Abstract
Background
Psoriasis is associated with increased risk of cardiovascular morbidities, especially in severe cases. Severity of the disease has been known to be associated with higher prevalence of these risk factors. However, in the absence of robust measurements, studies to date relied mostly on treatment spectrum as a proxy for the severity.
Objective
To evaluate the relationship between psoriasis area and severity index (PASI) and cardiovascular risk factors in Korean patients.
Methods
Presence of diabetes mellitus (DM), hypertension, smoking history was surveyed through questionnaires and serum lipid profile analysis were done after fasting overnight. The severity of psoriasis was assessed using PASI scores: mild, <10; moderate to severe, ≥10. Cardiovascular risk factors such as smoking, hypertension, diabetes and dyslipidemia were compared between the mild group and moderate to severe group. The prevalence of diabetes and hypertension was compared among these two groups of psoriasis patients and the general population based control; age and gender were matched among three groups accordingly prior to analysis.
Results
A total of 256 patients with plaque type psoriasis were included. Between mild group and moderate to severe group, significant differences of cardiovascular risk factors including lipid profile were not discovered except in triglyceride level. Comparing to general population, prevalence of diabetes was found significantly higher in psoriasis patients while that of hypertension was similar.
Although cardiovascular risk in patients with mild psoriasis may be relatively small, it increases with severity of disease1. However, in the absence of robust measurements, studies to date relied mostly on treatment spectrum as a proxy for disease severity. Usually, the subjects were defined as having moderate to severe psoriasis if they had a history of systemic treatments. However, some psoriasis therapies may increase incidence of cardiovascular diseases while others may decrease it12. These heterogenous effects of individual drugs on cardiovascular disease may limit current practice of determining the severity according to past treatment history, in the aspect of evaluating the current cardiovascular risk factors. Then we used psoriasis area and severity index (PASI) which is widely used to measure severity in both research and clinical setting as a severity index. To date, few studies which determine the relationship between cardiovascular risk factors and PASI have been published and the relationship has not been clearly demonstrated in Asian psoriasis patients.
In this study, we included psoriasis patients aged >18 years who visited the Department of Dermatology at the Hallym University Sacred Heart Hospital from October 2013 to January 2015. While small and large plaque-type psoriasis patients were included in this study, other types such as guttate-type, erythrodermic, generalized pustular psoriasis, and palmoplantar psoriasis were excluded. The study protocol was approved by Institutional Review Board/Ethics Committee of Hallym University Sacred Heart Hospital (IRB No. 2015-I126).
The presence of diabetes mellitus (DM), hypertension, smoking history were surveyed through questionnaires. Smoking status was defined as whether the subjects have smoked any cigarettes in the past one month. Weight and height were checked and body mass index (BMI) was calculated as weight (kg)/height (m)2. Severity of psoriasis was assessed by one physician using PASI score. Within 1 week of evaluating PASI, serum lipid profile analysis was done; the level of triglyceride, total cholesterol, high-density lipoprotein (HDL)-cholesterol (HDL-C) and low-density lipoprotein (LDL)-cholesterol (LDL-C) were investigated. Blood samples were taken after the subjects had fasted overnight.
The subjects with PASI score lower than 10 were defined having mild psoriasis, and score 10 or higher moderate to severe psoriasis. Cardiovascular risk factors such as smoking, hypertension, diabetes and dyslipidemia were compared between the mild group and moderate to severe group. We used the Korea Health Statistics 20133 as general population based control and compared the prevalence of diabetes and hypertension after matching age and gender with two psoriasis patients group—moderate to severe and mild.
Chi-square test was used to compare categorical parameters between the groups, while t-test was used to compare continuous parameters. All the statistical analysis were performed using SPSS (Windows version 13.0; SPSS Inc., Chicago, IL, USA). The p-value<0.05 was considered statistically significant.
A total of 256 patients with plaque type psoriasis were included in this study (Table 1). In the patient group with mild psoriasis, there were 73 men and 62 women. In the psoriasis group with moderate to severe degree, there were 69 men and 52 women. There was no statistically significant difference in the gender between the groups (p=0.635). The mean age of the mild psoriasis patients group was 40.30±13.32 years and that of the moderate to severe psoriasis patients group was 42.96±11.44 years. There was no significant difference in the mean age (p=0.242).
There was no significant difference in smoking status or BMI between the mild group and the moderate to severe group (p=0.807 and 0.394, respectively). The prevalences of hypertension and DM were not significantly different (p=0.165 and 0.844, respectively) between two groups. Concerning the lipid profile, the triglyceride levels in the moderate to severe group were significantly higher than those in the mild group (p=0.047). The triglyceride levels in both mild group and moderate to severe group was analyzed by correlation coefficient test, and the results were 0.143 (p=0.098), 0.248 (p=0.006, <0.01). Both values showed positive correlation, and statistical significance was only observed in moderate to severe group. Among the other lipid profiles such as total cholesterol, HDL-C, LDL-C, there was no significant intergroup (p=0.152, 0.877 and 0.555, respectively) (Table 2). Compared with data from Korean Health Statistics3, diabetes showed significantly higher prevalence while hypertension showed insignificant results (Table 3)—however, severity of psoriasis did not correlate with the prevalence of both diseases, as prevalence of DM was significantly higher in mild psoriasis group (p=0.033).
