Abstract
Background
Ustekinumab is a fully human monoclonal antibody approved for the treatment of chronic moderate-to-severe plaque psoriasis in adults. However, factors including efficacy, tolerability, ease of use, and cost burden may affect ustekinumab utilization. Noncompliance may, in turn, affect treatment response.
Methods
In this phase 4 observational study conducted in Indonesia, Malaysia, Singapore, Korea, and Taiwan, adults with plaque psoriasis receiving ustekinumab were followed for up to 52 weeks. Study endpoints were the proportion of all patients using ustekinumab according to label-recommended intervals and the proportion of Korean patients who achieved a psoriasis area severity index 75 response at week 16. Safety was assessed by monitoring adverse events.
Results
Overall, 169 patients received ustekinumab (Korea, n=102; other countries, n=67). Just over half (56.2%) of patients used ustekinumab with the label-recommended interval from baseline to week 40; the proportion was higher in Korea (73.5%) than in other countries (29.9%), probably because ustekinumab was provided without charge for Korean patients up to week 40. Noncompliance increased after week 40 in Korea and from week 28 in other Asia-Pacific countries, with cost cited as the most common reason. At week 16, 56.9% of Korean patients achieved a Psoriasis Area Severity Index 75 response. Safety results were in line with those seen in previous studies.
Diseases of the skin cause a huge burden on global health, ranking as the 18th leading cause of disability-adjusted life-years worldwide1. Psoriasis, a chronic inflammatory skin disorder associated with several comorbidities, has been shown to negatively affect daily functioning and quality of life2345. In Caucasian populations, psoriasis affects men and women equally, whereas in Mongoloid races, more men than women are affected56. Prevalence among Mongoloid races is somewhat lower than among Caucasians7, ranging from 0.2% in Taiwan57 and 0.3% in Korea8 (population-based surveys) to 0.3% to 1.2% in Japan79 and 1.1% to 5.5% in Malaysia79 (clinic-based studies).
Although the pathophysiology of psoriasis is not fully understood, cytokines such as interleukin (IL)-12, IL-23, and tumor necrosis factor-alpha (TNF-α) have been shown to play important roles in the development of lesions10. IL-12 and IL-23 share a common subunit, p40, which has been shown to be overexpressed in psoriatic plaques1112. Polymorphisms in the gene encoding p40 have also been linked to the pathophysiology of psoriasis13, making p40 a potential target for biologic therapies in psoriasis3. Ustekinumab (Stelara®; Janssen Biotech, Inc., Horsham, PA, USA) is a fully human monoclonal antibody with high specificity for the IL-12/23 p40 subunit, blocking biological activity and inhibiting signaling and subsequent downstream immune activation10. Ustekinumab is approved in multiple countries for the treatment of adults with chronic moderate-to-severe plaque psoriasis. In two phase 3, double-blind, placebo-controlled multicenter trials (PHOENIX-1 and -2) involving 1,996 patients, significantly more ustekinumab-treated patients achieved a psoriasis area severity index (PASI) 75 response at week 12 compared with placebo (p<0.0001)1415. Ustekinumab has also been shown to be effective in Asian patients with moderate-to-severe psoriasis161718.
Long-term safety data indicate that up to 5 years of ustekinumab treatment is generally well tolerated, with no evidence of cumulative toxicity1920, and ustekinumab-treated patients have expressed satisfaction with therapy21. However, for psoriasis treatment, many factors (e.g., perceived benefit, tolerability, ease of use, and cost burden) are likely to determine adherence22, and poor adherence may in turn affect efficacy outcomes. Herein we describe the results of an observational study designed to evaluate how ustekinumab is used and its effects in the real-world setting in selected Asia-Pacific countries.
This was a phase 4, multicenter, open-label, observational study (ClinicalTrials.gov identification number NCT0167-7598) conducted from 29 November 2011 to 30 November 2013. Twelve study sites participated: one each in Indonesia, Singapore, and Taiwan; two in Malaysia; and seven in Korea. The study was performed in accordance with current guidelines on good clinical practice and applicable regulatory- and country-specific requirements (Seoul National University, IRB No. B-1111-139-008; National Taiwan University Hospital, IRB No. 201202059RSA; Yonsei University, IRB No. 4-2011-0568; University of Indonesia, IRB No. 210/H2F1/ETIK/XII/2013; Malaysian Ministry of Health, IRB No. NMRR-11-633-9662; Singapore, IRB No. 2011/01877).
