Abstract
Background
The age-dependent change in atopic dermatitis (AD) at an individual level has mostly performed in a hospital-setting.
Objective
We evaluated the age-dependent change of AD symptoms at an individual level in a community-setting.
Methods
For the diagnostic accuracy, all participants of schoolchildren were received skin examination by dermatologists (twice a year for the same group), instead of questionnaire-based surveys. For this study, sequential check-ups of 273 elementary school children, aged 7~8 years, were performed for 4 years up to the age of 10~11 years.
Results
Among the 47 AD children, who had been diagnosed as having AD at the first-year check-up, spontaneous remission was detected in nine children during the follow-up periods (remission rate of 19.1%). As a consequence, the one-year AD prevalence was decreased by 5.9% in the elementary schoolchildren over four years. Unexpectedly, late onset (after 8 years of age) AD was observed in 21.7% of AD children. There was no statistically significant relationship between spontaneous remission and host factors including sex and family history of atopic diseases.
Atopic dermatitis (AD) manifests as chronic relapsing eczema of the skin, showing a typical pattern on specific locations, depending on the patient's age. Among various instruments for AD diagnosis, the International Study of Asthma and Allergies in Childhood (ISAAC) is considered as a standard tool for cross-sectional, epidemiological surveys of childhood AD, and it has been used and validated worldwide since 1990s up till now123. AD prevalence among children is approximately 10%~20%, but AD prevalence among adults decreases later to less than 5%, indicating that many AD patients have a good prognosis and can remit spontaneously during their lives4567. Spontaneous remission of AD was reported to occur before adolescence in 40%~70% of patients with infantile AD89. In epidemiological surveys by using the ISAAC-based questionnaire, the one-year AD prevalence in childhood was reported to be 19.1% (in 2008) in Korea10.
As for the onset, AD is known to develop commonly during the very early stage of life: approximately 50% of patients develop AD before 2 years of age, and a majority of patients develop AD by 5 years of age11. On the same basis, the U.K. Working Group's criteria for AD diagnosis include one item of ‘early onset before 2 years’ among the five-item criteria1213. Recently, however, the prevalence of late onset AD is increasing worldwide, and it has been reported that almost half of patients developed AD from juvenile stage (unpublished data). These results suggest that continuous monitoring of AD prevalence in given communities or individuals is very important for efficient AD management.
Due to inherent limitations of the ISAAC as a diagnostic tool for follow-up studies at an individual level, there is no report on the age-dependent change in AD prevalence via sequential follow-up studies on childhood AD in a community setting10. Instead, the age-dependent change in AD prevalence has been reported by studying infantile AD patients who visited hospitals or were admitted to hospitals for their skin conditions, or children who were diagnosed with AD at hospitals, and not by community-based surveys891415. Hospital-visiting AD patients are known to have more severe symptoms than those detected by field surveys. In previous reports about severity of AD, 67.9%~86.1% of AD cases were mild in community-based surveys, but 32.7% of AD cases were mild in hospital-based surveys15161718. Moreover, 36% of schoolchildren with AD in a community had not consulted their doctors, probably because the disease was mild18. Therefore, the generalization of results from hospital-based surveys to the whole population in a given community contains a high probability to cause selection bias.
With this background, this study aimed to evaluate the age-dependent change in AD prevalence among children in the age range of 7~8 years at an individual level. In this study of a community-setting, skin examination by dermatologists, instead of questionnaire-based survey, for AD diagnosis was used.
Children aged 7 to 8 years in 2011 who were in the elementary school of Gwangju, Korea were recruited. A total of 305 children were included, and they were followed up at twice a year (June and December). Both skin examination by dermatologists was performed prospectively for 4 years. From 2011 to 2014, 32 children dropped out, and a total of 273 children were followed up (Fig. 1). In 2011, the number of children who were 7 years and 8 years of age was 119 and 154, respectively. There were 146 boys (53.5%), and 127 girls (46.5%). The study was approved by Chonnam National University Hospital Institutional Review Board (IRB no. CNUH-2012-099) and conducted according to the ethical guidelines of the Declaration of Helsinki.
One-time skin examination is likely to exclude mild or transient AD cases, in which many AD children with mild symptoms showed a temporary remission for certain time periods in a year19. Therefore, as a gold standard for AD diagnosis, skin examination by dermatologists should be performed twice a year at least in the same group of children. Two dermatologists visited the elementary school for skin examination. Considering that there are two seasons (summer and winter) in which AD symptoms can be aggravated in Korean AD children (unpublished data), we performed the 1st skin examinations in June. Based on the results of the skin examination, children were classified into one of the three groups; ‘AD’, ‘non-AD’, and ‘undetermined’. In December, the 2nd skin examination was performed in children, who were classified as ‘non-AD’ and ‘undetermined’ on the 1st skin examination. When AD was diagnosed at least once in June or December, it was defined as presenting AD during that year. The severity of AD was graded as mild, moderate, or severe according to the following criteria: (1) mild, skin involvement by mild eruption only; (2) moderate, <10% surface area involvement by severe eruption; (3) severe, >10% of body involvement by severe eruption18.
