Dear Editor:
Hypohidrotic ectodermal dysplasia (HED) is characterized by a triad of clinical features including absent or diminished eccrine sweat glands, missing teeth, and sparse hair. Frequent skin manifestations of HED are xerosis and periorbital hyperpigmentation over the wrinkled skin, but there was no previous report of acquired dermal melanocytosis (ADM) in HED patient1.
A 26-year-old man presented with bluish patches on the face, which developed one year ago. On physical examination, an alphabet X-shaped bluish patch on the glabella and paranasal cheeks along Blaschko's lines and ovoid bluish patches on the temples were found (Fig. 1A). Typical clinical features of HED such as the characteristic face, dry skin, periorbital hyperpigmentation over the wrinkled skin, sparse hair and teeth were presented (Fig. 1). As he had sparse hair, he got a tattoo on the eyebrows. He also had a history of inability to sweat and recurrent febrile seizures since infancy and complained of high body temperature during the summer. He was diagnosed with atopic dermatitis in childhood. He had no family members showing similar manifestations.
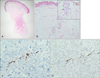
We performed a 3-mm-punch biopsy on the left paranasal cheek, which revealed flattened epidermis, hypoplasia of skin appendages and mild superficial perivascular lymphocytic infiltrations (Fig. 2A). In the dermis, multiple elongated, slightly wavy pigmented cells reacting with melan-A and S-100 were seen (Fig. 2B~D). The clinicopathological findings led to the diagnosis of ADM with HED. We suggested the patient to get genetic study but he refused because of the high cost. The pigmented lesions showed improvement after Q-switched neodymium-doped yttrium aluminium garnet (Nd:YAG) laser treatment.
Periorbital hyperpigmentation in HED usually presents as grayish patch over fine wrinkles just like postinflmmatory hyperpigmentation in atopic dermatitis2. Because the pigmented lesion in our case presented as X-shaped bluish patch without wrinkles, it is clinically different from previously reported cases of periorbital hyperpigmentation in HED. Although there are no biopsied cases of periorbital hyperpigmentation in HED, epidermal hypermelanosis and dermal melanophages may present in those cases like as histopathology of postinflammatory hyperpigmentation and it would be a differential diagnostic point.
The most frequent form of ADM is acquired bilateral nevus of Ota-like macules and other unusual forms of ADM were also reported3. Pathogenesis of ADM is poorly understood, but the faulty activation of dormant or inactive dermal melanocytes is considered as the main pathogenesis4. Various factors, such as ultraviolet (UV) rays, excessive sex hormone, trauma, chronic inflammation, interaction of collagen and elastic fibers or genetic factor can trigger ADM5. In our case, considering mild dermal inflammation seen in the pathology specimen, chronic inflammation is the most like triggering factor, but trauma from tattooing may also be involved. Furthermore, the effect of UV rays cannot be excluded.
As for most dermal pigmentary lesions, the Q-switched Nd:YAG laser is widely accepted treatment for the ADM. Our patient showed clinical improvement of the pigmentation after 8 sessions of Q-switched Nd:YAG laser treatment. Herein, we report a rare case of ADM on the glabella, paranasal cheeks and temples in a patient with HED.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download