Abstract
Background
The risk factors for intracranial atherosclerosis are unclear but may differ from those for other stroke subtypes. Here, we investigated whether metabolic syndrome, an emerging risk factor for cardiovascular disease, is associated with intracranial atherosclerotic stroke.
Methods
Using the Adults Treatment Panel III criteria, we evaluated the components of metabolic syndrome in 439 patients with ischemic stroke or transient ischemic attacks. The prevalence of metabolic syndrome within each stroke subtype was determined, and the association between intracranial atherosclerosis and metabolic syndrome was evaluated.
Results
Metabolic syndrome was observed more frequently in patients with intracranial atherosclerosis than in those with other types of stroke (P=0.003). In a multiple regression analysis, metabolic syndrome, but not conventional risk factors, was independently associated with intracranial atherosclerosis (P=0.016). By contrast, the serum level of C-reactive protein was correlated negatively with the presence of intracranial atherosclerosis. Intracranial atherosclerosis was most prevalent in patients with metabolic syndrome and low levels of C-reactive protein (P=0.024).
Intracranial atherosclerosis causes 8~10% of all acute strokes in the United States. In one Chinese study, more than half of patients with acute ischemic stroke had intracranial stenosis.1 The risk factors for intracranial atherosclerosis are unclear and may differ from those for other stroke subtypes; they may even differ from risk factors for extracranial atherosclerosis.
It has been suggested that metabolic syndrome, which refers to a constellation of metabolic risk factors that are linked to insulin resistance, is associated with increased risk for cardiovascular disease. The guidelines in the Third Report of the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP-III) recognized metabolic syndrome as a secondary target for risk-reduction therapy and defined metabolic syndrome as the presence of three or more of five risk determinants.2 Recently, it was reported that metabolic syndrome was associated with risk that was not accounted for entirely by traditional risk scoring paradigms.3 As ischemic stroke is a heterogeneous condition, the impact of metabolic syndrome on ischemic syndrome may depend on the stroke subtype.
In the mid 1990s, immunoassays for C-reactive protein (CRP), with greater sensitivity than those previously in routine use, revealed that increased CRP values, even within the range previously considered normal, strongly predict future coronary events. Recently, it is generally accepted that inflammation is important in plaque rupture, including an association between elevated CRP levels and an increased risk of ischemic events or high-risk unstable plaque morphology.
Our hypothesis was that metabolic syndrome is associated with intracranial large atherosclerotic stroke, as inflammation in carotid and coronary atherosclerosis. Therefore, we investigated the impact of metabolic syndrome on the development of intracranial atherosclerotic stroke. We also evaluated the possible interrelationships among metabolic syndrome, CRP level, and atherosclerotic stroke.
From September 2002 to August 2004, we prospectively studied consecutive patients admitted to the Department of Neurology at Ajou University Hospital with ischemic stroke or transient ischemic attacks. Patients were evaluated according to a protocol that included demographic data, medical history, vascular risk factors, clinical stroke syndrome, and the National Institutes of Health Stroke Scale (NIHSS) score, as in our previous studies.4-5 All patients underwent diagnostic testing that included a vascular study (digital subtraction or magnetic resonance angiography), echocardiogram, electrocardiogram, and routine blood tests. Digital subtraction angiography was performed in 77 patients and magnetic resonance angiography in the remaining patients, at 1.8±2.3 days after the onset of symptoms. We additionally performed transesophageal echocardiogram and/or Holter monitoring, if the patient had one of the following characteristics: past vascular events, such as deep venous thrombosis, or pulmonary embolism; palpitations preceding or accompanying stroke onset; or peripheral vascular insufficiency, deep vein thrombosis, or pulmonary embolism (38 patients). Hemostatic markers of prothrombotic tendency, including protein C, protein S, antithrombin III, and antiphospholipid antibodies were measured in all patients younger than 50 years.