The study design is shown in Fig. 1. Patients were to be treated with ustekinumab for a duration of 52 weeks, with subcutaneous injections administered by the investigator or designee. Ustekinumab exposure was recorded during the initial study site visit (week 0) and at three subsequent visits (weeks 16, 28, and 52). In Korea, an additional two visits (weeks 4 and 40) were planned.
The primary objectives of the study were twofold. The first was to determine how patients use ustekinumab (label-recommended or other/missed-dose interval) in Asia-Pacific countries. For the purposes of this analysis, label-recommended dosing was defined as week 0, week 4, and every 12 weeks thereafter. Doses must have been taken within ±10 days of scheduled time. Once a patient received a dose outside the ±10-day interval, all subsequent doses were considered noncompliant. The second objective was to evaluate efficacy in Korean patients by investigating the proportion of patients who achieved PASI 75 responses at week 16.
In all five Asia-Pacific countries, men and women aged ≥18 years, with a diagnosis of plaque psoriasis according to the dermatologists' clinical judgment, were eligible for inclusion in the study. Patients were required to agree to initiate treatment of ustekinumab on the same day as enrollment and were not permitted to have received any anti-IL-12/23 therapy within six months prior to enrollment. All patients or their legal representatives signed informed consent forms prior to study initiation.
At the time of study initiation, ustekinumab was not being reimbursed in Korea. A local protocol amendment was issued to apply the expected reimbursement guidelines for Korean patients. As a result, the Korean subset of patients were required to meet additional inclusion criteria, including presence of plaque psoriasis for ≥6 months prior to the first administration of ustekinumab; PASI ≥10 at screening and at the time of the first administration of ustekinumab; plaque-type psoriasis covering at least 10% of total body surface area at screening and at the time of first administration of ustekinumab; and nonresponder to, intolerant of, or with contraindications to systemic therapy (methotrexate or cyclosporine) or phototherapy for ≥12 weeks prior to first administration of ustekinumab.
Exclusion criteria included difficulty understanding questions posed by any of the questionnaires, current participation in another clinical study, and active tuberculosis or other severe infections (e.g., sepsis, abscesses, or opportunistic infections).
Reimbursement varied significantly between participating countries when the study was conducted. Patients in Indonesia were required to self-pay (no reimbursement). Patients in Malaysia had to fail to respond to systemic therapy and had to still have severe disease (body surface area ≥30% or PASI ≥20) to qualify for government reimbursement; otherwise, they were required to self-pay. In Singapore, eligible patients had to have met means-tested criteria based on household income and had to have experienced failures of phototherapy and at least two oral systemic treatments. Reimbursement applications had to be renewed after 6 months; patients not eligible for reimbursement were required to self-pay. Patients in Taiwan were eligible for reimbursed treatment if they met minimum baseline criteria of PASI ≥10, prior failure of 3 months of phototherapy, and prior failure of at least two oral systemics—each of 3 months' duration. The Taiwanese national health insurance system paid for the maintenance of biologic therapy only for patients in whom the initial reimbursement criteria were still met (PASI ≥10) and who had a PASI response ≥50% after three injections. In Korea, ustekinumab was provided free of charge through week 40 because of lack of reimbursement at the time of study initiation. Current reimbursement policy requires 60% co-payment by the patient for biologics in dermatologic use.
Because this was an observational study, patients received prescriptions from their physicians or health-care providers, and the medications were supplied by the pharmacy or clinic. In Korea, commercial drug ustekinumab with additional protocol label was supplied to the investigational sites by the local sponsor, to be distributed to patients at each visit up to and including week 40. Patients received ustekinumab according to the recommended dose instructions. For patients weighing ≤100 kg (220 lbs), each dose (week 0, week 4, and every 12 weeks thereafter) was 45 mg; for patients weighing >100 kg (220 lbs), each dose was 90 mg2324.
The primary endpoint of the study was ustekinumab usage. Frequency and percentage of patients in each category (label-recommended or other/missed-dose intervals) and two-sided 95% confidence interval (CI) for percentages were calculated.
