Abstract
Kaposi's sarcoma is a multifocal proliferative vascular tumor involving the skin and other organ and psoriasis is a chronic cutaneous disease with papules and plaques with white scale. Development of Kaposi's sarcoma in psoriasis patients has been reported rarely. A 71-year-old man presented with multiple brownish to violaceous plaques on both feet and arms which were found 4 months ago. The biopsy confirmed Kaposi's sarcoma. The patient was diagnosed with psoriasis vulgaris 10 years ago and Kaposi's sarcoma lesions developed between psoriatic plaques. We herein report a rare case of simultaneous occurrence of Kaposi's sarcoma and psoriasis vulgaris which need quite different treatment.
Psoriasis vulgaris is chronic, immune-mediated skin disease which is common among general population. The pathogenesis of psoriasis is still not yet completely understood, but it is clear that immune cells induce alterations of tissue cell function which lead to regeneration-like reactions of the skin1. Kaposi's sarcoma (KS) is an endothelial proliferating vascular disease with different modes of manifestation and human papillomavirus-8 (HHV-8) is considered to be the necessary cause of all variants of KS2. KS can involve the skin and other internal organs and four clinical subsets are currently recognized: classic, endemic, iatrogenic, and AIDS-related345. Development of KS in psoriasis patients has rarely been reported in spite of the fact that the current treatments of psoriasis are aimed at inhibiting the immune system1. We herein report a 71-year-old man with simultaneous occurrence of KS and psoriasis.
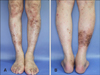
A 71-year-old man presented with multiple violaceous plaques on both feet, legs and arms which were found 4 months ago. Upon physical examination, multiple red-brown to violaceous patches and plaques were noted on his both legs (Fig. 1A) and dorsa of feet and toe webs (Fig. 1B), and a few red-brown papules between psoriatic plaques were found on the elbow (Fig. 2A). The patient did not have any symptoms and the lesions slowly grew in size. He had a 10-year history of psoriasis vulgaris and had been treated with topical agents at a local clinic before he visited our clinic 9 months ago. He had no other remarkable history besides taking calcium-channel blocker for hypertension and had no family history of psoriasis vulgaris or other hereditary disorders.
The biopsy samples from his left sole and elbow showed extensive vascular proliferation with multiple dilated vascular spaces and spindle shaped cells in the dermis (Fig. 3A), and were positive for HHV-8 immunohistochemistry stain (Fig. 3B). The laboratory findings, including a blood chemistry and urinalysis were normal. Tests for human immunodeficiency virus (HIV) and hepatitis B virus were negative. He had previously been treated intermittently with topical corticosteroids and emollients, oral antihistamines, and narrowband ultraviolet B (NB-UVB) phototherapy for psoriasis, but had never taken systemic immunosuppressive treatment. Thus, we led to the conclusion of simultaneous occurrence of classic KS in a patient with psoriasis vulgaris. Upon reviewing the clinical photos taken for psoriasis nine months ago, a few tiny violaceous lesions between psoriatic plaques were noted on his elbow (Fig. 2B, C). Systemic evaluation including abdominal and chest computed tomography (CT) and torso positron emission tomographic-CT showed no signs of internal involvement of KS. He was prescribed with oral pentoxyphylline (1,200 mg/day) and papular lesions were treated with cryotherapy. He received radical radiation therapy of 30 Gy/10 fractions for extensive KS lesions on both legs. The lesions slowly regressed and the follow-up biopsy showed negative in tumor cells in both legs. The patient is under close observation and no recurrence of KS has occurred, however his psoriatic lesions wax and wane.
HHV-8 infection is a common etiology in all four types of KS3456. The development of KS appears to require latent infection of HHV-8. And other cofactors, such as compromised immune system due to HIV or systemic immunosuppressive treatments may contribute to the development of HIV-related and iatrogenic KS, respectively. Genetic factors such as HLA-D25, malnutrition, male gender, mild immunosuppression or immune activation have also been proposed as cofactors in classical KS1.
Simultaneous occurrence of KS and psoriasis is rarely reported in English literatures. To the best of our knowledge, total of nine cases have been reported (Table 1). In reported cases, suspected causes of KS were angiotensin converting eyzme inhibitor3, biologics such as tocilizumab7 and infliximab8, immunosuppressive agents such as fumaric acid esters1 and steroid29, and immune suppression due to underlying diseases610. And in one case, as similar to our case, simultaneous occurrence of KS and psoriasis was found in a patient who had only received NB-UVB therapy11.
Although systemic and topical steroids and immunosuppressive agents are mainstay in the treatment of psoriasis, co-occurrence of psoriasis and KS is very rare. Moreover, five cases (case number 3, 4, 8, 9, and our patient) have been reported where KS developed in psoriasis patients who have not received immunosuppressive agents311. As such, we speculate that besides HHV-8 and immunosuppression, other host-related or environmental cofactors such as male gender, genetic factor, malnutrition, and other factors which need to be elucidated play important roles in much of the development of KS1.
It is easy to diagnose two diseases separately because both have distinctive skin lesions. However, if they are coexistent, making a separate diagnosis can be a challenge. As in our case, KS lesions were hidden in psoriatic plaques in previous clinical photos the patient took about nine months before he was histologically confirmed with KS. Clinicians have to remember that these two diseases may be coexistent, which need quite a different therapy.
Figures and Tables
 | Fig. 2(A) A few angiomatous papules between psoriatic plaques on the elbow. (B) Violaceous lesions suspicious of Kaposi's sarcoma were hidden between extensive psoriatic lesions in clinical photos taken nine months ago. (C) Closer view (arrows: violaceous lesions suspicious of Kaposi's sarcoma between psoriatic lesions). |
 | Fig. 3(A) Extensive vascular proliferation with multiple dilated vascular spaces of back-to-back configuration and spindle shaped cells in the dermis (H&E, ×100). (B) Positive for human papillomavirus-8 (HHV-8 immunohistochemistry stain, ×100). |
Table 1
Summary of reported cases of KS in psoriasis patients

