Abstract
Background
The atopic dermatitis (AD) can limit a patient's physical and psychosocial development as well as lower their overall quality of life (QOL), including sleep quality.
Objective
The purpose of this study was to evaluate the relationships between clinical disease severity, QOL and sleep quality in children and adults with AD.
Methods
The SCORing atopic dermatitis (SCORAD) was examined to evaluate the severity of AD in fifty adult AD patients and 50 children AD patients. A questionnaire based on the children's sleep habits questionnaire (CSHQ) and the children's dermatology life quality index (CDLQI) were used to evaluate QOL and sleep disturbance in children AD patients. The Pittsburgh sleep quality index (PSQI) and dermatology life quality index (DLQI) were used in adult AD patients.
Results
The SCORAD and CSHQ score, the SCORAD and CDLQI score and the CSHQ and CDLQI score demonstrated significant correlations. The SCORAD and PSQI score showed no significant correlation. However, there were significant correlations between the SCORAD and DLQI score and the PSQI and DLQI score.
Conclusion
Increasing severity of AD affects sleep quality in child AD patients. In adults, even though the total score of the sleep questionnaire is not associated with the severity of AD, two components of sleep questionnaire are associated with the severity of AD. There is a significant correlation between sleep quality and QOL in both children and adults. Therefore, we suggest that evaluating the sleep quality as well as clinical severity of the disease is necessary in the management of AD patients.
Atopic dermatitis (AD) is a chronic inflammatory skin disease characterized by pruritic, dryness and eczematous lesions1. In recent years, many studies have shown higher rates of AD prevalence ranging from 17% in children and 2% to 3% in adults2. The chronic and recurrent nature of AD, combined with the absence of a curative treatment, negatively impact the quality of life (QOL) of the patient. The symptoms of AD can limit a patient's physical and psychosocial development as well as lower their overall QOL, including sleep quality1. Sleep disturbances may have considerable effects on both child and adult patients23 they can result in significant daytime deficits including fatigue, mood disorder, and poor behavioral functioning as well as developmental disorders in children1. Despite the high prevalence of sleep disturbance in AD patients, only a few studies have evaluated the sleep quality in AD patients.
The purpose of this study was to identify the correlation between clinical disease severity, sleep quality and QOL in children and adults with AD. We also analyzed the relationship between disease severity and the components of a sleep questionnaire.
This study included 50 children AD patients (30 boys and 20 girls) and 50 adult AD patients (22 men and 28 women) who visited the Department of Dermatology at Eulji Medical Center between January 2014 and September 2014. All patients fulfilled the diagnostic criteria of Hanifin and Rajka. The patients' mean age was 4.9±3.23 years for the child AD patients and 26.4±9.56 years for the adult AD patients. The exclusion criteria included any congenital disorders, any other chronic disorders and any neuropsychiatric disorders that could cause sleep disorders. This study was approved by the Ethics Committee of Eulji Medical Center (IRB No. 2014-02-003).
A trained dermatologist used the SCORing atopic dermatitis (SCORAD) index, including objective index scores (extent and intensity; ranging from 0 to 118 points) and subjective index scores (pruritus and sleep loss; ranging from 0 to 20 points), to evaluate the severity of AD in all patients4. The severity groups were defined as follows: SCORAD scores <20 (mild AD group), 20~40 (moderate AD group), and ≥40 (severe AD group). A questionnaire based on the children's sleep habits questionnaire (CSHQ) and the children's dermatology life quality index (CDLQI) were used to determine sleep quality and QOL in child patients56. The CSHQ (ranging from 6 to 83 points) is a retrospective, 35-item parent questionnaire that has eight components reflecting the following sleep domains in children: 1) bedtime resistance, 2) sleep onset delay, 3) sleep duration, 4) sleep anxiety, 5) night waking, 6) parasomnias, 7) sleep disordered breathing, and 8) daytime sleepiness. A higher CSHQ score is indicative of more disturbed sleep. It appears to be a useful sleep screening instrument to delineate sleep habits and identify problematic sleep components in children. The CDLQI (ranging from 0 to 30 points) is a children's version of the dermatology life quality index (DLQI), which was developed as a tool to facilitate a QOL assessment of children with skin conditions. It is self-explanatory and can be simply handed to the patient who is asked to fill it in with the help of a parent or guardian.