Decision between the ‘spontaneous remission’ group and the ‘intermittent or persistent’ group was taken in 47 children who were diagnosed with AD in 2011. We defined ‘spontaneous remission’ in AD children who were disease free for 3 years continuously: skin lesions were not detected on skin examinations by dermatologists, twice a year. If children did not satisfy the above requirements, they were classified into the intermittent or persistent group.
Pearson's chi-squared test was used for analyzing the factors associated with remission of AD. The factors included age, aggravation due to food, and family history of asthma, allergic rhinitis, allergic conjunctivitis, AD, and atopic diseases. Atopic diseases were classified as diseases including asthma, allergic rhinitis, allergic conjunctivitis, and AD. IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA) was used to analyze the data, with p-values of <0.05 being considered statistically significant.
Of the 47 children who were diagnosed with AD in 2011, nine patients (19.1%) showed spontaneous remission, and 38 patients (80.9%) had intermittent or persistent symptoms during the 4 years follow-up period. Two hundred thirteen children who did not show any symptoms during the follow-up period were classified into the non-AD group (Fig. 1).
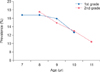
A total 5.9% decrease in AD prevalence was observed during the 4 years follow-up period. The annual change in prevalence among first graders was 16.8% (7 years of age), 16.8% (8 years of age), 15.9% (9 years of age), and 12.6% (10 years of age). The annual change in prevalence among second graders was 17.5% (8 years of age), 14.9% (9 years of age), 13% (10 years of age), and 10.4% (11 years of age) (Fig. 2).
Additional questionnaire-based surveys on the onset age and aggravating factors were performed for children who were diagnosed as AD by skin examination. The onset age was ≤1 year in 24 patients (40%), 2~3 years in 19 patients (31.7%), and ≥4 years in 17 patients (28.3%). Thirteen children (21.7% of AD patients) had AD after 8 years of age, or were diagnosed with AD on skin examination during our study (Fig. 3). The severity of AD was mild in 33 out of the 47 AD patients (70.2%), moderate in 13 AD patients (27.7%), and severe in 1 AD patient (2.1%) in 2011 (Table 1).
Forty-seven children, who were diagnosed as having AD in 2011, were classified into the ‘spontaneous remission’ group and the ‘intermittent or persistent’ group. Family history of atopic diseases, which include asthma, allergic rhinitis, allergic conjunctivitis, and AD, was positive in 38 patients (80.9%). Sex, family history of asthma, allergic rhinitis, allergic conjunctivitis, AD, and atopic diseases did not show a statistically significant difference between the ‘spontaneous remission’ group and the ‘intermittent or persistent’ group (Pearson's chi-squared test, p>0.05) (Table 2).
AD is a common inflammatory skin disease in childhood, often manifesting in early infancy and has a natural course that varies over time. One of misconceptions among parents of children with AD is that AD is a life-long persistent disease, although this is true only in a small number of patients14. Lack of information about the natural course causes anxiety, and leads to the use of an unscientific approach and untested regimens. Because the natural course of AD varies among individuals, studies on its natural course in different age groups and races are important. However, because only few prospective studies exist, the natural course of AD is not completely known. Most epidemiologic studies of AD are cross-sectional studies showing point prevalence, and it is difficult to understand the natural course of AD2021. Previous studies have been flawed because only the patients with infantile AD in a hospital setting are considered1122. The results do not reflect the other age groups of AD except for infantile AD. Furthermore, there is a large difference in severity between patients in a hospital setting and those in a community setting. The proportion of patients with severe AD in a hospital setting is higher than that of patients with severe AD in a community setting23. The previous study in Koreans has a limitation in terms of its retrospective nature, and it was performed by reviewing the medical records and parents' telephone interview14.
In previous studies, about 70% of infantile AD cases went into spontaneous remission91415. In a population-based cohort study from Taiwan, spontaneous remission occurred in 69.8% of the 1,404 early-onset AD patients (onset in the first 2 years) during the 10-year follow-up period9. In a study, which was performed for 5 years in children in the age group of 1~3 years , 52% showed spontaneous remission24. In a study, which was performed in children in the age group of 9~11 years until they were 16 to 20 years old, 6.1% showed spontaneous remission25. In previous studies, the spontaneous remission rate was decreased significantly with aging. In this study, children in the age group of 7~8 years were followed up prospectively until they were 10~11 years old, and spontaneous remission was detected in 19.1% of patients. This result reflects the natural course of childhood AD in 7 to 11 years old children who had not been included in previous studies.
