Abstract
Background
Seborrheic dermatitis (SD) is a multifactorial disease; Malassezia species play an important role in its pathogenesis.
Objective
We aimed to determine whether a cream containing climbazole/piroctone olamine (C/P cream), antifungal agents with expected efficacy against Malassezia species, could improve SD symptoms.
Methods
We instructed 24 patients with mild-to-moderate SD to apply the C/P cream and emollient cream on the right and left sides of the face, respectively, every morning and evening for 4 weeks. The casual sebum level (measured with Sebumeter®; Courage & Khazaka Electronic GmbH, Germany) and the extent of erythema (measured with Mexameter®; Courage & Khazaka Electronic GmbH) on the face were measured at baseline and after 4 weeks. The minimal inhibitory concentration (MIC) was determined to demonstrate the antifungal activity of the C/P cream.
Results
The casual sebum level and erythema were measured at week 4, and the median values demonstrated a quantitative improvement on the C/P cream-treated right side of the face compared to the emollient cream-treated left side. For the C/P cream, the MICs were 0.625, 5, 0.625, and 2.5 mg/ml for Malassezia restricta, M. globosa, M. sympodialis, and M. slooffiae, respectively.
Seborrheic dermatitis (SD) is a chronic dermatitis that affects 1%~3% of the population1. SD is characterised by sharply defined erythematous patches and plaques with greasy-looking, yellowish scales on seborrheic areas such as the scalp, face, upper trunk, and flexures. The growth of Malassezia species was suggested as an important pathogenic factor of SD23, as demonstrated by studies that showed that SD was improved by the use of antifungal agents45. Current treatment options include antifungal drugs, anti-inflammatory agents (steroids, calcineurin inhibitors, and lithium salts), keratolytic agents, and phototherapy. SD is usually treated with topical corticosteroids and antifungals. However, prolonged use of topical steroids may cause adverse effects such as skin atrophy, telangiectasia, rosacea, and acne. The use of topical antifungal agents in the treatment of mild SD is well established. Itraconazole can be prescribed for moderate to severe facial SD and result in significant clinical improvement and decrease in the growth of Malassezia species6.
The cream containing climbazole/piroctone olamine (C/P cream) (Sensibio DS+®; Bioderma Laboratoire Dermatologique, Lyon, France) tested in this study is a cosmetic product containing piroctone olamine and climbazole. Piroctone olamine, the ethanolamine salt of the hydroxamic acid derivative piroctone, is a hydroxypyridone anti-mycotic agent. Climbazole is an imidazole antifungal agent. A non-steroidal cream containing piroctone olamine was reported to effectively treat SD by inhibiting the growth of Malassezia species7, and a shampoo containing piroctone olamine and climbazole effectively reduced dandruff by suppressing the growth of Malassezia8. However, no study thus far has reported on an over-the-counter product containing piroctone olamine and climbazole for the treatment of facial SD. We aimed to evaluate the efficacy and safety of C/P cream in the treatment of facial SD.
This 4-week single-center, open-label split-face study was approved by the institutional review board of Konkuk University Medical Center (IRB no. KUH1120054). All of the patients included in this study signed an informed consent form. The participants were 24 patients diagnosed with facial symmetric mild-to-moderate SD by a dermatologist. The severity of SD9 was determined by using two scales; one scored erythema, plaque, infiltration, and pustules as absent (0), mild (1), moderate (2), or severe (3), and the other scored the extent of lesions as less than 10% (1), 10%~30% (2), 30%~50% (3), 50%~70% (4), or more than 70% (5). The total score was calculated by multiplying the severity by the lesion area of erythema, plaque, infiltration, and pustules, respectively, and adding the scores of all four items. The total scores were categorised into mild (≤5 points), moderate (6~11), or severe (12~60). Patients who used any oral drug that could affect the condition of the skin (steroids, antibiotics, antifungal agents, antihistamines, etc.) within 4 weeks of study entry or any therapeutic external preparation within 2 weeks of study entry were excluded. Patients with a skin disease other than SD and those who underwent a facial procedure within 6 months of study entry were excluded as well.
The patients were instructed to apply C/P cream (Sensibio DS+®), which contains climbazole and piroctone olamine, on the right side of the face and emollient cream (Atoderm®; Bioderma Laboratoire Dermatologique), a moisturizer that does not contain climbazole and piroctone olamine, on the left side every morning and evening for 4 weeks. The use of other cosmetics, therapeutic external preparations, and drugs that could affect the clinical trial was prohibited during the study. At the baseline visit and at 4 weeks, (1) Sebumeter® and Mexameter® (Courage & Khazaka Electronic GmbH, Cologne, Germany) were used to measure the casual sebum level and most intense erythema on the forehead and cheek on both sides; and (2) patients were asked to subjectively score their itchiness, burning sensation, erythema, scaling, and tightness on each side of the face as none, 0; mild, 1; moderate, 2; or severe, 3. This research was conducted in winter from November to December.
Safety was assessed by inquiring about local irritation or other adverse events by using questionnaires.