Based on clinical syndrome, infarct size on a diffusion-weighted image, the results of vascular and cardiological studies, and laboratory data, we divided the patients into five groups, as reported previously6: (1) large artery atherosclerosis (LAA); (2) cardioembolism; (3) small arterial disease (SAD); (4) other determined causes, such as carotid or vertebral dissection, hypercoagulable state, vasculitis, and complicated migraine; and (5) cryptogenic stroke. Patients in the LAA group were divided further into two groups: (1) those with occlusive lesions on the extracranial arterial system (EC-LAA group) and (2) those with occlusive lesions on the proximal portion of the middle cerebral artery, intracranial portion of the vertebral artery, or basilar artery, but with no significant stenosis on the relevant extracranial arterial system (IC-LAA group). An occlusive lesion was defined according to previously published criteria as >50% stenosis or occlusion of the large intracranial and extracranial vessels.7-8 An acceptable level of agreement for the presence of an occlusive lesion on angiography was found between the raters who interpreted the angiograms (kappa=0.91, P<0.05). The exclusion criteria included patients who underwent an incomplete workup (29 patients), who had had two or more causes of stroke (nine patients), or who had isolated lesions on the intracranial portion of the internal carotid artery (20 patients).
The NCEP ATP-III guidelines define metabolic syndrome as the presence of three or more of the following risk factors2: (1) abdominal obesity; (2) elevated triglyceride levels (≥150 mg/dl); (3) low high-density lipoprotein (HDL) cholesterol levels (<40 mg/dl for men, <50 mg/dl for women); (4) hypertension (systolic blood pressure ≥130 mmHg or diastolic pressure ≥85 mmHg) or antihypertensive medication use; and (5) impaired fasting glucose levels (≥110 mg/dl). Using the revised Asia-Pacific criteria suggested aracteristics of the study population by the World Health Organization Western Pacific Region (2000), abdominal obesity was defined as a waist circumference of ≥90 cm for men and ≥80 cm for women.9
Samples of peripheral blood were withdrawn from each patient at the time of admission (mean±SD=1.8±2.2 days after symptom onset). As a novel risk factor for atherosclerosis, the serum levels of CRP of all except eight patients were evaluated using a highly sensitive assay. Three patients with CRP levels >100 mg/L were also excluded from this assay because of the possible coexistence of an infectious condition. Consistent with recent recommendations from the Centers for Disease Control and Prevention, a CRP cutoff value of 3 mg/L was used to differentiate high and low levels.10
Differences between groups were examined using a Chi-squared test, Student's t-test, or a one-way analysis of variance (ANOVA) with appropriate post hoc tests for significance. We performed a multi-variant logistic regression analysis to determine whether metabolic syndrome and CRP levels were independent predictors for intracranial atherosclerosis in addition to the risk factors for stroke. Those factors that were significant at the 0.2 level were entered into the initial multivariate model. When the most parsimonious model was obtained by backward stepwise elimination of nonsignificant factors, each of the excluded variables was again entered separately into the model to test its contribution to the final model. The results are presented as odds ratio (OR) estimates of relative risk with a 95% confidence interval (CI). Statistical significance was established at P<0.05.
Among 497 patients who were admitted during the study period, 439 were included in the study (254 men and 185 women, mean age=62.3±12.3 years). According to clinical, diffusion-weighted imaging, angiography, and cardiological findings, 121 patients were classified in the IC-LAA group, 67 in the EC-LAA group, 104 in the SAD group, 56 in the cryptogenic group, 60 in the cardioembolic group, and 31 in the other cause group.
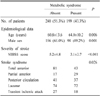
The clinical characteristics are presented in Table 1. Metabolic syndrome was observed in 199 of 439 patients (43.3%). Patients with metabolic syndrome were significantly older and were more likely to be female (P=0.05 for both variables). The severity of stroke and stroke syndrome differed according to the presence of metabolic syndrome: the NIHSS score at admission was significantly lower in patients with metabolic syndrome than in those without metabolic syndrome (P<0.001), and, while total anterior circulation infarcts were more common in the latter group, lacunar and partial anterior circulation infarcts were observed more often in the former group (P=0.026).
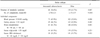