The recent literature has focused on linking psoriasis severity with an increase in comorbidity risk, a risk evident even with mild psoriasis compared with controls4. Through meta-analysis, it was found that patients with severe psoriasis may have an even higher risk of developing diabetes5. In addition, ischemic heart disease and cardiovascular risk factors were associated with psoriasis in hospitalized patients, who were hypothesized to be severe psoriasis patients6. It has been also speculated that the more severe psoriasis is, the greater the incidence of metabolic syndrome7. In Korean studies, there were conflicting results in respect of incidence of metabolic syndrome. Kim et al.8 reported that there was no significant difference in prevalence of metabolic syndrome in regard to the body surface area, well known risk factor for severe psoriasis. In the contrary, Choi et al.9 showed the risk of metabolic syndrome was associated with the severity of psoriasis determined by whether history of systemic treatments exist or not.
To our knowledge, there were only few reports which analyzed how cardiovascular comorbidities were affected by PASI. In a Canadian study consisting of psoriatic arthritis patients, risk of hypertension correlated positively with high PASI score, and the risk of myocardial infarction was proven to be more prominent in the group with PASI score greater than 2010. Also, it was reported Framingham risk score, one of the widely used cardiovascular risk score estimation system, showed the significant correlation with PASI, but not with body surface area, characteristics of treatment, duration of psoriasis in a Spanish study11. On the other hand, there was no difference in the prevalence of metabolic syndrome between patients with PASI score lower and higher than 10 in an Italian study12.
To assess the severity of psoriasis for determining the relationship to cardiovascular risk factors, we concluded classifying severity based on the medication history was inappropriate, because the opinions of the patients may affect treatment intensity or schedule, and systemic medications itself may influence cardiovascular risk factors. It is well known that systemic psoriasis therapies affect the risk of cardiovascular disease. Acitretin can increase serum triglycerides and cholesterol, specifically by shifting high-density lipoproteins to low-density lipoproteins. Cyclosporine can increase blood pressure, serum triglycerides, and total cholesterol. On the other hand, methotrexate and tumor necrosis factor inhibitors may reduce the risk of cardiovascular disease morbidity1. Psoriasis treatments work by anti-inflammatory mechanism and thus it could be hypothesized that decrease of inflammation with psoriasis treatments may lead to improvement of cardiovascular risk2.
In the present study, significant differences of cardiovascular risk factors and lipid profile according to the severity of the psoriasis were not discovered except in triglyceride level. Prevalence of DM was shown to be higher in psoriasis groups as a whole compared to control group, but between in regard to severity the mild group had more DM patients than the moderate-and-severe group with significant results. In previous studies813, it was described that only triglyceride level exhibited significant difference between psoriasis and control subjects among lipid profile; HDL, LDL, and total cholesterol were not subject to same conclusion. The reason why the only triglyceride level resulted in this abnormality remains unclear. We think that careful attention must be paid to dyslipidemia—hypertriglyceridemia in particular—in psoriasis patients, especially if the degree of psoriasis is moderate to severe. Similar lipid profile between both groups—again excluding triglyceride level—might be due to inadequate sample size or other circumstance such as administration of antihypertensive or antidiabetic agent, as these are known to affect lipid metabolism in various ways; antihypertensive medication such as β-blocker or thiazide diuretics are known to have deleterious effect to lipid metabolism, while calcium channel blockers and angiotensin-converting enzyme inhibitors are found to have favorable effect14.
Thiazolidinediones can cause an elevation in HDL and variable increase in LDL, while metformin and insulin have favorable effects by decreasing triglycerides and raising HDL15. Triglyceride levels and the coefficient of both group were respectively 0.143 (p=0.098), 0.248 (p=0.006), which showed positive correlation, and significance was observed in moderate to severe group. This is supposedly because the more severe psoriasis is, the more patient went through systemic therapy and, oral medications such as acitretin, cyclosporine could have increased serum triglyceride level. As the sample size was relatively small, further study with bigger sample size is needed.
After matching age and gender, incidences of hypertension in psoriasis patients group in our study were not significantly higher than control group, and that of hypertension and DM showed inverse correlation with severity of the disease—in addition, the result of DM was significant. Because we analyzed the presence of these diseases only through questionnaire survey, it is possible some cases were unnoticed, causing underestimation of the prevalence among subjects. Relatively small sample size may have contributed the confounding of results, too. These limitation of our study mentioned above calls for further investigation to elucidate the exact nature of association. Larger study such as nationwide studies are needed to prove or disprove the association between the severity of psoriasis and cardiovascular risk factors in Korean psoriasis patients.
Figures and Tables
Table 1
Comparisons of dermographic data according to the psoriasis area severity index (PASI) in psoriasis patients
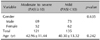
| Variable | Moderate to severe (PASI≥10) | Mild (PASI<10) | p-value |
|---|---|---|---|
| Gender | 0.635 | ||
| Male | 69 | 73 | |
| Female | 52 | 62 | |
| Total | 121 | 135 | |
| Age (yr) | 42.96±11.44 | 40.30±13.32 | 0.242 |
Table 2
Comparisons of cardiovascular risk factor according to the psoriasis area severity index (PASI) in psoriasis patients