In a previous sequential study on AD prevalence in the same group (19% in the 0 to 1 year age group, 14% in the 1 to 2 years age group, and 5% in the 6 to 7 years age group), spontaneous remission of AD was commonly observed in the early stage AD patients9. In this study, we found that the change of AD prevalence in children of the 7~8 years age group (0.9%~3.3% decrease every year) was markedly lower in comparison with that in children of the 0~1 year age group9. These results reflect the importance of surveys in children of different age groups in relation with spontaneous remission of AD in the future.
Due to the difference in the population, the factors associated spontaneous remission of AD were inconsistent with those in previous studies9152224. One study in Europe showed that the course of AD is significantly related to egg sensitivity, and the average healing time is higher in egg-sensitive patients15. The other study showed that independent factors at baseline predicting remission were milder type, later onset, non-flexural area, no food allergy, and rural living24. However, a population-based cohort study from Taiwan in 1,404 AD patients showed that sex, onset age, presence of allergic rhinitis, presence of asthma, and presence of respiratory atopy (either allergic rhinitis or asthma) did not have a statistically significant influence on disease course9. A meta-analysis study about the factors predicting complete remission showed that parental allergy and sex did not predict the remission of infant-onset AD until the age of 6~7 years22. A retrospective study in Korean AD patients showed that none of the risk factors were significant by multivariate analysis, but maternal diet restriction during lactation and no sensitization to cow's milk were significantly associated with remission of AD in the moderate-to-severe AD group14. In this study, sex, family history of asthma, allergic rhinitis, allergic conjunctivitis, and AD did not show a statistically difference between the spontaneous remission group and the intermittent or persistent group. This result was in accordance with the previous reports91422, which did not show any factors associated with remission when the population had a high proportion of mild AD cases.
Most of the AD patients are diagnosed before childhood especially in the first year of life2627. One questionnaire-based survey of 7~8 years old Korean children reported the following findings: onset age: <2 years in 43.7% and ≥5 years in 26% of children21. However, the prevalence of late-onset AD or relapsing AD that shows re-occurrence of AD symptoms after pubertal age is increasing worldwide. Almost half of the patients developed AD from the juvenile stage; juvenile stage (10%), early adult stage (13%), late adult stage (20%), and senile stage (1%~3%) (unpublished data). The onset age was found to be 10% in <2 years old children, 28.3% in ≥5 years old children, and 21.7% in >8 years old children, showing an increase in the prevalence of late-onset AD. These patients were diagnosed with AD by skin examination performed by dermatologists which might be more precise than the questionnaire survey.
This study has several advantages over previous studies. Firstly, our prospective study was performed for four years. For reducing the error in AD diagnosis, skin examinations were performed twice every year (June and December) by dermatologists. Secondly, the age-group for this study was 7~11 years and this age group had not been studied in previous reports. Thirdly, our study was a community-based survey that more precisely reflected the course of mild AD (70% of total AD children) in a population-based setting. However, this study has limitation, because it was done in small population (n=305). Further studies are required to unravel the true prognosis of childhood AD in Korea by a large-population-based survey for longer follow-up periods. The recall bias could be in this study, because the questionnaire survey was done for aggravation factors of AD.
This study was a community-based follow-up study about the natural course of childhood AD (7 to 11 years of age) in Gwangju province, Korea. The population was selected from a community, not from a hospital, and the study was performed prospectively. We found that 19.1% of AD patients showed spontaneous remission, and 80.9% of AD patients had intermittent or persistent symptoms during the 4 years follow-up period. A total decrease of 5.9% in the AD prevalence was noted in the 4 years follow-up period. Also, 21.7% of patients developed AD after 8 years of age or were diagnosed by skin examination during our study. Sex, family history of asthma, allergic rhinitis, allergic conjunctivitis, AD, and atopic diseases did not show a statistically difference between the spontaneous remission and intermittent or persistent groups.
Figures and Tables
Fig. 3
Natural course of disease within 4 years followed up period in 60 children with atopic dermatitis. Each square represents a one children's natural course. Squares in color represent that symptoms of atopic dermatitis were present.