The frequency of metabolic syndrome was variable and depended on the stroke subtype (P=0.003). Patients in the IC-LAA group had the highest frequency of metabolic syndrome (58.7%), whereas lower frequencies of metabolic syndrome were associated with patients with cardioembolic (30.0%), cryptogenic (35.7%), and other types of stroke (35.5%). The prevalence of metabolic syndrome in patients in the SAD and EC-LAA groups was similar and intermediate (48.1 and 43.3%, respectively). The same was true for the number of components of metabolic syndrome exhibited by patients (P<0.001; Fig. 1): patients in the IC-LAA group had a higher level of metabolic abnormality compared with those of the other groups, particularly with regard to blood pressure, abdominal obesity, and HDL cholesterol levels (Table 2).
Table 3 shows the results of the multiple logistic regression model and the OR for each factor. Metabolic syndrome, but not conventional risk factors, was independently associated with intracranial athero sclerosis. Patients with more severe metabolic abnormalities were more likely to have intracranial atherosclerosis (P=0.016). Patients with 1, 2, 3, 4, and 5 components of metabolic syndrome were about 3, 4, 5, 8, and 5 times more likely to have intracranial atherosclerosis, respectively, compared with patients who had no abnormalities, after adjustment for other risk factors. By contrast, CRP levels were correlated negatively with intracranial atherosclerosis, although this correlation was not statistically significant (P=0.084).
To explore the relationships among metabolic syndrome, CRP level, and intra- and extracranial atherosclerosis, we divided the study cohort into four groups on the basis of the presence or absence of metabolic syndrome and on the basis of CRP levels less than or greater than 3.0 mg/L. As shown in Fig. 2, the frequency and type of atherosclerotic stroke were associated with the serum level of CRP as well as with the presence or absence of metabolic syndrome. When the patients were categorized into four risk groups, strokes in patients in the IC-LAA group were less prevalent in patients who had a high level of serum CRP than in patients with a low CRP level, regardless of the presence or absence of metabolic syndrome. The frequency of intracranial atherosclerosis was highest in patients who had metabolic syndrome and low CRP levels and was lowest in patients who had metabolic syndrome and high CRP levels (P=0.024). The latter group had the highest frequency of extracranial atherosclerosis, although this was not statistically significant (P=0.262). Beside the site of atherosclerosis, the level of CRP was not related to the presence or absence of metabolic syndrome (4.60±9.25 mg/L and 4.42±9.54 mg/L, respectively; P=0.845). In addition, for all subjects, correlation analysis showed that CRP was not significantly associated with blood pressure, serum glucose, triglyceride, HDL-cholesterol, and waist circumference (r<0.05, P>0.05 in all the cases).
Metabolic syndrome is associated with an increased risk of cardiovascular disease and mortality in patients without a history of cardiovascular disease. Metabolic syndrome is also associated with subclinical ultrasound-associated atherosclerosis.11 In the present study, the proportion of individuals with metabolic syndrome was almost identical to those evaluated in other studies of stroke patients; specifically, the proportion of patients in the present study with three or more components of the metabolic syndrome was 43.3% compared with 42.8% in the Second Manifestations of Arterial Disease (SMART) Study.12
The apparent differences in risk factors for intra- and extracranial atherosclerosis are unclear. In the present study, we investigated several novel factors that emerged recently as risk factors for atherosclerosis. Our study revealed diversity in the frequency of metabolic syndrome that depended on the stroke subtype; this may be due to the fact that ischemic stroke is a heterogeneous condition. Our study revealed that metabolic syndrome (rather than conventional risk factors) is a strong independent risk factor for intracranial atherosclerotic stroke. To our knowledge, the frequency and implications of metabolic syndrome in patients with intracranial atherosclerosis have not been reported to date. The association between intracranial atherosclerosis and metabolic syndrome may be derived from the individual components of the syndrome, such as abdominal obesity, hypertension, and HDL cholesterol levels. However, our multivariate analysis demonstrated that modeling the severity of metabolic abnormalities as a risk factor for intracranial atherosclerosis was a powerful yet convenient method to incorporate several proven risk factors.
