.4% (55/180). The in-hospital mortality rate was significantly higher for patients aged 50-64 years than for their younger (47.4%, 101/218; p<0.01) and older (43.0%, 98/233; p<0.01) counterparts. Patients aged <50 years were discharged to home/short-term facilities in 44.1% of cases (79/180), while those aged 50-64 years (18.9%, 41/218) and ≥65 years (18.3%, 42/233) had significantly lower rates of discharge to home/short-term facilities (p<0.01 for both). The tracheostomy rate was 14.9% (26/180) for patients aged <50 years, 13.8% (30/218) for patients aged 50-64 years (p=0.77), and 13.8% (31/233) for patients aged ≥65 years (p=0.77); the corresponding PEG/PEJ tube placement rates were 17.0% (31/180), 18.4% (40/218, p=0.73) and 9.4% (22/233, p=0.02). The length of stay and ICH rate did not differ significantly between those aged <50 years and the other two age groups. These data are summarized in Table 2.
A total of 340 patients treated with mechanical thrombectomy (53.9%) received concomitant IV-tPA. IV-tPA administration did not significantly alter the mortality rate: this was 38.7% (132/340) and 43.4% (122/280) among mechanical thrombectomy patients receiving and not receiving IV-tPA, respectively (p=0.24); the corresponding ICH rates were 11.1% (38/345) and 21.3% (61/286, p<0.01).
The mortality rate was significantly higher among mechanical thrombectomy patients receiving IV-tPA (38.7%, 132/340) than among those receiving IV-tPA alone (23.8%, 370/1554; p<0.01). The ICH rate among patients receiving IV-tPA alone was 7.4% (115/1554, p=0.02).
In-hospital mortality did not differ between IV-tPA patients aged <50 years (22.7%, 41/179), 50-64 years (25.4%, 134/529; p=0.46), and ≥65 years (23.0%, 195/846; p=0.92). Patients aged <50 were discharged to home/short-term facilities in 52.1% of cases (93/179), compared to 38.7% (205/529) for patients aged 50-64 years (p=0.01) and 26.9% (227/846) for those aged ≥65 years (p<0.01). Tracheostomy rates were 11.4% (20/179) for patients aged <50 years, compared to 8.4% (44/529) for those aged 50-64 years (p=0.23) and 8.3% (70/846) for those aged ≥65 years (p=0.18); the corresponding PEG/PEJ tube placement rates were 7.7% (14/179), 10.5% (56/529, p<0.28), and 13.6% (115/846, p=0.03). The length of stay did not differ significantly between patients aged <50 years and the other two age groups. These data are summarized in Table 3.
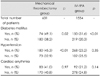
The mortality rates was higher among mechanical thrombectomy patients with a diagnosis of diabetes mellitus than among those without such a diagnosis (49.1% versus 38.2%, p=0.02). Similar findings were seen in the IV-tPA group (31.6% versus 20.3%, p<0.01). Hypertension was a significant predictor of mortality in the mechanical thrombectomy group (45.3% versus 32.9%, p<0.01) but not in the IV-tPA group (23.2% versus 25.5%, p=0.35). Cardiac dysrhythmia was not associated with mortality in either the mechanical thrombectomy group (41.0% versus 40.8%, p=0.97) or the IV-tPA group (21.2% versus 24.8%, p=0.14). These data are summarized in Table 4.
For patients receiving mechanical thrombectomy, multivariate analysis demonstrated that compared to patients aged <50 years, those aged 50-64 years had a higher odds ratio (OR) for in-patient mortality [OR=1.79, 95% confidence interval (CI)=1.14-2.83; p=0.01], as did patients aged ≥65 years (OR=1.62, 95%CI=1.02-2.58; p=0.04). IV-tPA administration was not associated with any difference in in-hospital mortality (OR=0.86, 95%CI=0.59-1.24; p=0.42). Multivariate logistic regression analysis for patients receiving IV-tPA demonstrated no significant difference in mortality for age. These data are summarized in Table 5.
The NIS provides data on real-world outcomes and practice data for patients treated with IV-tPA and endovascular mechanical thrombectomy across the USA. The findings of the present study demonstrate a relatively high rate of poor outcomes among patients requiring IV-tPA and/or mechanical thrombectomy for the treatment of acute posterior-circulation stroke. Overall, almost 75% of patients receiving mechanical thrombectomy and 66% of those receiving IV-tPA either died or were discharged to long-term care facilities. Both mechanical thrombectomy and IV-tPA were associated with increasingly worse outcomes with advancing age, although the relationship between age and mortality was stronger among patients treated with endovascular therapy.
Several studies have examined the outcomes of mechanical thrombectomy for the treatment of posterior-circulation stroke. Reported mortality rates for mechanical endovascular recanalization for the treatment of vertebrobasilar stroke range from 20% to 45%, with a good clinical outcome seen in 20-50% of patients.15-21 Recanalization rates are generally high, ranging from 80% to 100%.15-21 In a pooled analysis of patients with vertebrobasilar stroke in the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and multi-MERCI trials, Lutsep et al.18 found that clot retrieval resulted in recanalization rates of nearly 80%. However, the mortality rate in their analysis was 44%, and good outcomes were only seen in 41% of patients.18 In a study of a "drip, ship, and retrieve" protocol in which patients treated in a community setting were given IV-tPA and sent to stroke centers that provided endovascular mechanical recanalization, Pfefferkorn et al. found a recanalization rate of 85%, a mortality rate of 31%, and good clinical outcomes in 20% of patients.21 Mordasini et al. found that stent retrieval for the treatment of acute basilar artery occlusion resulted in a 100% recanalization rate, with a mortality rate of 36% and good clinical outcomes in approximately 30% of patients.20 These results are similar to those of the present study, which included a much larger population; nearly 40% of the mechanical thrombectomy patients suffered in-hospital mortality and only 25% of patients were discharged to home. The ICH rate in the present study was approximately 16%; those reported elsewhere for mechanical clot retrieval for vertebrobasilar stroke have ranged from 6% to 21%.15-21