Table 1
Severity of atopic dermatitis
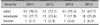
| Severity | 2011 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| Mild | 33 (70.2) | 31 (72.1) | 31 (79.5) | 21 (67.7) |
| Moderate | 13 (27.7) | 11 (25.6) | 7 (17.9) | 8 (25.8) |
| Severe | 1 (2.1) | 1 (2.3) | 1 (2.6) | 2 (6.5) |
Table 2
Factors associated with spontaneous remission of atopic dermatitis

References
1. Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995; 8:483–491.

2. Weiland SK, Björkstén B, Brunekreef B, Cookson WO, von Mutius E, Strachan DP, et al. Phase II of the International Study of Asthma and Allergies in Childhood (ISAAC II): rationale and methods. Eur Respir J. 2004; 24:406–412.

3. Ellwood P, Asher MI, Beasley R, Clayton TO, Stewart AW. ISAAC Steering Committee. The international study of asthma and allergies in childhood (ISAAC): phase three rationale and methods. Int J Tuberc Lung Dis. 2005; 9:10–16.
4. Mortz CG, Lauritsen JM, Bindslev-Jensen C, Andersen KE. Prevalence of atopic dermatitis, asthma, allergic rhinitis, and hand and contact dermatitis in adolescents. The odense adolescence cohort study on atopic diseases and dermatitis. Br J Dermatol. 2001; 144:523–532.

5. Tay YK, Kong KH, Khoo L, Goh CL, Giam YC. The prevalence and descriptive epidemiology of atopic dermatitis in Singapore school children. Br J Dermatol. 2002; 146:101–106.

6. Eller E, Kjaer HF, Høst A, Andersen KE, Bindslev-Jensen C. Development of atopic dermatitis in the DARC birth cohort. Pediatr Allergy Immunol. 2010; 21:307–314.

8. Illi S, von Mutius E, Lau S, Nickel R, Grüber C, Niggemann B, et al. The natural course of atopic dermatitis from birth to age 7 years and the association with asthma. J Allergy Clin Immunol. 2004; 113:925–931.

9. Hua TC, Hwang CY, Chen YJ, Chu SY, Chen CC, Lee DD, et al. The natural course of early-onset atopic dermatitis in Taiwan: a population-based cohort study. Br J Dermatol. 2014; 170:130–135.