To determine the antifungal activity of the C/P cream and emollient cream against specific Malassezia species strains, their minimal inhibitory concentrations (MICs) were measured in a laboratory. MIC is the lowest concentration of antifungals or antibiotics that will inhibit the visible growth of a microorganism after overnight incubation. Malassezia restricta, M. sympodialis, and M. slooffiae were isolated and identified at Konkuk University Medical Center, South Korea, and M. globosa (Centraalbureau voor Schimmelcultures [CBS] 7966) was purchased from the CBS Fungal Biodiversity Center. These strains were grown on Leeming and Notman agar medium10 (0.5% glucose, 1% polypeptone, 0.01% yeast extract, 0.8% bile salt, 0.1% glycerol, 0.05% glycerol monostearate, 0.05% tween 60, 1.2% agar, 0.5% whole fat cow milk, and 170 µg/ml chloramphenicol). Susceptibility testing of the C/P cream and emollient cream was performed according to a method described previously11. Antifungal assays were repeated twice, and identical results were obtained.
The patients' mean age was 35.37 years. We enrolled 24 Korean patients (6 men and 18 women), none of whom withdrew from the study.
The casual sebum level and extent of erythema on the left- and right-side forehead and cheek were measured by using Sebumeter® and Mexameter® , and compared at baseline and 4 weeks. At week 4, the C/P cream-treated area showed a statistically significant reduction in the median casual sebum level on the forehead (marked with a black bold line in Fig. 1) compared to the emollient cream-treated area (p=0.011). On the cheek, the C/P cream-treated area also showed a lower median casual sebum level compared to the emollient-treated area, but this was not statistically significant (Fig. 1). At week 4, the C/P cream-treated area showed a statistically significant reduction (p=0.002) in median erythema level compared to the emollient cream-treated area, on both the forehead and the cheek (Fig. 2).
A questionnaire was administered at baseline and 4 weeks to determine differences in symptoms between the left and right sides of the face (Fig. 3, 4). The week 4 median itchiness, burning sensation, and erythema were reduced in both the C/P cream-treated area and emollient cream-treated area, suggesting that the patients' subjective symptoms improved with both treatments; there was no statistically significant difference between the two treatments.
No serious adverse effects requiring medical treatment were reported, although 2 patients reported a temporary pricking sensation after application of the C/P cream.
The antifungal activity of the C/P cream and emollient cream against Malassezia species was measured (Table 1). The MIC of the C/P cream, an index indicating antifungal agent activity, was 0.625 mg/ml for M. restricta, 5 mg/ml for M. globosa, 0.625 mg/ml for M. sympodialis, and 2.5 mg/ml for M. slooffiae, indicating antifungal activity against all the aforementioned species. The C/P cream is a crude mixture. The concentrations of climbazole and piroctone olamine, which are single compounds with antifungal action, were re-evaluated in order to determine whether their antifungal activities were proportionate to the amounts of their active ingredients. This substance was also shown to be effective against M. restricta, M. globosa, M. sympodialis, and M. slooffiae. The emollient cream was not observed to exert any antifungal activity.
The pathophysiological mechanism of SD remains unclear. Although Malassezia species are a part of the normal microflora found on normal skin of 75% to 98% of healthy adults12, its role in SD has been supported by the positive correlation between the population density of Malassezia species on the skin and the severity of SD13, as well as the high therapeutic efficacy of antifungal agents in SD14. The current understanding of the pathophysiological mechanism of SD suggests a role of Malassezia species in triggering inflammatory and hyper-proliferative epidermal responses15. The following are the four sequential pathophysiological phases of SD15: 1) Malassezia ecosystem and interaction with the epidermis; 2) initiation and propagation of inflammation; 3) disruption of proliferation and differentiation processes of the epidermis; and 4) physical and functional skin barrier disruption. According to these phases, if the proliferation of Malassezia species is controlled, the progression of the pathophysiological phases of SD and its signs and symptoms would be improved.
Climbazole [(1-4-chlorophenoxy)-1-(1H-imidazonyl)-3,3-dimethylbutan-2-one] is an imidazole antifungal agent commonly used in the treatment of human fungal skin infections such as dandruff and SD. Similarly, with other azole antifungal agents, climbazole is thought to exhibit antifungal activity by inhibiting ergosterol, a major component of fungal cytoplasmic membranes. Azoles that bind to a cytochrome P-450 molecule are involved in the synthesis of ergosterol16. Azoles bind by their basic nitrogen to the heme iron and by their N-1 substituent to the protein moiety of fungal P-450s, resulting in the blocking of P-450-mediated reactions17.
Piroctone olamine [1-hydroxy-4-methyl-6(2,4,4-trimethylpentyl)-2(1H)-pyridone, 2-aminoethanol salt] is a pyridine derivate, as is ciclopirox olamine. It is a component of many cosmetic products such as anti-dandruff shampoo and is known to have a fungicidal effect. Piroctone olamine penetrates the cell membrane and forms complexes with iron ions, inhibiting energy metabolism in mitochondria18. Piroctone olamine has been approved for use in cosmetic products at a maximal concentration of 1% (rinse-off products) or 0.5% (other products).
