Dear Editor:
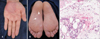
A 60-year-old man presented with erythematous to violaceous annular pruritic patches on both palms and soles for 2 weeks (Fig. 1A, B). No remarkable medical history was reported. Histopathological examination revealed perivascular and interstitial lymphohistiocytic infiltration with abundant eosinophils throughout the dermis and subcutaneous tissue but no flame figure (Fig. 1C). Oral prednisolone combined with cyclosporine was initiated and maintained for 1 month, but the response was poor. The patient never returned to the clinic.
The second case was a 52-year-old man with pruritic erythema on both palms and soles for 4 months. He had no history of either systemic disorder or allergy. Physical examination revealed ill-defined erythematous pruritic patches on the left palm (Fig. 2A). Histopathologically, a minimal vacuolar change at the dermoepidermal junction was observed. Dense perivascular infiltration with lymphohistiocytes and abundant eosinophils was also seen in the superficial and deep dermis (Fig. 2C, D). Neither flame figure nor multinucleated giant cell was observed. Laboratory test results were normal, including eosinophils (0.7%). Systemic and topical steroids with cyclosporine were administered for 9 months but resulted in only transient improvement. Also, the lesion was getting larger and showed a well-demarcated annular feature (Fig. 2B). Therefore, hydroxychloroquine (400 mg daily) was added to oral prednisolone and the skin lesions improved rapidly within a week. There was no remarkable aggravation for 5 months.
Eosinophilic annular erythema (EAE) is a rare figurate erythema that was first described in 20001. According to El-Khalawany et al.2, erythematous small plaques (<5 cm in diameter) in the early clinical stage become larger and more annular in the well-developed stage. Long-standing lesions show pigmented atrophic centers with elevated borders (>10 cm in diameter). Histopathologically, perivascular eosinophilic infiltration is characteristic and becomes more prominent as the lesion develops. EAE is typically known to lack flame figures histopathologically and blood eosinophila (>7%) in laboratory tests, which are hallmarks of Well's syndrome (WS). Clinically, more prominent gyrate erythema is observed compared to WS, and findings such as prodromal burning, painful edema and peripheral induration are absent unlike WS2. However, cases of EAE with flame figures histopathologically along with blood eosinophilia have been reported. Also, well-developed and long standing lesions of EAE are highly compatible with WS2. Therefore, EAE is suggested as a subset of WS23.
EAE shows an excellent response to antimalarials (chloroquine and hydroxychloroquine) unlike classic WS, in which systemic steroid is most effective4. Therefore, antimalarials are suggested as the drug of choice in EAE, and minocyclines, cyclosporine, and dapsone as alternatives23. EAE generally involves trunk or extremities. A case of EAE limited to palms and soles that showed similar features to our cases was recently reported5. That case was associated with thymoma, although the pathogenetic correlation between them was unclear. The case of Iga et al.5 and our cases suggest that EAE migrating mainly to palms and soles may be a unique clinical spectrum of EAE. In addition, hydroxychloroquine with prednisolone is suggested to be first-line treatment for EAE localized to palms and soles.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download