Why did patients with intracranial atherosclerosis in the present study exhibit a high frequency of metabolic syndrome? Possible explanations for this include the followings. First, oxidative stress is associated with metabolic syndrome and has been suggested to play a role in endothelial dysfunction and subsequent atherosclerosis.13 Increased vascular risk may be explained by the individual risk factors of metabolic syndrome in association with other aspects of the syndrome that are not measured routinely, such as oxidative stress, impaired fibrinolysis, increased small dense low-density lipoprotein (LDL) cholesterol levels, hypercoagulability, inflammation, and hyperinsulinemia.14 The Third National Health and Nutrition Examination Survey reported that adults with metabolic syndrome have suboptimal concentrations of several antioxidants, which may explain in part why such individuals are at greater risk for the development of cardiovascular disease.15 An autopsy study revealed that intracranial arteries responded with accelerated atherogenesis when antioxidant protection of these arteries was decreased to a relatively greater extent than was the case for extracranial arteries.16 The authors suggested that the progression of atherosclerosis within intracranial arteries might be due partly to reduced intracellular defenses against oxygen radical-mediated processes. Therefore, it is conceivable that intracranial arteries become susceptible to oxidative stress resulting in atherosclerotic stroke, particularly under conditions of increased oxidative stress such as those that exist in patients with metabolic syndrome. Further studies of markers of oxidative stress in patients with intracranial atherosclerosis are needed. The second explanation of why patients with intracranial atherosclerosis exhibited a high frequency of metabolic syndrome is that atherogenesis (including the effect of plasma lipids17) within the intracranial vascular bed might be different from atherogenesis that occurs in coronary or extracranial carotid arteries. Hemodynamic conditions affect atherogenesis and might modify the effects of circulating agents in different vascular beds.
Recently, it was reported that CRP levels were greater in patients with metabolic syndrome and that CRP provided important and independent prognostic information about further cardiovascular risk.18-19 It is well known that CRP directly affects vessel walls and that inflammation is important in plaque rupture. In the present study, however, the level of CRP was negatively correlated with the presence of intracranial atherosclerosis, regardless of the presence or absence of metabolic syndrome. In the same manner, extracranial atherosclerosis was observed most frequently in patients that did not have metabolic syndrome and also had increased CRP levels. These findings suggest that the mechanisms that underlie the development of atherosclerosis within intracranial arteries may differ from those that occur within extracranial arteries and that pathophysiological mechanisms other than inflammation may play an important role in the development of intracranial atherosclerosis.
A limitation of the present study is that our results may represent stroke patients with a high prevalence for intracranial atherosclerosis. However, confounding factors such as differences in the prevalence of risk factors and genetic background were precluded. The strengths of our study include the prospective study design and the availability of well-characterized stroke events for analysis (stroke subtypes, and conventional and novel risk factors). We believe that further studies of different populations (e.g., Caucasians) and larger cohorts are warranted.
The results of the present study suggest that a different therapeutic approach may be needed for atherosclerotic stroke and that the diagnosis of metabolic syndrome (and possibly measurements of CRP levels) will be useful in targeting therapies for the primary prevention of atherosclerotic stroke. If the results of the present study are replicated in subsequent studies, we propose that pharmacological or nonpharmacological treatment of the metabolic abnormalities that characterize the metabolic syndrome may be a major new strategy for preventing intracranial atherosclerotic stroke.
Figures and Tables
Fig. 1
The number of components of metabolic syndrome within each stroke subtype. Asterisk indicates a significantly higher value compared with other stroke subtypes (P<0.001).
SAD; small arterial disease, EC-LAA; extracranial large arterial atherosclerosis, IC-LAA; intracranial large arterial atherosclerosis