In adult AD patients, we used the Pittsburgh sleep quality index (PSQI) and DLQI78. The PSQI (ranging from 0 to 21 points) is composed of seven components that evaluate the quality of sleep in adults: 1) subjective sleep quality, 2) sleep latency, 3) sleep duration, 4) habitual sleep efficiency, 5) sleep disturbance, 6) use of sleeping medication, and 7) daytime dysfunction. A higher PSQI score is indicative of more disturbed sleep. It is an effective instrument used to measure the quality and patterns of sleep in adults. The DLQI (ranging from 0 to 30 points) is a simple 10-question validated questionnaire that is a self-administered and efficient instrument for assessing QOL in dermatology patients. The higher the DLQI score, the more QOL is impaired.
Statistical analysis was performed with SPSS ver. 12.0 for Windows Statistical Package (SPSS Inc., Chicago, IL, USA). The Pearson's correlation coefficient was used to observe the correlations among SCORAD score, the CSHQ/PSQI scores and the CDLQI/DLQI scores. The differences were considered to be significant when the p-value was less than 0.05.
All questionnaire mean results are shown in Table 1. The mean scores of the CSHQ, SCORAD and CDLQI in child AD patients (n=50) were 42.67±6.32, 26.76±10.91 and 9.31±5.16, respectively. The mean score of the PSQI, SCORAD and DLQI in adult AD patients (n=50) were 8.51±7.32, 34.8±16.21 and 10.67±5.81, respectively. According to the categories of the SCORAD score (SCORAD<20, 20<SCORAD<40 and SCORAD≥40), the mean scores were 15.04±2.89 (n=14), 28.5±4.93 (n=29) and 47.79±3.81 (n=7) in the child AD patients and 15.65±2.79 (n=10), 30.01±4.58 (n=28), 55.12± 10.91 (n=12) in adult AD patients, respectively.
In children, the SCORAD and CSHQ scores demonstrated a significant correlation (p=0.005; Fig. 1A). There was also a significant correlation between SCORAD and CDLQI scores (p=0.01; Fig. 1B). In adults, the SCORAD and PSQI scores showed no significant correlation (p=0.27; Fig. 1C). On the other hand, there was a significant correlation between the SCORAD and DLQI scores (p<0.001; Fig. 1D). Among the children, there was significant correlation between objective index and CSHQ (p=0.005), subjective index and CSHQ (p=0.01). The objective index and CDLQI, subjective index and CDLQI were also showed significant correlation (p=0.05 and p=0.01). In adult, there was significant correlation between objective index and PSQI (p=0.04), subjective index and PSQI (p< 0.001). The objective index and DLQI, subjective index and DLQI were also showed significant correlation (p=0.04 and p=0.02). Among the subjective index, the pruritus scores are significant association with both CSHQ scores (p=0.002, r=0.752; Fig. 2A) and PSQI scores (p< 0.001, r=0.578; Fig. 2B).
Associations between each component of the CSHQ/PSQI and the SCORAD score are shown in Table 2. In children, the SCORAD score was significantly associated with five components of the CSHQ (bedtime resistance, sleep onset delay, sleep anxiety, parasomnias and sleep disordered breathing). In adults, the SCORAD score was associated with only two components of the PSQI (subjective sleep quality, sleep latency).
We performed this study to evaluate the relationships between clinical disease severity, QOL and sleep quality in children and adults with AD. Several studies have investigated the association between sleep disorders and dermatologic disease. Mostaghimi9 reported the high prevalence of poor mood and sleep problems in chronic skin disorders, including AD and alopecia areata, using the Current Life Functioning questionnaire, the PSQI score and the Beck depression inventory (BDI-II). Camfferman et al.10 reported that children with eczema have significantly reduced neurocognitive functioning including sleep disturbances. They evaluated sleep problems using the sleep disturbance scale for children (SDSC), a neurocognitive assessment by the Wechsler intelligence scale for children (WISC-IV) and overnight polysomnographic (PSG) data, and showed that children with eczema had worse sleep quality on PSG and significantly reduced neurocognitive performance. These two studies did not investigate the association between sleep quality and AD severity. In our study, we evaluated sleep quality according to AD severity in both children and adults.
A recent study by Yano et al.11 evaluated the sleep quality of Japanese adult AD patients by their PSQI score. In their study, PSQI score was associated with SCORAD score, and two components of the PSQI, sleep quality and sleep latency, were significantly associated with SCORAD and DLQI scores. Our study showed that the total score of the sleep questionnaire was not associated with the severity of AD in adult patients, but the sleep quality and sleep latency components of adult patients were significantly associated with AD severity, similar to the Japanese study. In child AD patients of our study, there were significant associations between the total score of the sleep questionnaire and AD severity, and showed a statistical relationship in the five components of the CSHQ, including bedtime resistance and sleep onset delay, which are similar to the sleep latency component of the PSQI. In addition, we evaluated the sleep quality according to SCORAD score which is separated by objective index and subjective index. In both children and adults, sleep quality and QOL are associated with objective signs and subjective symptom in the SCORAD index.
