Abstract
Background
Physicians can play a crucial role in the knowledge that patients have about a disease and its prognosis. Recently, patients with atopic dermatitis (AD) are increasingly turning from western medicine to oriental herbal medicine. However, their awareness of AD and attitude toward Western medicine and oriental herbal medicine clinics are scarcely reported.
Objective
The aim of this study was to determine the understanding of AD among patients and their parents and to identify their awareness of and attitude toward Western medicine and oriental herbal medicine as treatments for AD.
Methods
An online questionnaire was administered to 500 consenting respondents with AD (age, 16~49 years) and parents of children with AD (age, 0~15 years).
Results
The mean percentage of correct answers to questions about AD was 52.54%. A parental history of AD was independently associated with higher respondent’s knowledge about the disease and its treatment. The satisfaction with treatment outcomes was highest among patients treated at private clinic of dermatology specialists (49.4%), while lowest among those treated at oriental herbal medicine clinics (38.4%). Many participants were aware that oriental herbal medicine requires a longer treatment period for a cure and does not burden the skin, while steroid phobia was seen in most of participants.
Atopic dermatitis (AD) is a common chronic inflammatory skin disease that has many pathogenetic factors, including genetic, immunological, and environmental ones. AD is accompanied by numerous health disorders, such as asthma, allergic rhinitis, conjunctivitis, and food allergy. Although it mostly develops in infancy or early childhood, 2%~3% of adults are also affected123. The prevalence of AD is about 30% in most developed countries, and this has increased considerably in recent decades4567. AD is associated with a significant negative economic burden and impacts the quality of life (QoL) of patients and their families8910.
The understanding of AD patients about the disease is as important as the medical care provided to them. Previous studies have supported that compliance with AD management practices and knowledge of patients and their parents about AD are important to improving clinical outcomes11121314. However, many patients with AD do not fully understand their disease and its treatment1516.
The role of medical institutions in the treatment of AD has become increasingly important in terms of providing education about AD and its treatment. Many patients with AD visit various medical institutes and are confused about the treatment they need. According to recent reports, complementary and alternative medicines (e.g., oriental herbal medicines) are have emerging, due owing to the chronic course of AD. However, the studies regarding the awareness of Western medicine and oriental herbal medicine treatments among patients with AD are scarce.
The aim of this study was to determine the understanding that AD patient and their parents have about the disease and its treatment, and to elucidate their awareness of and attitude toward Western medicine and oriental herbal medicine as treatments for AD.
Eligible participants for this study were males or females aged 16~49 years with AD and parents with children aged 0~15 years with AD who were diagnosed at a medical institution. We performed proportional quota sampling using the proportions of participants with AD according to age and sex. The questionnaire developed for this survey by the investigators was implemented on the Internet via the Macromillembrain agency, and the data were collected online from 500 eligible patients during September 5~23, 2014. The patients were informed that the questionnaire was anonymous and confidential, and all of those who agreed to be involved provided written informed consent to participate. The protocol was approved by the institutional review board of Konkuk University Hospital (IRB no. KUH1120071), in accordance with the principles of Good Clinical Practice and the Helsinki Guidelines.
This questionnaire survey was developed through the Korean Atopic Dermatitis Association and was composed of four parts: sociodemographic characteristics of the participants, AD knowledge, AD treatment behavior, and awareness and satisfaction of Western medicine and oriental herbal medicine for treating AD.
The survey included questions on the living area, age, sex, marital status of respondents, Patient-Oriented SCORing Atopic Dermatitis (PO-SCORAD) score, onset of AD, and parental history of AD. PO-SCORAD scores were divided into the following four categories: <15, mild; 15~40, moderate; 41~49, severe; and ≥50, very severe17. AD knowledge was addressed with 10 questions, and participants were asked to choose all of the phrases that they agreed with. The percentage of correct answers was calculated.
AD treatment behavior was assessed by asking the respondents what they did the first time they thought they had AD symptoms, and asking whether they regularly visited a medical institution for AD treatment, and which of the following interventions they performed to treat AD when symptoms became aggravated: visiting a medical institution, frequently applying an emollient, modifying their lifestyle including eating habits, applying topical steroids, or taking systemic steroids (multiple answers were allowed). The respondents were asked whether they have ever used topical or systemic steroids, whether they were satisfied with steroid treatment, and about their attitudes toward and awareness of steroids. The respondents were also asked how much they spent per annum on treatments for AD.