10. Choi WJ, Ko JY, Kim JW, Lee KH, Park CW, Kim KH, et al. Prevalence and risk factors for atopic dermatitis: a crosssectional study of 6,453 Korean preschool children. Acta Derm Venereol. 2012; 92:467–471.

11. Hwang CY, Chen YJ, Lin MW, Chen TJ, Chu SY, Chen CC, et al. Prevalence of atopic dermatitis, allergic rhinitis and asthma in Taiwan: a national study 2000 to 2007. Acta Derm Venereol. 2010; 90:589–594.

12. Williams HC, Burney PG, Pembroke AC, Hay RJ. The U.K. working party's diagnostic criteria for atopic dermatitis. III. Independent hospital validation. Br J Dermatol. 1994; 131:406–416.

13. Williams HC, Burney PG, Pembroke AC, Hay RJ. Validation of the U.K. diagnostic criteria for atopic dermatitis in a population setting. U.K. diagnostic criteria for atopic dermatitis working party. Br J Dermatol. 1996; 135:12–17.

14. Chung Y, Kwon JH, Kim J, Han Y, Lee SI, Ahn K. Retrospective analysis of the natural history of atopic dermatitis occurring in the first year of life in Korean children. J Korean Med Sci. 2012; 27:723–728.

15. Ricci G, Patrizi A, Baldi E, Menna G, Tabanelli M, Masi M. Long-term follow-up of atopic dermatitis: retrospective analysis of related risk factors and association with concomitant allergic diseases. J Am Acad Dermatol. 2006; 55:765–771.

16. Kim DS, Lee JH, Lee KH, Lee MG. Prevalence and severity of atopic dermatitis in Jeju Island: a cross-sectional study of 4,028 Korean elementary schoolchildren by physical examination utilizing the three-item severity score. Acta Derm Venereol. 2012; 92:472–474.

17. Marks R, Kilkenny M, Plunkett A, Merlin K. The prevalence of common skin conditions in Australian school students: 2. Atopic dermatitis. Br J Dermatol. 1999; 140:468–473.

18. Saeki H, Iizuka H, Mori Y, Akasaka T, Takagi H, Kitajima Y, et al. Prevalence of atopic dermatitis in Japanese elementary schoolchildren. Br J Dermatol. 2005; 152:110–114.

19. De D, Kanwar AJ, Handa S. Comparative efficacy of Hanifin and Rajka's criteria and the UK working party's diagnostic criteria in diagnosis of atopic dermatitis in a hospital setting in North India. J Eur Acad Dermatol Venereol. 2006; 20:853–859.

20. Park YL, Kim HD, Kim KH, Kim MN, Kim JW, Ro YS, et al. Report from ADRG: a study on the diagnostic criteria of Korean atopic dermatitis. Korean J Dermatol. 2006; 44:659–663.
21. Flohr C, Weinmayr G, Weiland SK, Addo-Yobo E, Annesi-Maesano I, Björkstén B, et al. How well do questionnaires perform compared with physical examination in detecting flexural eczema? Findings from the International Study of Asthma and Allergies in Childhood (ISAAC) phase two. Br J Dermatol. 2009; 161:846–853.

22. Lee HY, Lee JR, Roh JY. Epidemiological features of preschool childhood atopic dermatitis in Incheon. Korean J Dermatol. 2009; 47:164–171.
23. Lee DJ, Kim EH, Jang YH, Lee ES. Epidemiological features of childhood atopic dermatitis in Suwon. Korean J Dermatol. 2010; 48:482–493.
24. von Kobyletzki L, Svensson Å, Apfelbacher C, Schmitt J. Factors that predict remission of infant atopic dermatitis: a systematic review. Acta Derm Venereol. 2015; 95:389–394.

25. Takeuchi S, Esaki H, Furue M. Epidemiology of atopic dermatitis in Japan. J Dermatol. 2014; 41:200–204.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download