The C/P cream tested in this study is a topical agent containing both climbazole and piroctone olamine, as well as other effective ingredients such as 18β-glycyrrhetinic acid and golden algae extract (Laminaria ochroleuca). 18β-glycyrrhetinic acid is extracted from the root of the liquorice plant, a perennial plant with upright stems covered with leaves and lilac-coloured flowers. It provides immediate relief owing to its endogenous anti-inflammatory properties19. Golden algae extract (L. ochroleuca) is a lipidic extract of golden algae. It reduces skin reactivity by inhibiting the synthesis of the cytokines involved in the irritation20.
The patients in the present study showed significant improvements in SD according to the results of Sebumeter® and Mexameter®. In the patient satisfaction questionnaire, patients reported an improvement in itchiness, burning sensation, and erythema in both the C/P cream-treated right side of the face and emollient cream-treated left side. But because there was no marked difference between the right and left sides, it may have been difficult for patients to sense and describe the symptom improvement separately.
The advantages of the C/P cream are that it can be purchased without prescription, can replace lotion applied every day after facial wash, and can mitigate the symptoms of SD without serious adverse effects that require medical treatment. The disadvantage was that the moisturising effect was not sufficient to prevent skin tightness in the winter; the patients often mentioned that they would like to use it in the summer.
We determined the MICs for Malassezia species in order to examine the antifungal activity of the C/P cream. The C/P cream is a crude mixture, and simple comparison with single compounds in terms of MIC for Malassezia species may not be feasible. To resolve this issue, we re-examined the concentrations of climbazole and piroctone olamine to determine whether their active ingredients validly reflected their degree of antifungal activity. Schmidt and Rühl-Hörster21 found that the MICs of climbazole and ketoconazole for M. furfur were <0.06 µg/ml. In another study, Schmidt22 found that the MIC of climbazole for M. pachydermatis was <0.06 µg/ml. Prabhamanju et al.23 reported that for M. furfur , the MIC of climbazole was 20 µg/ml and that of piroctone olamine was 5 µg/ml. Gokulshankar et al.24 reported that the MICs of climbazole for M. furfur, M. globosa , and M. restricta were 62.5, 125, and 125 µg/ml, respectively. Considering the above-mentioned findings in the literature, climbazole and piroctone olamine in the C/P cream can be expected to have antifungal activities against M. restricta, M. globosa, M. sympodialis, and M. slooffiae.
The use of cultural and phenotypical typing methods resulted in contradictory data about the proportion of Malassezia species in SD252627. However, the molecular analysis of Malassezia species in SD demonstrated that M. restricta was consistently the most common282930. According to a study on the distribution of Malassezia species in the human body that used 26S rDNA polymerase chain reaction (PCR)-restriction fragment length polymorphism, M. restricta was detected dominantly in the forehead, cheeks, and chest of Korean patients with SD31. In a study involving Japanese patients with facial SD, M. globose (93.5%) and M. restricta (61.3%) were the two most commonly detected Malassezia species by using a PCR-based, non-culture dependent method18. Considering the antifungal activity of the C/P cream against M. restricta, M. globosa, M. sympodialis, and M. slooffiae, the SD symptoms seemed improved by its antifungal activity against Malassezia species especially M. restricta, the most frequently occurring species on the face.
SD shows a strong correlation with sebaceous gland activity32. SD is most common in adolescence and young adulthood, when sebaceous glands are at their most active. In addition, the SD lesions were distributed on parts of the body where sebaceous glands were present, such as the face, scalp, chest, and back1. SD is considered to be a Malassezia driven disease23 and Malassezia species require lipids32. We measured the casual sebum level expecting that a reduction in the amount of casual sebum would be associated with reduced proliferation of Malassezia species, which would result in an improvement in the symptoms of SD. Looking at the final results, since the symptoms of SD seemed to improve in the C/P cream-treated right facial side which also showed a notable reduction in its casual sebum level, this suggests that reducing the casual sebum level may assist indirectly in improving the symptoms of SD.
This study has some limitations. This was a simple, single-center open-label study. The number of patients was small (n=24). The long-term efficacy of the C/P cream tested was not evaluated. Therefore, additional clinical data are required to determine the long-term efficacy and safety of the C/P cream tested.
In conclusion, based on the reduction of the casual sebum level and the extent of erythema, this C/P cream with antifungal activity against Malassezia species seems useful for the treatment of mild-to-moderate SD. The objective improvement in SD was associated with anti-Malassezia activity of C/P cream.
Figures and Tables
Fig. 1
The casual sebum level measured using Sebumeter® and Mexameter® (Courage & Khazaka Electronic GmbH, Germany) at baseline and week 4. A p-value<0.05 was considered statistically significant (*p<0.05). C/P cream: cream containing climbazole/piroctone olamine.
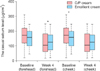
Fig. 2
Erythema measured using Sebumeter® and Mexameter® (Courage & Khazaka Electronic GmbH, Germany) at baseline and week 4. A p-value<0.05 was considered statistically significant (*p<0.05). C/P cream: cream containing climbazole/piroctone olamine.