References
1. Hugh J, Van Voorhees AS, Nijhawan RI, Bagel J, Lebwohl M, Blauvelt A, et al. From the Medical Board of the National Psoriasis Foundation: the risk of cardiovascular disease in individuals with psoriasis and the potential impact of current therapies. J Am Acad Dermatol. 2014; 70:168–177.

2. Churton S, Brown L, Shin TM, Korman NJ. Does treatment of psoriasis reduce the risk of cardiovascular disease? Drugs. 2014; 74:169–182.

3. Korea Centers for Disease Control and Prevention. The Sixth Korea National Health and Nutrition Examination Survey (KNHANES VI-1), 2013. Cheongju: Korea Centers for Disease Control and Prevention;2013.
4. Shlyankevich J, Mehta NN, Krueger JG, Strober B, Gudjonsson JE, Qureshi AA, et al. Accumulating evidence for the association and shared pathogenic mechanisms between psoriasis and cardiovascular-related comorbidities. Am J Med. 2014; 127:1148–1153.

5. Armstrong AW, Harskamp CT, Armstrong EJ. Psoriasis and the risk of diabetes mellitus: a systematic review and meta-analysis. JAMA Dermatol. 2013; 149:84–91.
6. Miller IM, Ellervik C, Yazdanyar S, Jemec GB. Meta-analysis of psoriasis, cardiovascular disease, and associated risk factors. J Am Acad Dermatol. 2013; 69:1014–1024.

7. Armstrong AW, Harskamp CT, Armstrong EJ. Psoriasis and metabolic syndrome: a systematic review and meta-analysis of observational studies. J Am Acad Dermatol. 2013; 68:654–662.

8. Kim GW, Park HJ, Kim HS, Kim SH, Ko HC, Kim BS, et al. Analysis of cardiovascular risk factors and metabolic syndrome in Korean patients with psoriasis. Ann Dermatol. 2012; 24:11–15.

9. Choi WJ, Park EJ, Kwon IH, Kim KH, Kim KJ. Association between psoriasis and cardiovascular risk factors in Korean patients. Ann Dermatol. 2010; 22:300–306.

10. Gladman DD, Ang M, Su L, Tom BD, Schentag CT, Farewell VT. Cardiovascular morbidity in psoriatic arthritis. Ann Rheum Dis. 2009; 68:1131–1135.

11. Fernández-Torres R, Pita-Fernández S, Fonseca E. Psoriasis and cardiovascular risk. Assessment by different cardiovascular risk scores. J Eur Acad Dermatol Venereol. 2013; 27:1566–1570.

12. Gisondi P, Tessari G, Conti A, Piaserico S, Schianchi S, Peserico A, et al. Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study. Br J Dermatol. 2007; 157:68–73.

13. Gyldenløve M, Storgaard H, Holst JJ, Vilsbøll T, Knop FK, Skov L. Patients with psoriasis are insulin resistant. J Am Acad Dermatol. 2015; 72:599–605.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download