The respondents were asked which of the following they thought would be the most effective method for improving their symptoms: Western medicine treatment, oriental herbal medicine treatment, steady use of an emollient, or lifestyle modifications including eating habits. The respondents were further asked which type of medical institution they preferred to use for receiving AD treatment, from the following choices: a private clinic of dermatology specialists, a private clinic of pediatric specialists, a university hospital dermatology clinic, a university hospital pediatric clinic, or an oriental herbal medicine clinic (multiple answers were allowed). The respondents provided a rating for their satisfaction with treatment at all institutions where they had been treated, and were asked to choose phrases describing their perceptions of the Western medicine and oriental herbal medicine treatments for AD.
We used PASW Statistics ver. 17.0 (IBM Co., Armonk, NY, USA) to analyze the data. The χ2 test was used to analyze the proportions and means of categorical variables, and the two-sample t-test and Kruskal-Wallis test were used for continuous variables. An ANOVA trend test was used to determine the annual expenditure according to disease severity. A probability value of p<0.05 was considered to be indicative of statistical significance. A multivariate linear regression analysis was used to examine the level of AD knowledge after controlling for demographic characteristics (sex, age, living area, marital status, disease onset, and parental history of AD). Variables with probability values of p≤0.10 in the univariate analysis were selected for the multivariate analysis with linear regression.
The demographic information of the patients and respondents is presented in Table 1. We represent “Patients” as those aged 16~49 years with AD, and if parents answered this questionnaire, their children aged 0~15 years with AD. We represent “Respondents” as those who answered this questionnaire (parents with children aged 0~15 years with AD and individuals aged 16~49 years with AD).
The age of the respondents was 32.58±8.40 years (mean±standard deviation [SD]). Of all respondents, 89.2% lived in an urban area and 10.8% lived in a rural area, 61.6% were married and 38.4% were unmarried. Most of the patients had AD of moderate severity (57.4%), followed by severe (19.4%), very severe (17.0%), and mild (6.2%). The overall PO-SCORAD score was 35.80±14.81 (range, 0.90~87.10). A parental history of AD was present in 41.2% of the patients, and 0~2 years was the most common time range for disease onset (37.4%), followed by 3~6 years (26.2%), 7~9 years (10.0%), 10~12 years (6.0%), 19~24 years (5.4%), 16~18 years (5.2%), 13~15 years (4.8%), 25~29 years (1.8%), 30~34 years (1.8%), 35~39 years (0.8%), and 40~44 years (0.6%).
The percentage of correct answers to questions about AD was 52.54%±11.58% (range, 20.0%~90.0%). The univariate regression analysis revealed that age, disease severity, marital status, and parental history of AD were significantly associated with knowledge about AD (p=0.0153, 0.0161, 0.0406, and <0.0001, respectively). The multivariate analysis revealed that only the parental history of AD was a significant predictor. The percentage of correct answers was 4.68% higher among those with a parental history of AD than those without such a history (p<0.0001; 95% confidence interval, 2.65~6.71; Table 2).
The most common management decision for respondents when suspecting AD was visiting a medical institution (43.6%), followed by emollient application (26.8%), AD ointment application (20.8%), and lifestyle modifications including eating habits (8.8%). Younger patients preferred applying emollients over specialized ointments, whereas adults preferred applying an emollient and a specialized ointment (p<0.0001); these preferences did not significantly vary with AD severity (p=0.823). Only 19.8% of the patients reported that they visited a medical institution regularly.
The respondents were asked what they did when their AD symptoms became aggravated. The most common treatment was applying emollient more frequently (64.4%), followed by visiting a medical institution (58.4%), lifestyle modifications including eating habits (43.4%), applying topical steroids (40.4%), and taking systemic steroids (4.4%).
The respondents most commonly spent 150,000~350,000 Korean won (KRW; 1,200 KRW is approximately equal to one US dollar) annually (mean±SD, 519,100±790,300 KRW). The patients who were aged 40~44 years spent the most on AD treatment annually (1,027,500±1,349,400 KRW, p<0.0001). The annual expenditure on AD treatment did not differ between men and women (561,700±833,900 KRW and 473,300±739,500 KRW, respectively; p=0.2118). In terms of expenditure relative to disease severity, this was highest among those with very severe disease (865,100±1,046,700 KRW), followed by those in the severe (575,900±857,200 KRW), moderate (435,800±679,200 KRW), and mild (164,200±159,700 KRW) groups (p<0.0001, Table 3).
About 91% of the patients had used topical steroids, and 28.8% had used systemic steroids. Of those treated with a steroid, 75.7% were satisfied with the treatment, while 15.1% were fairly satisfied, and 9.2% were not satisfied. Regarding steroid treatment, most (65.4%) answered that they used steroids minimally only when the symptoms become aggravated, followed by those who used a steroid first if the symptoms become aggravated (22.2%), and those who never used steroid even if their symptoms were aggravated (12.4%). For questions of awareness of using steroids, about 70% of respondents were aware that topical steroids could be addictive even if used once, 67.4% were aware that chronic use of a topical steroid can be harmful, 35.6% were aware that topical steroids produce skin atrophy as a side effect, and 10.4% were aware that a topical steroid had the same effect as a systemic steroid.