Fig. 3
Symptom intensity reported by patients at baseline. C/P cream: cream containing climbazole/piroctone olamine.

Fig. 4
Symptom intensity reported by patients at week 4. C/P cream: cream containing climbazole/piroctone olamine.

Table 1
Minimal inhibitory concentration measured to determine the antifungal activity of the cream containing climbazole/piroctone olamine (C/P cream)
ACKNOWLEDGMENT
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT, and Future Planning NRF-2013R1A1A2007863 and Bioderma Laboratoire Dermatologique.
Bioderma Laboratoire Dermatologique provided the research funding, as well as the Sensibio DS+® and Atoderm® distributed to the patients free of charge, but had no participation in the study proceedings, data analysis, or the process of manuscript preparation and submission.
References
2. Elewski BE. Safe and effective treatment of seborrheic dermatitis. Cutis. 2009; 83:333–338.
3. Gupta AK, Bluhm R, Cooper EA, Summerbell RC, Batra R. Seborrheic dermatitis. Dermatol Clin. 2003; 21:401–412.

4. Alizadeh N, Monadi Nori H, Golchi J, Eshkevari SS, Kazemnejad E, Darjani A. Comparison the efficacy of fluconazole and terbinafine in patients with moderate to severe seborrheic dermatitis. Dermatol Res Pract. 2014; 2014:705402.

5. Kastarinen H, Okokon EO, Verbeek JH. Topical antiinflammatory agents for seborrheic dermatitis of the face or scalp: summary of a Cochrane Review. JAMA Dermatol. 2015; 151:221–222.

6. Shemer A, Kaplan B, Nathansohn N, Grunwald MH, Amichai B, Trau H. Treatment of moderate to severe facial seborrheic dermatitis with itraconazole: an open noncomparative study. Isr Med Assoc J. 2008; 10:417–418.
7. Del Rosso JQ. Adult seborrheic dermatitis: a status report on practical topical management. J Clin Aesthet Dermatol. 2011; 4:32–38.
8. Schmidt-Rose T, Braren S, Fölster H, Hillemann T, Oltrogge B, Philipp P, et al. Efficacy of a piroctone olamine/climbazol shampoo in comparison with a zinc pyrithione shampoo in subjects with moderate to severe dandruff. Int J Cosmet Sci. 2011; 33:276–282.

9. Barac A, Pekmezovic M, Milobratovic D, Otasevic-Tasic S, Radunovic M, Arsic Arsenijevic V. Presence, species distribution, and density of Malassezia yeast in patients with seborrhoeic dermatitis-a community-based case-control study and review of literature. Mycoses. 2015; 58:69–75.

10. Leeming JP, Notman FH. Improved methods for isolation and enumeration of Malassezia furfur from human skin. J Clin Microbiol. 1987; 25:2017–2019.