Koca et al.12 evaluated sleep patterns in lichen simplex chronicus (LSC), which were characterized by repeated rubbing and scratching during sleep. They reported that PSG evaluations of 15 LSC patients revealed a significantly higher percentage of stage 2 non-rapid eye movement (REM) sleep and significantly lower percentage of stages 3 and 4 non-REM sleep. Non-REM sleep consists of 4 stages: stages 1 and 2, "light non-REM" sleep, and stages 3 and 4, "deep non- REM" sleep. The scratching episodes were observed in all stages of non-REM sleep, but were most frequent during stages 1 and 2 non-REM sleep. In the light non-REM sleep, a weak stimulus such as the scratching episodes can easily awake the patient and lead to impairment in deep stages of non-REM sleep.
Itching is considered to be the main factor leading to sleep problems in AD patients. We evaluated the pruritus scores of subjective symptom in the SCORAD index which are showed a significant correlation with sleep quality in both children and adults. And, it showed a stronger association in children (r=0.752) than in adults (r=0.578).
In addition, several factors may be provided for the sleep disorder observed in AD patients. Reuveni et al.13 evaluated to characterize the sleep pattern of children with AD. They reported that there is also abnormal sleep fragmentation in well-controlled AD patients. As well as scratching during the active phase of the disease, the itching sensation during clinical remission, itching habit, learned self-comforting behavior, and asthma can also induce the sleep fragmentation in AD patient.
QOL is generally reported to be reduced in patients with AD1415. Holm et al.14 evaluated the QOL in 101 AD patients (66 adults and 35 children) compared with healthy controls and showed that patients with AD had reduced DLQI scores compared to controls (p<0.0001). Sleep disturbance has also been reported to have a major influence on the QOL of AD patients. Chamlin et al.15 reported that poor sleep is a major factor impacting the QOL in about 10% of the children with eczema in their study. Our study also showed a significant correlation between sleep quality and QOL in both children and adults.
In this study, we confirmed the significant association between the severity of AD and sleep disorders in children, and also showed statistical significance between the severity of AD and five components of the sleep questionnaire, including bedtime resistance, sleep onset delay, sleep anxiety, parasomnias and sleep disordered breathing. These sleep disturbances may have a greater effect on children, whose physical and psychosocial development are ongoing. In adults, the total score of the sleep questionnaire was not associated with the severity of AD, but the sleep quality and sleep latency components were significantly associated with the severity of AD. Therefore, sleep problems should not be ignored in adult AD patients. Several limitation of this study should be noted. First, the CSHQ was based on parental reporting that is likely to lead to substantial under- or over-reporting of sleep quality of children. Second, there are many factors, including obesity, affecting the sleep quality in AD patients. We did not evaluate for other factors, except for severity of AD which means the possibility of confounding bias is present. Third, for the objective assessment of sleep quality, the polysomnography should have been performed.
Although sleep problems in AD patients are well recognized, there are few published studies or guidelines concerning the clinical management of sleep disturbances in AD patients. Therefore, adequate guidelines for treating or evaluating AD patients' sleep disorders should be provided. Furthermore, the exact mechanism of sleep disorders in AD patients has not been revealed. Therefore, more neurologic or immunologic studies will be necessary to verify the relationship between sleep disorders and AD.
Figures and Tables
Fig. 1
(A~D) Association between SCORing atopic dermatitis (SCORAD) and children's sleep habits questionnaire (CSHQ)/Pittsburgh sleep quality index (PSQI) scores or children's dermatology life quality index (CDLQI)/dermatology life quality index (DLQI) scores. (A) SCORAD and CSHQ, (B) SCORAD and CDLQI, (C) SCORAD and PSQI, (D) SCORAD and DLQI. (E, F) Association between CSHQ/PSQI scores and CDLQI/ DLQI scores. (E) CSHQ and CDLQI, (F) PSQI and DLQI.