In response to the question about which treatment they considered to be the most effective for AD, most respondents answered lifestyle modifications (43.5%), followed by steady use of an emollient (26.7%), Western medicine treatment (26.1%), and oriental herbal medicine treatment (3.7%). Of those who were receiving treatment at a medical institution, most respondents preferred a private clinic of dermatology specialists (59.6%), followed by a private clinic of pediatric specialists (23.2%), a university hospital dermatology clinic (22.2%), a university hospital pediatric clinic (12.1%), and an oriental herbal medicine clinic (9.1%).
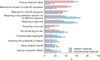
Forty-one point six percent of respondents were satisfied with a university hospital dermatology clinic, 42.9% said they were fairly satisfied, and 15.6% were not satisfied. Forty-one point eight percent of respondents were satisfied with a university hospital pediatric clinic, 43.3% were fairly satisfied, and 14.9% were not satisfied. Forty-nine point four percent of respondents were satisfied with a private clinic of dermatology specialists, 39.6% were fairly satisfied, and 11.0% were not satisfied. Thirty-three point three percent of respondents were satisfied with a private clinic of pediatric specialists, 55.9% were fairly satisfied, and 10.8% were not satisfied. Thirty-eight point four percent of respondents were satisfied with an oriental herbal medicine clinic, 43.8% were fairly satisfied, and 17.8% were not satisfied (Fig. 1).
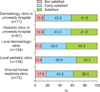
Most of the respondents considered that Western medicine had a prompt treatment effect (54.8%), followed by those who considered it to be relevant for severe or acute AD symptoms (43.4%), suitable for mild AD symptoms (35.0%), requiring a long treatment duration for an effective response (31.8%), requiring a high cost (28.8%), requiring a low cost (20.0%), not burdening the skin (20.0%), curative medicine for AD (16.6%), reducing the probability of relapse (16.0%), using reliable material (15.2%), and having no adverse effects (9.2%). Most of the respondents considered that oriental herbal medicine required a long treatment duration for an effective response (59.6%), followed by requiring a high cost (53.8%), not burdening the skin (36.2%), curative medicine for AD (31.2%), suitable for mild AD symptoms (25.4%), having no adverse effects (23.2%), reducing the probability of relapse (19.8%), using reliable material (19.4%), relevant for severe or acute AD symptoms (14.6%), having a prompt treatment effect (11.2%), and requiring a low cost (3.8%; Fig. 2).
The knowledge of patients and their parents about AD and the role of medical institutions are important for clinical outcomes and QoL. This study analyzed the knowledge of patients and their parents about treatments for AD, their treatment behaviors, and their awareness of the role of medical institutions in the treatment of AD.
Across all of the collected data, mean 52.54% of the answers were correct (range, 20.0%~90.0%) for questions about AD and its treatment, which indicates that almost half of the AD knowledge of the respondents was incorrect. The multivariate regression analysis showed that parental history of AD was independently associated with AD knowledge. AD is a chronic disease with cyclic periods of exacerbation and remission, and daily care of skin and environment is important for treatment. Patients with a parental history of AD might have indirectly learned about treatments through exposure to the daily care practices of their parents. However, patients without any previous AD experience should acquire knowledge from other sources. Previous studies15181920 have found that many patients obtained information from the Internet and trusted the source of that information, which was sometimes false. Thus, knowledge acquisition without being helped by experts may render in-depth understanding of the AD treatment by patients without any previous AD experience difficult. Enhancing the knowledge about AD treatment would encourage treatment adherence and improve patient prognoses11132122. For the improvement of the clinical outcomes of AD patients, active physician-based education programs targeting AD patients and their parents are necessary.
The most common strategy adopted by the respondents when they suspected they had AD was to visit a medical institution (43.6%). Such visits were the second most common response (293 responders) when symptoms became aggravated, after applying emollient more frequently. However, the proportion of respondents who regularly visited medical institutions for AD care was relatively low (19.8%). A chronic course of AD seems to exhaust the patients and reduce the number of patients who regularly visit a medical institution. However, similar to the case for other chronic diseases, AD should be well controlled with appropriate medical treatment; proactive treatment with long-term continuous low level topical anti-inflammatory therapy has been proposed for the prevention of atopic eczema flares23. This suggests that medical institutions should concentrate their efforts on facilitating regular follow-ups and increasing compliance among AD patients.