11. Sugita T, Tajima M, Ito T, Saito M, Tsuboi R, Nishikawa A. Antifungal activities of tacrolimus and azole agents against the eleven currently accepted Malassezia species. J Clin Microbiol. 2005; 43:2824–2829.

12. Dessinioti C, Katsambas A. Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies. Clin Dermatol. 2013; 31:343–351.
13. Heng MC, Henderson CL, Barker DC, Haberfelde G. Correlation of Pityosporum ovale density with clinical severity of seborrheic dermatitis as assessed by a simplified technique. J Am Acad Dermatol. 1990; 23:82–86.

14. Schwartz RA, Janusz CA, Janniger CK. Seborrheic dermatitis: an overview. Am Fam Physician. 2006; 74:125–130.
15. Schwartz JR, Messenger AG, Tosti A, Todd G, Hordinsky M, Hay RJ, et al. A comprehensive pathophysiology of dandruff and seborrheic dermatitis-towards a more precise definition of scalp health. Acta Derm Venereol. 2013; 93:131–137.

16. Van den Bossche H, Willemsens G, Cools W, Cornelissen F, Lauwers WF, van Cutsem JM. In vitro and in vivo effects of the antimycotic drug ketoconazole on sterol synthesis. Antimicrob Agents Chemother. 1980; 17:922–928.

17. Joly V, Bolard J, Yeni P. In vitro models for studying toxicity of antifungal agents. Antimicrob Agents Chemother. 1992; 36:1799–1804.

18. Kim Y, Alpmann P, Blaum-Feder S, Krämer S, Endo T, Lu D, et al. Increased in vivo efficacy of lenalidomide by addition of piroctone olamine. In Vivo. 2011; 25:99–103.
19. Scrivener Y, Cribier B. Pathogenesis of seborrheic dermatitis. Ann Dermatol Venereol. 2004; 131:119–122.
20. Tsukahara M, Nishino T, Furuhashi I, Inoue H, Sato T, Matsumoto H. Synthesis and inhibitory effect of novel glycyrrhetinic acid derivatives on IL-1 beta-induced prostaglandin E(2) production in normal human dermal fibroblasts. Chem Pharm Bull (Tokyo). 2005; 53:1103–1110.

21. Schmidt A, Rühl-Hörster B. In vitro susceptibility of Malassezia furfur against azole compounds. Mycoses. 1996; 39:309–312.
22. Schmidt A. In vitro activity of climbazole, clotrimazole and silver-sulphadiazine against isolates of Malassezia pachydermatis. Zentralbl Veterinarmed B. 1997; 44:193–197.

23. Prabhamanju M, Gokul Shankar S, Babu K, Ranjith MS. Herbal vs. chemical actives as antidandruff ingredients-which are more effective in the management of dandruff?-an overview. Egypt Dermatol Online J. 2009; 5:8.
24. Gokulshankar S, Ranjith MS, Sumithira , Ranganathan S, Manuel F, Mohanty BK. Factors determining the antidandruff effect of climbazole in a shampoo formulation. J Appl Cosmetol. 2011; 29:135–140.
25. Crespo Erchiga V, Ojeda Martos AA, Vera Casaño A, Crespo Erchiga A, Sánchez Fajardo F. Isolation and identification of Malassezia spp. In pytiriasis versicolor, seborrheic dermatitis and healthy skin. Rev Iberoam Micol. 1999; 16:S16–S21.
26. Sandström Falk MH, Tengvall Linder M, Johansson C, Bartosik J, Bäck O, Särnhult T, et al. The prevalence of Malassezia yeasts in patients with atopic dermatitis, seborrhoeic dermatitis and healthy controls. Acta Derm Venereol. 2005; 85:17–23.

27. Gupta AK, Kohli Y, Summerbell RC, Faergemann J. Quantitative culture of Malassezia species from different body sites of individuals with or without dermatoses. Med Mycol. 2001; 39:243–251.

28. Tajima M, Sugita T, Nishikawa A, Tsuboi R. Molecular analysis of Malassezia microflora in seborrheic dermatitis patients: comparison with other diseases and healthy subjects. J Invest Dermatol. 2008; 128:345–351.

29. Patiño-Uzcátegui A, Amado Y, Cepero de García M, Chaves D, Tabima J, Motta A, et al. Virulence gene expression in Malassezia spp from individuals with seborrheic dermatitis. J Invest Dermatol. 2011; 131:2134–2136.

30. Lee YW, Byun HJ, Kim BJ, Kim DH, Lim YY, Lee JW, et al. Distribution of malassezia species on the scalp in korean seborrheic dermatitis patients. Ann Dermatol. 2011; 23:156–161.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download