Several studies have examined the outcomes of IV-tPA for the treatment of vertebrobasilar stroke.7,9,13 In a systematic meta-analysis comparing intravenous thrombolysis (IVT) to intra-arterial thrombolysis, Lindsberg et al. found a recanalization rate with IVT of 53%, a mortality rate of 50%, and good clinical outcomes in approximately 25% of patients.7 The Basilar Artery International Cooperation Study (BASICS) found that 16% and 30.6% of IV-tPA patients presenting with a mild-to-moderate deficit died and had significant morbidity, respectively; the corresponding rates for patients with a severe deficit were 46% and 28%.9 Sairanen et al.13 reported a recanalization rate of 65%, a mortality rate of 41%, and a good clinical outcome in 26% of patients receiving IV-tPA; they also found that increasing age was associated with increased morbidity and mortality. ICH rates with IV-tPA in these large studies have ranged between 10% and 15%.7,13 Similar to these studies, IV-tPA in the present study was associated with an in-hospital mortality rate of approximately 25%, a discharge to home rate of 33%, and an ICH rate of approximately 7%. Similar to the BASICS, we found that gender was not associated with an increased rate of poor outcomes with IV-tPA22; the present findings demonstrate that increasing age is associated with worsening outcomes for both mechanical thrombectomy and IVT in patients treated for vertebrobasilar stroke. In the mechanical thrombectomy group, approximately 44% of patients under the age of 50 years were discharged to home/short-term care facilities, while less than 20% of patients over the age of 50 years were discharged to home/short-term care facilities. Similarly, in the IV-tPA group, more than 50% of patients under the age of 50 years were discharged to home/short-term care facilities, while the rates for patients aged 50-64 and ≥65 years were approximately 40% and 25%, respectively. These findings are consistent with those of previous studies demonstrating that increasing age is associated with significantly worsening outcomes for mechanical thrombectomy and IV-tPA patients.11-13
In the current context of recently published studies that have demonstrated no significant difference in outcomes between IV-tPA and mechanical thrombectomy for the treatment of acute ischemic stroke,23 the role of mechanical thrombectomy needs to be examined further, especially in younger patients. Approximately 40% of the patients included in the recent study of Ciccone et al. were ≤67 years old, among which a good functional outcome occurred in 42% of the endovascular treatment patients versus 38% of the IV-tPA patients (p=0.75).23 Future randomized controlled studies of the benefit of endovascular versus intravenous treatment could focus on this younger cohort of patients in order to demonstrate improved endovascular outcomes.
The NIS does not provide data on stroke severity (e.g., National Institutes of Health Stroke Scale), functional outcome (e.g., modified Rankin Scale score), or 90-day mortality, and hence it is not possible to compare the present results with the outcomes reported for prospective registries and clinical trials. Instead, discharge status was used as a measure of morbidity in the present study, as in previous studies that also used this administrative database.11,24 Thus, when assessing mortality, it is not possible to account for patients who received palliative care and may have died shortly after their hospitalization. The severity of clinical presentation is one of the most important determinants of clinical outcome, as demonstrated by the BASICS.9,25 It is likely that patients with a higher stroke severity were directed toward endovascular therapy rather than IV-tPA, but because information on stroke severity at presentation was not available, the effect of such a bias on morbidity and mortality within the endovascular and IV-tPA subgroups could not be assessed in the present study. Therefore, the outcomes were not compared between IV-tPA and mechanical thrombectomy patients.
The NIS database does not contain information regarding the time-to-treatment and degree of recanalization, both of which are significant predictors of clinical outcome. In a BASICS subgroup analysis, time to recanalization was found to be a significant predictor of clinical outcome.25 Previous studies have demonstrated that recanalization is associated with improved outcomes with both IV-tPA and endovascular recanalization.6,7,9,10,13,16,18-20 Coding errors are also a potential limitation of the present study, as with any study utilizing a large administrative database.
In conclusion, patients requiring recanalization for acute posterior-circulation strokes have high morbidity and mortality rates. Regardless of the treatment modality, outcomes for posterior-circulation infarctions receiving recanalization worsen with increasing age. Further studies are needed to optimize the outcome in patients with posterior-circulation occlusions who undergo IV-tPA and mechanical thrombectomy.
Figures and Tables
Table 1
Demographics of patients in the intravenous tissue plasminogen activator (IV-tPA) and mechanical thrombectomy groups
References
1. Bose A, Henkes H, Alfke K, Reith W, Mayer TE, Berlis A, et al. The Penumbra System: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am J Neuroradiol. 2008; 29:1409–1413.

2. Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004; 363:768–774.

3. Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, et al. The European Cooperative Acute Stroke Study (ECASS). Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. JAMA. 1995; 274:1017–1025.

4. Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008; 39:1205–1212.
5. Smith WS, Sung G, Starkman S, Saver JL, Kidwell CS, Gobin YP, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. 2005; 36:1432–1438.

6. Davis SM, Donnan GA. Basilar artery thrombosis: recanalization is the key. Stroke. 2006; 37:2440.
7. Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke. 2006; 37:922–928.
8. Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. 2011; 10:1002–1014.

9. Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. 2009; 8:724–730.

10. Schulte-Altedorneburg G, Hamann GF, Mull M, Kühne D, Liebetrau M, Weber W, et al. Outcome of acute vertebrobasilar occlusions treated with intra-arterial fibrinolysis in 180 patients. AJNR Am J Neuroradiol. 2006; 27:2042–2047.
11. Brinjikji W, Rabinstein AA, Kallmes DF, Cloft HJ. Patient outcomes with endovascular embolectomy therapy for acute ischemic stroke: a study of the national inpatient sample: 2006 to 2008. Stroke. 2011; 42:1648–1652.

12. Nasr DM, Brinjikji W, Cloft HJ, Rabinstein AA. Utilization of intravenous thrombolysis is increasing in the United States. Int J Stroke. 2013; 8:681–688.

13. Sairanen T, Strbian D, Soinne L, Silvennoinen H, Salonen O, Artto V, et al. Intravenous thrombolysis of basilar artery occlusion: predictors of recanalization and outcome. Stroke. 2011; 42:2175–2179.

14. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.

15. Andersson T, Kuntze Söderqvist Å, Söderman M, Holmin S, Wahlgren N, Kaijser M. Mechanical thrombectomy as the primary treatment for acute basilar artery occlusion: experience from 5 years of practice. J Neurointerv Surg. 2013; 5:221–225.

16. Costalat V, Machi P, Lobotesis K, Maldonado I, Vendrell JF, Riquelme C, et al. Rescue, combined, and stand-alone thrombectomy in the management of large vessel occlusion stroke using the solitaire device: a prospective 50-patient single-center study: timing, safety, and efficacy. Stroke. 2011; 42:1929–1935.

17. Espinosa de Rueda M, Parrilla G, Zamarro J, García-Villalba B, Hernández F, Moreno A. Treatment of acute vertebrobasilar occlusion using thrombectomy with stent retrievers: initial experience with 18 patients. AJNR Am J Neuroradiol. 2013; 34:1044–1048.

18. Lutsep HL, Rymer MM, Nesbit GM. Vertebrobasilar revascularization rates and outcomes in the MERCI and multi-MERCI trials. J Stroke Cerebrovasc Dis. 2008; 17:55–57.

19. Miteff F, Faulder KC, Goh AC, Steinfort BS, Sue C, Harrington TJ. Mechanical thrombectomy with a self-expanding retrievable intracranial stent (Solitaire AB): experience in 26 patients with acute cerebral artery occlusion. AJNR Am J Neuroradiol. 2011; 32:1078–1081.

20. Mordasini P, Brekenfeld C, Byrne JV, Fischer U, Arnold M, Heldner MR, et al. Technical feasibility and application of mechanical thrombectomy with the Solitaire FR Revascularization Device in acute basilar artery occlusion. AJNR Am J Neuroradiol. 2013; 34:159–163.

21. Pfefferkorn T, Holtmannspötter M, Schmidt C, Bender A, Pfister HW, Straube A, et al. Drip, ship, and retrieve: cooperative recanalization therapy in acute basilar artery occlusion. Stroke. 2010; 41:722–726.
22. Arnold M, Fischer U, Compter A, Gralla J, Findling O, Mattle HP, et al. Acute basilar artery occlusion in the Basilar Artery International Cooperation Study: does gender matter? Stroke. 2010; 41:2693–2696.

23. Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013; 368:904–913.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download