In our study, respondents answered that they spent an average of 519,100 KRW (approximately 433 USD) per patient annually for AD treatment. Kim et al.24 surveyed patients in 3 university hospitals for the expenditure on AD treatment. They found that the annual direct cost (including consultation fees, costs of medical tests and procedures, prescription fees, dispensing fees, medication storage fees, and the costs of drugs and other dermatologic products) per patient was 2,646,372 KRW. In this study, we conducted a web-based survey for the general population; on the other hand, Kim et al.24 surveyed patients who visited large university hospitals, and the results of their survey could be overestimated. Thus, this sampling bias may have caused this discrepancy. According to the results of a review of 418 articles on AD in the United States25, the annual direct cost per patient for AD treatment was 167~580 USD, and the total national costs of AD treatment ranged from 364 million USD to 3.8 billion USD. The national health insurance system of Korea covers a larger proportion of heath costs than does the national health insurance system of the United States. According to Organization for Economic Cooperation and Development (OECD) statistical data, not only the total payment but also the out-of-pocket payment for health care in the United States is higher than that in Korea26. Nevertheless, the high amount spent for AD treatment in Korea, similar to the amount spent in the United States, seems a burden to the Korean society. In our study, costs appeared to increase significantly with increasing disease severity. In contrast, Kim et al.24 reported that expenditure on AD treatment did not significantly increase with the disease severity. This may be attributable to the larger size of the study population (500 participants) than that in the previous study (32 participants).
Steroid phobia may cause poor compliance with AD treatment and influence the incidence rate of treatment failure15. In the present study, although most of the patients with AD and their parents (75.7%) were satisfied with steroid treatment, they tended to use steroids minimally even for aggravated symptoms. Furthermore, most of the patients and their parents were aware that a topical corticosteroid (TCS) can be addictive even after a single use (70.2%) and that long-term use of topical steroids is harmful (67.4%). Consistently, Kim et al.15 and Aubert-Wastiaux et al.27 found that TCS phobia occurred in 86.3% and 80.7% of their patients, respectively. TCSs are the representative mainstay of AD treatment27, and although they have adverse effects, their safety is well established when they are used correctly28293031. Thus, appropriate education is needed on the use of steroids for AD treatment in order to reduce steroid phobia and improve treatment adherence.
The proportion of patients who believed that Western medicine treatments are the most effective treatment for AD (26.1%) was much larger than that for oriental herbal medicine treatments (3.7%). A private clinic of dermatology specialists was the preferred medical institution (60 responders), while an oriental herbal medicine clinic was the least preferred (10 responders). Reflecting these results, the percentage of satisfied patients was highest for a private clinic of dermatology specialists and lowest for an oriental herbal medicine clinic. Several studies have found that oriental herbal medicine improves AD symptoms and is well tolerated32. However, our results showed that most patients do not appear to be satisfied with oriental herbal medicine. Consistently, Chin et al.33 reported that herbal remedies prescribed by oriental herbal medicine clinics were therapeutic in only 25.3% of the included patients, with the conditions in the others remaining unchanged or even being aggravated.
Many of our participants were aware that Western medicine has a prompt treatment effect and that it is useful for severe or acute AD symptoms, whereas oriental herbal medicine requires a longer treatment time for a cure but has the advantage of not burdening the skin. Many of the participants had used herbal medicines for a long time. However, no study has determined the therapeutic and toxicological safety profiles (to determine the risk-to-benefit ratio), which is an important aspect to consider when assessing the efficacy and tolerability of oriental herbal medicine32. This suggests that long-term oriental herbal medicine treatment for AD should be scientifically evaluated, and further study is needed to clarify its efficacy and tolerability.
This study was subject to several limitations. First, the study design did not allow face-to-face clinical visits during the questionnaire survey. Owing to the indirect administration of the questionnaire online, the study could be susceptible to nonresponse bias. However, we avoided this nonresponse bias by using a protocol designed by a survey company which was programmed to enroll respondents who fully completed the survey to participate in this study. In addition, owing to the readily accessible characteristics of the Web based survey, we could enroll a large number of respondents. Second, we used the PO-SCORAD score to measure severity. Although this is self-reported, a previous study34 demonstrated that those scores were strongly correlated with SCORAD scores, which suggests that the PO-SCORAD score provides a meaningful assessment of the disease severity of AD.
In conclusion, education programs provided by experts should be encouraged for AD patients and their parents. Patients should be educated about the importance of medical institutions not only for treating AD but also for their care and prevention. There were critical misunderstandings regarding Western medicine and oriental herbal medicine among the AD patients and their parents included in this study. To improve their treatment outcomes, efforts are needed to correct misconceptions about Western medicine and oriental herbal medicine.
Figures and Tables
 | Fig. 2Awareness of Western medicine and oriental herbal medicine for atopic dermatitis (AD) treatment. |
Table 1
Demographic characteristics of the patients and respondents (n=500)