| Author | No. | Age (yr)/sex | Type of KS | Duration of psoriasis (yr) | Comorbidities | Suspected cause of KS (duration of treatment) |
|---|---|---|---|---|---|---|
| Philipp et al.1 | 1 | 60/M | Iatrogenic | 40 | - | Fumaric acid esters (25 months) |
| Tebbe et al.2 | 2 | 59/M | Iatrogenic | 46 | Chronic obstructive lung disease | Prednisolone treatment (5 months) |
| Dervis and Demirkesen3 | 3 | 54/F | Classic | 29 | Hypertension | Cilazapril (ACEi) (9 months) |
| Sorce and Bongiorno6 | 4 | 74/F | Classic | 15 | Hypertension, vitiligo, monoclonal gammopathy of undetermined significance | Immune dysregulation underlying chronic inflammatory disorders |
| Verdelli et al.7 | 5 | 78/F | Iatrogenic | - | - | Tocilizumab (13 months) |
| Ursini et al.8 | 6 | 49/M | Iatrogenic | 9 | Diabetes mellitus | Infliximab (15 months) |
| Selvi et al.9 | 7 | 75/F | Iatrogenic | 30 | - | Intra-articular steroid injection for psoriatic arthritis |
| Fargnoli et al.10 | 8 | 56/M | Classic | 20 |
Down syndrome, Hodgkin’s lymphoma |
Down syndrome-related compromised immune surveillance |
| Häring et al.11 | 9 | 46/M | Classic | 10 | - | UV light therapy |
| Our case | 71/M | Classic | 10 | Hypertension | Unknown, maybe due to immune dysregulation under chronic inflammatory dermatosis, psoriasis |
References
1. Philipp S, Kokolakis G, Hund M, Witte E, Witte K, Kunz S, et al. Immunological changes in psoriasis patients under long-term treatment with fumaric acid esters: risk of Kaposi sarcoma occurrence? Eur J Dermatol. 2013; 23:339–343.

2. Tebbe B, Mayer-da-Silva A, Garbe C, von Keyserlingk HJ, Orfanos CE. Genetically determined coincidence of Kaposi sarcoma and psoriasis in an HIV-negative patient after prednisolone treatment. Spontaneous regression 8 months after discontinuing therapy. Int J Dermatol. 1991; 30:114–120.

3. Dervis E, Demirkesen C. Kaposi's sarcoma in a patient with psoriasis vulgaris. Acta Dermatovenerol Alp Pannonica Adriat. 2010; 19:31–34.
4. Dukers NH, Rezza G. Human herpesvirus 8 epidemiology: what we do and do not know. AIDS. 2003; 17:1717–1730.
5. Lee DK, Chon KJ, Son SJ, Kim DJ, Cho DI. A case of AIDS-related Kaposi's sarcoma. Ann Dermatol. 2000; 12:211–214.

6. Sorce M, Bongiorno MR. Simultaneous diagnosis of Kaposi's sarcoma, psoriasis, vitiligo and monoclonal gammopathy of undetermined significance in an immunocompetent patient. J Dermatol. 2013; 40:479–480.

7. Verdelli A, Bonciani D, Bonciolini V, Caproni M. Is tocilizumab safe in Kaposi sarcoma? A complex association among rheumatoid arthritis, psoriasis, and Kaposi sarcoma. Clin Drug Investig. 2014; 34:437–438.

8. Ursini F, Naty S, Mazzei V, Spagnolo F, Grembiale RD. Kaposi's sarcoma in a psoriatic arthritis patient treated with infliximab. Int Immunopharmacol. 2010; 10:827–828.

9. Selvi E, De Stefano R, Manganelli S, Marcolongo R. Kaposi's sarcoma in psoriatic arthritis. Rheumatology (Oxford). 2003; 42:389.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download