Dear Editor:
Erythema annulare centrifugum (EAC), a chronic inflammatory skin disease with an unknown etiology, is considered a hypersensitivity reaction caused by cutaneous or systemic infection, malignant neoplasms, drugs, and various autoimmune diseases, among other factors12. Clinically, EAC presents as erythematous papules or plaques that enlarge by peripheral extension with central clearing, resulting in an annular or polycyclic appearance13. Kim et al.3 previously reported that EAC is associated with various underlying conditions, including infectious and immunologic diseases, consumption of certain food, and drug use. Furthermore, Weyers et al.4 suggested that, although EAC is generally classifiedas either superficial or deep, the term should be reserved for the superficial type only, as these types appear to be separate clinicopathologic entities, and the deep type should hence be classified as another disease entity. Meanwhile, Ziemer et al.5 concluded that EAC is a clinical reaction pattern rather than a specific clinicopathologic entity.
As mentioned above, histopathologically, based on the extent of perivascular lymphocytic infiltration, EAC can be divided into superficial and deep types. However, according to this histopathologic classification, the clinical characteristics are currently not fully understood. Thus, the purpose of this study was to analyze the clinical features, associated diseases, recurrence rates, and treatment outcomes of EAC according to the histopathologic subtypes.
We retrospectively analyzed the medical records and biopsy specimens of 39 patients histopathologically diagnosed with EAC at the Department of Dermatology at the Catholic Medical Center (Seoul, Korea) between January 2003 and December 2013. The Institutional Review Board of the Catholic Medical Center granted approval (XC14RIMI0086) for the review of the medical records, and the study protocol was conducted in accordance with the Helsinki Declaration of 1975 (as revised in 2000). Associated diseases were confined to cases that occurred before the development of EAC and that showed a correlation with the clinical course of EAC. We divided the treatment outcomes into three groups: (1) excellent (>50% improvement in the skin lesion within 3 months after treatment), (2) moderate (took more than 3 months to achieve >50% improvement after treatment), and (3) poor (<50% improvement at 3 months after treatment)6. Recurrence was defined as skin lesions showing aggravation after an excellent response. We reviewed the histopathologic slides of the patients, and classified the cases that presented with various epidermal changes (hyperkeratosis, parakeratosis, spongiosis, or basal vacuolar degeneration) and perivascular lymphocyte infiltration in the upper dermis into superficial EAC. In contrast, cases that showed no or minimal epidermal changes, mild edema in the papillary dermis, and perivascular inflammatory cells (lymphocyte predominant) in the upper and deep dermis were classified as the deep type. Data analysis was conducted using IBM SPSS Statistics ver. 22.0 (IBM, Armonk, NY, USA). For categorical data, χ2 or Fisher's exact test was used as appropriate. A p-value<0.05 was considered statistically significant.
Among the 39 patients, 13 patients (33.3%) showed associated conditions, including cutaneous fungal infection (n=5), pregnancy (n=2), malignancy (thyroid cancer, n=2), autoimmune diseases such as Behcet disease and rheumatoid arthritis (n=2), and medication use (cephalosporin, n=2). Based on the histopathologic findings, 32 cases (82.1%) were classified into the superficial type, and 7 cases (17.9%) into the deep type (Table 1).
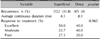
Twenty-seven (superficial type, n=22; deep type, n=5) of the 39 patients had available follow-up data from our clinic after the skin biopsy, and their clinical outcomes were as follows: 5 patients (18.5%) showed persistent skin lesions without improvement (poor response) over 1 year. The average duration of continuous skin lesionswas 4.7 months. Thirteen (48.1%), 7 (25.9%), and 7 patients (25.9%) showed the excellent, moderate, and poor responses, respectively. Of the 7 cases with a poor response, 1 and 6 cases were deep and superficial EAC, respectively. Eleven of the 32 superficial cases (34.4%) were associated with another disease, whereas 2 out of the seven deep cases (28.6%) had associated diseases. These results indicated that there were no remarkable differences in the incidence rates of associated diseases between the superficial and deep types of EAC (p=1) (Table 1). However, a distinct difference between the superficial and deep types was observed for the average duration of continuous skin lesions (4.1 vs. 8.1 months). The recurrence rate was 31.8% for the superficial type, whereas no deep EACs showed recurrence. In terms of treatment outcomes, 27.3% and 20.0% of patients with the superficial and deep types respectively revealed a poor response to treatment; there was little difference between these two types (p=0.965) (Table 2).
There were some limitations to this study, including the fact that it was a retrospective study and that the number of deep-type cases was small. Accordingly, further large-scale prospective studiesare required to ascertain these results.
In conclusion, our findings revealed differences in the clinical outcomes according to the histopathologic subtype of EAC, with the superficial type being associated with a higher recurrence rate and a shorter duration of skin lesions compared with the deep type.
Figures and Tables
Table 1
Demographic and clinical data of 39 patients with erythema annulare centrifugum

Table 2
Clinical features of erythema annulare centrifugum according to histopathologic classification
| Variable | Superficial | Deep | p-value |
|---|---|---|---|
| Recurrence, n (%) | 7/22 (31.8) | 0/5 (0) | |
| Average continuous duration (mo) | 4.1 | 8.1 | |
| Response to treatment (%) | 0.965 | ||
| Excellent | 50.0 | 40.0 | |
| Moderate | 22.7 | 40.0 | |
| Poor | 27.3 | 20.0 |
References
1. Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 463–466.
2. Helbling I, Walewska R, Dyer MJ, Bamford M, Harman KE. Erythema annulare centrifugum associated with chronic lymphocytic leukaemia. Br J Dermatol. 2007; 157:1044–1045.

3. Kim KJ, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. Clinicopathologic analysis of 66 cases of erythema annulare centrifugum. J Dermatol. 2002; 29:61–67.

4. Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003; 25:451–462.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download