For the analysis of efficacy (prespecified endpoint for Korean patients), PASI score was determined. PASI is a physician-administered tool used for grading psoriatic lesion severity and therapeutic response, which produces a numeric score ranging from 0 (no disease) to 72 (maximal disease). The PASI assessment was performed by physicians in all countries at screening/baseline and then at each clinic visit. Every effort was made to ensure continuity of the PASI administrator throughout the study to reduce interrater variability25. For Korean patients, counts and proportions of PASI 75 response over time were displayed with an estimated 95% CI. Comparison between observed and expected PASI 75 response rates was performed using the normal approximation method.
The dermatology life quality index (DLQI) is a 10-item, patient-reported, quality-of-life questionnaire. It was completed by patients in all countries at screening/baseline and at each clinic visit. Change from baseline in DLQI was calculated for weeks 16, 28, 40 (Korea only), and 52. A health economics/medical resource utilization questionnaire (HE/MRU) collected information on demography (patient living status), medical insurance, use of biologic agents, and use of phototherapy in all participating countries. Sections 1 and 2 of the questionnaire were completed by the patient; sections 3 and 4 were completed by the investigator. HE/MRU questionnaires were completed at screening/baseline and then at weeks 16, 28, and 52.
Safety was assessed by monitoring adverse events (AEs) from the day of signing the informed consent form until 30 days after the last study-related procedure. AEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA Version 14.0; MedDRA MSSO, McLean, VA, USA). The incidence of treatment-emergent AEs (TEAEs) was summarized by severity and relationship to ustekinumab by using the system organ class and preferred terms defined by MedDRA. Serious AEs and AEs of interest (e.g., infections, nonmelanoma skin cancer, other malignancies, major adverse cardiovascular events—including cardiovascular death, myocardial infarction, and stroke—or any AE resulting in modification or discontinuation of ustekinumab) were also documented. Vital signs, physical examination results, weight, and waist circumference were also recorded.
To determine the sample size for this study, it was assumed that 50% of patients would use ustekinumab with label-recommended interval and 50% would not. With the planned number of 160 patients to be recruited and with an estimated dropout rate of 20%, it was determined that a precision of 17.9% width of the 95% CI could be obtained with approximately 128 patients who completed the study.
It was assumed that PASI response rates at week 16 would be lower than the rates observed in the PEARL study conducted in Korea and Taiwan17, because eligible patients in the current study had more severe disease and were not required to undertake a washout period from prior therapies, potentially resulting in first-visit PASI scores that were not reflections of true baseline disease. It was, therefore, determined that 84 Korean patients would be required for meaningful PASI results to be calculated; considering a 15% dropout rate, approximately 100 Korean patients should be recruited.
The full analysis set consisted of all patients who were enrolled and who received at least one dose of ustekinumab and completed postbaseline effectiveness measurements regardless of their compliance with the protocol. The safety analysis set consisted of all patients enrolled and who received at least one dose of ustekinumab. All analyses were descriptive in nature because there was no hypothesis testing. PASI measurements were summarized by using mean, standard deviation (SD), median, minimum, and maximum values.
Overall, 169 patients were enrolled into the study, of whom 102 were from Korea. Reimbursement details are shown in Table 1. Patient disposition is shown in Fig. 2. All 169 patients received ustekinumab and were included in the analyses. Both the full analysis set and the safety population therefore comprised 169 patients.
Baseline demographics are reported in Table 2. Overall, three-quarters of patients were male, with a median weight of 72 kg (159 lb); most patients (78%) used concomitant topical antipsoriatics during the study. Although baseline characteristics were broadly similar between patients from Korea and those from other Asia-Pacific countries, the PASI distribution varied. Owing to the additional inclusion criteria, no Korean patients had PASI <10, and more Korean patients had PASI scores ≥15. Furthermore, those from Korea were much less likely to have received prior biologic therapy (21.6%) compared with patients from the other four countries (50.7%). Results from the HE/MRU questionnaire indicated that 100% of patients in Korea had public health insurance, whereas in other Asia-Pacific countries, levels of public health insurance were lower (63%), and almost a quarter of patients (24%) had no health insurance coverage. Only one patient who paid for private insurance coverage was reimbursed a portion of the psoriasis treatment costs, implying that the majority of patients either (1) had received prior treatments that were reimbursed by public health insurance or (2) were required to self-pay for nonreimbursed treatment.