Figure 2
The impact of metabolic syndrome and C-reactive protein levels on atherosclerotic stroke. Filled bars (▪), intracranial atherosclerosis; Open bars (□), extracranial atherosclerosis. Met SD indicates metabolic syndrome. CRP, C-reactive protein. Low and high refers to CRP levels of ≤3 and >3 mg/L, respectively.

References
1. Wong KS, Huang YN, Gao S, Lam WW, Chan YL, Kay R. Intracranial stenosis in Chinese patients with acute stroke. Neurology. 1998. 50:812–813.

2. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.
3. Girman CJ, Rhodes T, Mercuri M, Pyorala K, Kjekshus J, Pedersen TR, et al. The metabolic syndrome and risk of major coronary events in the Scandinavian Simvastatin Survival Study (4S) and the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS). Am J Cardiol. 2004. 93:136–141.

4. Bang OY, Lee PH, Joo SY, Lee JS, Joo IS, Huh K. Frequency and mechanisms of stroke recurrence after cryptogenic stroke. Ann Neurol. 2003. 54:227–234.

5. Lee PH, Bang OY, Oh SH, Joo IS, Huh K. Subcortical white matter infarcts: comparison of superficial perforating artery and internal border-zone infarcts using diffusion-weighted magnetic resonance imaging. Stroke. 2003. 34:2630–2635.
6. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993. 24:35–41.

7. Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. Am J Neuroradiol. 2000. 21:643–646.
8. North American Symptomatic Carotid Endarterectomy Trial Collaborator. Beneficial effect of carotid endarterectomy in symptomatic patients with high degree stenosis. N Engl J Med. 1991. 325:445–453.
9. Inoue S, Zimmet P, Catersen I, Chunming C, Ikeda Y, Khalid AK, et al. The Asia-Pacific perspective: redefining obesity and its treatment. 2000. Health Communication Australia Pty.
10. 2002. In : Centers for Disease Control/American Heart Association Workshop on Inflammatory Markers, and Cardiovascular Disease: application to clinical and public health practice; March 14-15, 2002; Atlanta. Atlanta, Ga: Centers for Disease Control and Prevention.
11. Hulthe J, Bokemark L, Wikstrand J, Fagerberg B. The metabolic syndrome, LDL particle size, and atherosclerosis: the atherosclerosis and insulin resistance (AIR) study. Arterioscler Thromb Vasc Biol. 2000. 20:2014–2017.
12. Olijhoek JK, van der Graaf Y, Banga JD, Algra A, Rabelink TJ, Visseren FL, et al. The metabolic syndrome is associated with advanced vascular damage in patients with coronary heart disease, stroke, peripheral arterial disease or abdominal aortic aneurysm. Eur Heart J. 2004. 25:342–348.

13. Cai H, Harrison DG. Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res. 2000. 87:840–844.

14. Sakkinen PA, Wahl P, Cushman M, Lewis MR, Tracy RP. Clustering of procoagulation, inflammation, and fibrinolysis variables with metabolic factors in insulin resistance syndrome. Am J Epidemiol. 2000. 152:897–907.

15. Ford ES, Mokdad AH, Giles WH, Brown DW. The metabolic syndrome and antioxidant concentrations: findings from the Third National Health and Nutrition Examination Survey. Diabetes. 2003. 52:2346–2352.
16. D'Armiento FP, Bianchi A, de Nigris F, Capuzzi DM, D'Armiento MR, Crimi G, et al. Age-related effects on atherogenesis and scavenger enzymes of intracranial and extracranial arteries in men without classic risk factors for atherosclerosis. Stroke. 2001. 32:2472–2479.
17. Shahar E, Chambless LE, Rosamond WD, Boland LL, Ballantyne CM, McGovern PG, et al. Plasma lipid profile and incident ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2003. 34:623–631.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download