Dear Editor:
A 25-year-old Korean woman presented with 3 months history of multiple, symmetric, red-brown papules on face (Fig. 1A). Facial erythema, flushing and telangiectasia weren't detected. She denied aggravating factors such as alcohol, spicy food intake or any medication. A skin biopsy showed a caseous necrosis surrounded by epithelioid cells (Fig. 1B). She was diagnosed with lupus miliaris disseminates faciei (LMDF). Although patient was treated by minocycline, topical steroid, tacrolimus 0.1% cream, systemic steroid, and doxycycline, LMDF wasn't improve. Finally, it was improved using cyclosporine for 9 months but scars remained (Fig. 1C). One year later, she presented with several skin colored papules on the palms and finger webs (Fig. 1D, E). There was no trauma history. A skin biopsy taken on the index-third finger web showed the same as the previous biopsy (Fig. 1F). Acid-fast bacilli (AFB) stains of specimen and tuberculin skin test were negative. Chest x-ray was normal. We diagnosed as an extrafacial manifestation of LMDF.
LMDF is a rare granulomatous disease presenting dome-shaped red-brown papules on the central face with remarkable preference for the eyelids. LMDF was considered as a variant of lupus vulgaris or a tuberculid because of the histological feature of caseating granuloma. However, LMDF patients didn't showed consistent results of cutaneous hypersensitivity response of tuberculin and PCR techniques demonstrating the DNA of Mycobacteria tuberculosis. LMDF was also considered as a spectrum of sarcoidosis, granulomatous rosacea, and perioral dermatitis. However, in most LMDF cases, histologic features are not consistent with ‘naked granuloma’, and there is no sign of systemic sarcoidosis. LMDF isn't aggravated by sunlight exposure, alcohol or spicy food intake and doesn't show pustules, telangiectasia and flushing compared to rosacea12. In addition, it may sometimes resolve spontaneously with scarring or be refractory to rosacea treatment2. Furthermore, LMDF shows absences of burning, itching, and relationship with topical steroid compared to perioral dermatitis. In pathophysiology, some authors suggested an immune response to the pilosebaceous units contributes to LMDF development. However, LMDF occurred on glabrous skin cannot explain this pathogenesis.
LMDF cases with extrafacial involvement were reviewed by a search in PubMed using LMDF & extrafacial, acne agminata & extrafacial, and LMDF & review as search items up to July 2015. Twenty-one cases have been reported and are summarized in Table 1123456789. Nine cases weren't recorded in details5. It occurred in adults (mean age, 39.25; range 24~63) and sex ratio is 0.71. Four cases in total 21 cases didn't affect face (19%) and 8 cases involved more than two sites. The common sites of extrafacial manifestation are neck (33%), trunk (29%), and axillae (24%). Two cases involving neck showed no facial manifestation. Any cases with extrafacial involvement didn't resolve spontaneously and showed poor response to dapsone, prednisolone, and antibiotics. Seven cases remained scar. In conclusion, LMDF is a distinct disease defined as idiopathic granuloma affecting extrafacial area as well as face after ruling out tuberculosis, rosacea, and sarcoidosis. In addition, LMDF with extrafacial involvement cannot resolve spontaneously and be refractory to treatment.
Figures and Tables
Fig. 1
Clinical images (A, C, D, E) and biopsy specimens (B, F) of the patient. (A) Monomorphous erythematous to brown papules involving the central face at initial visit, (B) biopsy specimen on the chin at initial visit, (C) erythematous macules on her face after cyclosporine treatment, (D, E) firm nodules on palm and the second interdigital web, (F) biopsy specimen of the nodule from interdigital web, (B, F) Histologic images showing tuberculoid granuloma with caseous necrosis surrounded by epithelioid cells (H&E, ×20).
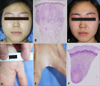
Table 1
Summary of case reports showing lupus miliaris disseminates faciei with extrafacial involvement

| Case | Reference | Race | Age (yr)/sex | Facial involvement | Extrafacial involvement | Treatment | Scar |
|---|---|---|---|---|---|---|---|
| 1 | Kim et al.2 (2008) | Asian | 63/F | N | Neck, chest | Minocycline, doxycycline→NR | Y |
| 2 | van de Scheur et al.1 (2003) | NR | 48/F | Y | Ears, neck, hands, legs |
Minocycline, clofazimine→NR Sulfasalazine+isotretinoin→CR |
Y |
| 3 | van de Scheur et al.1 (2003) | NR | 44/M | Y |
Nape of the neck, both axillae, Umbilical region, penis, scrotum |
Minocycline→NR Prednisolone+dapsone→CR |
ND |
| 4 | van de Scheur et al.1 (2003) | NR | 26/M | Y | Neck, chest |
Sulfasalazine→NR Isotretinoin→CR |
Y |
| 5 | Hillen et al.4 (2006) | White | 36/F | Y | Axillae | ND | ND |
| 6 | Bedlow et al.3 (1998) | ND | 55/F | N | Axillae |
Minocycline, flucloxacillin, dapsone→NR Rifampicin, isoniazid→PR |
Y |
| 7 | Bedlow et al.3 (1998) | ND | 31/F | Y | Axillae, scalp | Flucloxaciline, amoxicillin→NR | Y |
| 8 | Farrar et al.9 (2003) | ND | 53/F | Y | Axillae | ND | ND |
| 9 | Uchiyama and Tsuboi7 (2013) | Asian | 24/M | Y | Scalp | Prednisolone, minocycline→PR | Y |
| 10~12 | Al-Mutairi5 (2011) | ND | ND | Y | Neck | ND | ND |
| 13~15 | Al-Mutairi5 (2011) | ND | ND | Y | Neck, trunk | ND | ND |
| 16~18 | Al-Mutairi5 (2011) | ND | ND | Y | Scalp | ND | ND |
| 19 | Kou et al.8 (2014) | ND | 30/M | N | Trunk, upper extremities | Roxitrhromycin→PR | ND |
| 20 | Nath et al.6 (2011) | ND | 36/M | N | Neck, shoulder | Anti-tubercular therapy→NR | ND |
| 21 | This case | Asian | 25/F | Y | Hands (palms and dorsums) | Minocycline, doxycycline, dapsone, prednisolone→NR cyclosporin→PR | Y |
References
1. van de Scheur MR, van der Waal RI, Starink TM. Lupus miliaris disseminatus faciei: a distinctive rosacea-like syndrome and not a granulomatous form of rosacea. Dermatology. 2003; 206:120–123.

2. Kim DS, Lee KY, Shin JU, Roh MR, Lee MG. Lupus miliaris disseminatus faciei without facial involvement. Acta Derm Venereol. 2008; 88:504–505.

3. Bedlow AJ, Otter M, Marsden RA. Axillary acne agminata (lupus miliaris disseminatus faciei). Clin Exp Dermatol. 1998; 23:125–128.

4. Hillen U, Schröter S, Denisjuk N, Jansen T, Grabbe S. Axillary acne agminata (lupus miliaris disseminatus faciei with axillary involvement). J Dtsch Dermatol Ges. 2006; 4:858–860.

5. Al-Mutairi N. Nosology and therapeutic options for lupus miliaris disseminatus faciei. J Dermatol. 2011; 38:864–873.

6. Nath AK, Sivaranjini R, Thappa DM, Basu D. Lupus miliaris disseminatus faciei with unusual distribution of lesions. Indian J Dermatol. 2011; 56:234–236.

7. Uchiyama M, Tsuboi R. Lupus miliaris disseminatus faciei involving the scalp resulted in cicatricial alopecia. J Dermatol. 2013; 40:760–761.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download