Table 2
Predictive variables of knowledge characterized by percentages of correct answers in a multivariate linear regression model

| Variable | β estimate | 95% confidence interval | p-value | |
|---|---|---|---|---|
| Parental history of atopic dermatitis | Yes | 4.6790 | 2.6518~6.7063 | <0.0001 |
| No | Reference | Reference |
Table 3
Annual costs associated with atopic dermatitis according to age, gender, and disease severity

References
2. Ellis CN, Mancini AJ, Paller AS, Simpson EL, Eichenfield LF. Understanding and managing atopic dermatitis in adult patients. Semin Cutan Med Surg. 2012; 31:3 Suppl. S18–S22.

3. Margolis JS, Abuabara K, Bilker W, Hoffstad O, Margolis DJ. Persistence of mild to moderate atopic dermatitis. JAMA Dermatol. 2014; 150:593–600.

4. Shin JY, Kim DW, Park CW, Seo SJ, Park YL, Lee JR, et al. An educational program that contributes to improved patient and parental understanding of atopic dermatitis. Ann Dermatol. 2014; 26:66–72.

5. Annesi-Maesano I, Mourad C, Daures JP, Kalaboka S, Godard P. Time trends in prevalence and severity of childhood asthma and allergies from 1995 to 2002 in France. Allergy. 2009; 64:798–800.

6. Eichenfield LF, Hanifin JM, Beck LA, Lemanske RF Jr, Sampson HA, Weiss ST, et al. Atopic dermatitis and asthma: parallels in the evolution of treatment. Pediatrics. 2003; 111:608–616.

7. Foley P, Zuo Y, Plunkett A, Marks R. The frequency of common skin conditions in preschool-age children in Australia: atopic dermatitis. Arch Dermatol. 2001; 137:293–300.
8. Wittkowski A, Richards HL, Griffiths CE, Main CJ. The impact of psychological and clinical factors on quality of life in individuals with atopic dermatitis. J Psychosom Res. 2004; 57:195–200.

9. Sánchez-Pérez J, Daudén-Tello E, Mora AM, Lara Surinyac N. Impact of atopic dermatitis on health-related quality of life in Spanish children and adults: the PSEDA study. Actas Dermosifiliogr. 2013; 104:44–52.

10. Kemp AS. Atopic eczema: its social and financial costs. J Paediatr Child Health. 1999; 35:229–231.

11. Cork MJ, Britton J, Butler L, Young S, Murphy R, Keohane SG. Comparison of parent knowledge, therapy utilization and severity of atopic eczema before and after explanation and demonstration of topical therapies by a specialist dermatology nurse. Br J Dermatol. 2003; 149:582–589.

12. Ben-Gashir MA, Seed PT, Hay RJ. Quality of life and disease severity are correlated in children with atopic dermatitis. Br J Dermatol. 2004; 150:284–290.

13. Armstrong AW, Kim RH, Idriss NZ, Larsen LN, Lio PA. Online video improves clinical outcomes in adults with atopic dermatitis: a randomized controlled trial. J Am Acad Dermatol. 2011; 64:502–507.

14. Moore EJ, Williams A, Manias E, Varigos G, Donath S. Eczema workshops reduce severity of childhood atopic eczema. Australas J Dermatol. 2009; 50:100–106.

