Dear Editor:
Fibro-osseous pseudotumor of the digit (FOPD) is a rare, biphasic ossifying tumor in young patient, characterized by osteoid formation and fibroblastic proliferation1. There are some tumors showing heterotopic ossification: myositis ossificans (MO), ossifying plexiform tumor2, acral angioosteoma cutis3 and extraskeletal osteosarcoma (EO). However, if it developed in an old-aged patient with cellular atypism, physician has to consider an overdiagnosis of EO to prevent from unnecessary amputation of the digit4. Herein, we report a patient with FOPD that can lead to the mistaken diagnosis of EO and others.
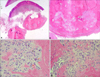
A 68-year-old male patient presented to the clinic with a tender, hard, half dome-shaped subcutaneous mass on the palmar side of left thumb (Fig. 1). The mass was 0.9 cm in diameter and had a duration of 3 months. There has been no history of trauma and infection. Also, he is a right-handed person. Other medical history is diabetic mellitus for about a decade. We took an incisional biopsy from the lesion and removed it totally. Histologically, at low power view, there are compact hyperkeratosis, epidermal hyperplasia and fusion of rete ridge in the epidermis. This mass shows no connection to the epidermis and bony structure (Fig. 2A). Moreover, irregular shaped osteoid formation surrounded by fibrotic band is observed with trabecular margin and calcified foci in subcutis layer (Fig. 2B). At high power field, osteoblast and multi-nucleated osteoclast are seen around osteoid portion. And a few of mitotic cells were detected (Fig. 2C). Biphasic immature pattern of spindle cellular portion and bony portion were shown chaotically at the same field. Also red blood cells extravasate from the capillary vessels. A part of cells has an irregular size, morphology and atypical nucleus (Fig. 2D). But we can exclude EO despite of these atypical features. Because overall cellular atypism is not severe and cellular density is not as high as in EO. After then, the patient stayed well without recurrence during follow-up for 6 months.
The most confoundable diagnosis would be a MO. Also, some author asserts that FOPD could be a superficial and distal variant of MO5. But, MO usually has a history of trauma, occurs on the deeper aspect of proximal soft tissue, and histopathologically shows a typical zoning phenomenon1. And ossifying plexiforn tumor may be clinically similar to FOPD in its propensity to develop on a distal finger. But the plexiform pattern of fibroblastic proliferation and osteoid formation is different from FOPD2. Also acral angioosteoma cutis can looks like FOPD given the ossification of acral soft tissue. But this tumor obviously has a portion of dilated capillary network3. Above all, the most important differential diagnosis is EO to avoid aggressive surgery4, especially when it accompany with a history of short duration, painful symptom and old age patient. So it is histologically essential to find and check malignant cells with pleomorphism.
In conclusion, FOPD is a rare ossifying tumor which can lead a mistaken diagnosis of EO. Our case emphasizes the need to detect these differential diagnoses in patients with tumor occurring on the digit with ossification.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download