Kikuchi's disease (KD) or subacute histiocytic necrotizing lymphadenitis is a benign disorder distinguishable from other types of lymphadenitis and malignancies. It affects mainly young women and presents with cervical lymphadenopathy and fever.1,2 Coexistent findings such as sore throat, headache, elevated serum transaminase levels, and skin rash occur in some patients, especially in those with fever.3 Leukopenia and elevated erythrocyte sedimentation rate (ESR) are usually observed.4 Characteristic histologic findings consist of proliferation of lymphoreticular cells, karyorrhexis, and a variable degree of necrosis. This self-limited reactive process should be differentiated from malignant lymphoma or systemic erythematosus. The course is usually benign; spontaneous resolution usually occurs within 2~3 weeks.5 However, a fatal case involving the myocardium during the active phase of the disease has been reported.6 The involvement of the nervous system is rare. A few patients with meningeal involvement were described in the literature from Japan. However, only few cases of aseptic meningitis in KD have been reported in Korea.7 We report such a patient.
CASE REPORT
A 23-year-old, previously healthy man presented with a 4-day history of severe headache, fever and vomiting. On admission, the temperature was 38.1℃. Signs of meningeal irritation were absent. The results of the neurologic examination were normal. Laboratory data showed a white blood cell count of 4,580/mm3 and an ESR of 37 mm/hr. Anti-nuclear antibody, heterophil antibody, and ASO tests were all negative. Serum and CSF antibody tests for cytomegalovirus, herpes simplex virus, varicella zoster virus, rubella virus, and Ebstein-Barr virus were all negative. The Widal test was negative and serological tests for Korean hemorrhagic fever, tsutsugamushi disease, or leptospirosis all were negative.
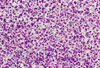
The MRI of the brain was unremarkable. CSF analysis revealed clear CSF with an opening pressure 300 mmH2O, RBC 0/mm3, WBC 283/mm3 (monocytes 98%), glucose 44 mg/dl (blood glucose 79 mg/dl), protein 86 mg/dl, and ADA 15U/L. Polymerase chain reactions for mycoplasma were negative. He was diagnosed as having aseptic meningitis. On the 9th hospital day, multiple tender lymph nodes on the left anterior neck were found. The lymph node biopsy disclosed histopathologic features typical of histiocytic necrotizing lymphadenitis (Fig. 1). He was discharged 1 month after admission. CSF abnormalities and lymphadenopathy resolved with no specific therapy, and he was fully recovered at 4th months of follow up. There was no recurrence of lymphadenopathy or meningitis to date, 36 months after the initial admission.
DISCUSSION
The etiology of KD is still unknown. A few previous reports suggest that viral infection plays a role in its pathogenesis.1,2 Although Ebstein-Barr virus or toxoplasma have been proposed as the causative agent, some investigators think that this is a kind of hyperimmune lymphadenitis induced by sensitized T cells. However, the nature of the proliferating mononuclear cells has not yet been clarified.1,6,8 Although the involvement of the nervous system is rare, aseptic meningitis, acute cerebellar ataxia, acute brachial neuritis and brainstem encephalitis have been reported to be complicated with KD.7,9-15 Because both KD and aseptic meningitis may be associated with viral infection, a common factor possibly related to viral infection may cause aseptic meningitis in the nervous system and KD in the lymphatic system.
Although KD has been known to have a predilection for young woman, the present case was a young male. Some suggest that aseptic meningitis with KD is more likely to occur in males than in females,9 but further epidemiological study is required to prove this. Most cases of aseptic meningitis in KD have been reported in Japan. The incidence of such cases in Korea may have been underestimated. There are some patients with KD who complain of severe systemic symptoms such as fever and headache during the course of the disease. The presence of aseptic meningitis should be suspected in this condition. KD should also be suspected in patients with meningitis of unknown etiology. We emphasize that KD with aseptic meningitis might be overlooked in Korea, because most of the cases worldwide (11 of 13 cases) have been reported in Japan,7,9-11 a nearby country with similar environments.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download