Fig. 2
Association between pruritus scores of subjective symptom in the SCORing atopic dermatitis index and children's sleep habits questionnaire (CSHQ)/Pittsburgh sleep quality index (PSQI) scores. (A) Pruritus score and CSHQ, (B) Prutitus score and PSQI.

Table 1
The mean scores of questionnaires
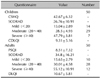
Table 2
Association between CSHQ/PSQI component scores and SCORAD

References
1. Bender BG, Ballard R, Canono B, Murphy JR, Leung DY. Disease severity, scratching, and sleep quality in patients with atopic dermatitis. J Am Acad Dermatol. 2008; 58:415–420.

2. Camfferman D, Kennedy JD, Gold M, Martin AJ, Lushington K. Eczema and sleep and its relationship to daytime functioning in children. Sleep Med Rev. 2010; 14:359–369.

3. Homey B, Steinhoff M, Ruzicka T, Leung DY. Cytokines and chemokines orchestrate atopic skin inflammation. J Allergy Clin Immunol. 2006; 118:178–189.

4. Severity scoring of atopic dermatitis: the SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology. 1993; 186:23–31.
5. Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000; 23:1043–1051.

6. Lewis-Jones MS, Finlay AY. The Children's Dermatology Life Quality Index (CDLQI): initial validation and practical use. Br J Dermatol. 1995; 132:942–949.

7. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28:193–213.

8. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994; 19:210–216.

9. Mostaghimi L. Prevalence of mood and sleep problems in chronic skin diseases: a pilot study. Cutis. 2008; 81:398–402.
10. Camfferman D, Kennedy JD, Gold M, Simpson C, Lushington K. Sleep and neurocognitive functioning in children with eczema. Int J Psychophysiol. 2013; 89:265–272.

11. Yano C, Saeki H, Ishiji T, Ishiuji Y, Sato J, Tofuku Y, et al. Impact of disease severity on sleep quality in Japanese patients with atopic dermatitis. J Dermatol Sci. 2013; 72:195–197.

12. Koca R, Altin R, Konuk N, Altinyazar HC, Kart L. Sleep disturbance in patients with lichen simplex chronicus and its relationship to nocturnal scratching: a case control study. South Med J. 2006; 99:482–485.

13. Reuveni H, Chapnick G, Tal A, Tarasiuk A. Sleep fragmentation in children with atopic dermatitis. Arch Pediatr Adolesc Med. 1999; 153:249–253.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download