15. Kim JE, Lee YB, Lee JH, Kim HS, Lee KH, Park YM, et al. Disease awareness and management behavior of patients with atopic dermatitis: a questionnaire survey of 313 patients. Ann Dermatol. 2015; 27:40–47.

16. Raffin D, Giraudeau B, Samimi M, Machet L, Pourrat X, Maruani A. Corticosteroid phobia among pharmacists regarding atopic dermatitis in children: a national french survey. Acta Derm Venereol. 2016; 96:177–180.

17. van Oosterhout M, Janmohamed SR, Spierings M, Hiddinga J, de Waard-van der Spek FB, Oranje AP. Correlation between Objective SCORAD and Three-Item Severity Score used by physicians and Objective PO-SCORAD used by parents/patients in children with atopic dermatitis. Dermatology. 2015; 230:105–112.

18. Kim DH, Li K, Seo SJ, Jo SJ, Yim HW, Kim CM, et al. A survey on understanding of atopic dermatitis among Korean patients. Korean J Dermatol. 2012; 50:201–211.
19. Kwon HJ, Kim YJ, Park SB, Yu DS, Kim JW. Study of atopic dermatitis information on the internet in Korea. Korean J Dermatol. 2006; 44:137–140.
20. Yoo JH, Sohn AR. Evaluation of obesity health information internet sites in Korea. Korea Sport Res. 2004; 15:249–258.
21. Kupfer J, Gieler U, Diepgen TL, Fartasch M, Lob-Corzilius T, Ring J, et al. Structured education program improves the coping with atopic dermatitis in children and their parents-a multicenter, randomized controlled trial. J Psychosom Res. 2010; 68:353–358.

22. Ricci G, Bendandi B, Aiazzi R, Patrizi A, Masi M. Three years of Italian experience of an educational program for parents of young children affected by atopic dermatitis: improving knowledge produces lower anxiety levels in parents of children with atopic dermatitis. Pediatr Dermatol. 2009; 26:1–5.

23. Schmitt J, von Kobyletzki L, Svensson A, Apfelbacher C. Efficacy and tolerability of proactive treatment with topical corticosteroids and calcineurin inhibitors for atopic eczema: systematic review and meta-analysis of randomized controlled trials. Br J Dermatol. 2011; 164:415–428.

24. Kim C, Park KY, Ahn S, Kim DH, Li K, Kim DW, et al. Economic impact of atopic dermatitis in Korean patients. Ann Dermatol. 2015; 27:298–305.

25. Mancini AJ, Kaulback K, Chamlin SL. The socioeconomic impact of atopic dermatitis in the United States: a systematic review. Pediatr Dermatol. 2008; 25:1–6.

26. OECD. Health spending (indicator) [Internet]. OECD;2015. cited 2015 Dec 23. Available from: https://data.oecd.org/healthres/health-spending.htm.
27. Aubert-Wastiaux H, Moret L, Le Rhun A, Fontenoy AM, Nguyen JM, Leux C, et al. Topical corticosteroid phobia in atopic dermatitis: a study of its nature, origins and frequency. Br J Dermatol. 2011; 165:808–814.

28. Hoare C, Li Wan Po A, Williams H. Systematic review of treatments for atopic eczema. Health Technol Assess. 2000; 4:1–191.

29. Furue M, Terao H, Rikihisa W, Urabe K, Kinukawa N, Nose Y, et al. Clinical dose and adverse effects of topical steroids in daily management of atopic dermatitis. Br J Dermatol. 2003; 148:128–133.

30. McHenry PM, Williams HC, Bingham EA. Management of atopic eczema. Joint Workshop of the British Association of Dermatologists and the Research Unit of the Royal College of Physicians of London. BMJ. 1995; 310:843–847.
31. Berth-Jones J, Damstra RJ, Golsch S, Livden JK, Van Hooteghem O, Allegra F, et al. Twice weekly fluticasone propionate added to emollient maintenance treatment to reduce risk of relapse in atopic dermatitis: randomised, double blind, parallel group study. BMJ. 2003; 326:1367.

32. Tan HY, Zhang AL, Chen D, Xue CC, Lenon GB. Chinese herbal medicine for atopic dermatitis: a systematic review. J Am Acad Dermatol. 2013; 69:295–304.
33. Chin HW, Jang HS, Jang BS, Jo JH, Kim MB, Oh CK, et al. A study on utilization of alternative medicine for patients with atopic dermatitis. Korean J Dermatol. 2005; 43:903–911.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download