The mean (SD) number of ustekinumab injections was 4.8 (1.31) in Korean patients and 3.5 (1.44) in the remaining patients during the 52-week follow-up period. Primary analysis of the overall patient population showed that 95/169 patients (56.2%; 95% CI, 48.7%~63.7%) used ustekinumab at the label-recommended interval from baseline up to and including week 40. The proportion was much higher in Korean patients (75/102, 73.5%; 95% CI, 65%~82.1%) than in patients from the other Asia-Pacific countries (20/67, 29.9%; 95% CI, 18.9%~40.8%) over 40 weeks.
The numbers of patients receiving ustekinumab at the recommended dosing interval (week 0, week 4, and every 12 weeks thereafter) are shown in Table 3. The compliance rate in Korean patients was higher than in other Asia-Pacific patients at all postbaseline visits; compliance appeared to decline from week 28 onward in non-Korean patients. There was a notable drop in compliance in Korean patients from weeks 40 to 52, which reflects the time point at which the drug was no longer provided for patients without charge. Noncompliant patients had less-frequent dosing than per label.
The reasons for not receiving the study drug as per the recommended dosing schedule (±10 days) are described in Table 4. In Korea, most of the noncompliance occurred at week 52, when the study drug was no longer provided for patients free of charge. As expected, the most common reason for noncompliance at that time point was cost (33.3%), followed by patient choice (16.7%). In the other Asia-Pacific countries, cost was a reason for noncompliance from as early as week 16. More patients in those countries were also noncompliant at week 52 because of a loss of efficacy (20.9%), compared with patients in Korea (2.9%).
The primary efficacy analysis for Korea showed that at week 16, 58/102 patients (56.9%; 95% CI, 47.3%~66.5%) achieved a PASI 75 response. At week 52, the PASI 75 rate in Korean patients was 70.6%.
Changes in median PASI score from baseline are shown in Fig. 3. For the Korean population, the median PASI at baseline was 16.7 (range, 10~72). The PASI score showed a consistent decline as early as week 4. For the four other Asia-Pacific countries, the median PASI score at baseline was 15.5 (range, 2~61); these patients showed a similar decline in PASI score. In Korea, numerically larger mean changes from baseline in PASI were observed in the compliant subgroup (-14.35 at week 16, -15.79 at week 28, and -16.36 at week 52) compared with the noncompliant subgroup (-12.45, -13.26, and -11.61, respectively). Similar changes were observed between compliant and noncompliant subgroups in the other Asia-Pacific countries.
Mean changes from baseline in DLQI in the overall Asia-Pacific population at week 52 by PASI 50, 75, and 90 responders were -7.5, -8.0, and -8.4 at week 16, and -8.1, -8.9, and -11.2, respectively, at week 52. Spearman's correlation coefficients were 0.307 for week 16 and 0.389 for week 52, indicating that the PASI response and the DLQI were positively correlated and maintained a proportional relationship (i.e., patients showed linear improvement in both variables over the course of the study). That positive correlation was also demonstrated for the subgroup of Korean patients and for the subgroup of patients from the other Asia-Pacific countries.
TEAEs are shown in Table 5. Overall, 65.1% of patients reported at least one TEAE, although only 28.4% were assessed by the investigator to be potentially drug related. The most commonly reported AEs were infections, of which the two most frequent were nasopharyngitis (10.7%) and upper respiratory tract infections (10.1%). The second most common class of TEAEs were skin disorders, of which the most frequently reported were pruritus (10.1%) and urticaria (3%). Four patients (2.4%) had a TEAE that led to discontinuation of treatment.
During the study period, 14 patients (8.3%) had serious AE. These were bone fracture (n=3), malignancy (n=2), and one case each of myocardial infarction, pustular psoriasis, psoriatic arthropathy, hypertension, pyrexia, pneumonia, limb injury, epistaxis, and vocal cord polyp. TEAEs of interest based on theoretical risks associated with IL-12/23 inhibition (infection, malignancy) and/or population risks in patients with psoriasis (major adverse cardiovascular events) were also evaluated. Overall, 32% of patients reported infections—including one case of pneumonia—but no cases of tuberculosis or opportunistic infections. There were two malignancies: one case of colon cancer and one of recurrent hepatocellular carcinoma (HCC). One myocardial infarction was reported, in a patient with a preexisting history of cardiovascular disease.
No clinically significant changes in vital signs and physical findings were observed during the study. No deaths occurred during the study period, although the patient with recurrent HCC died after completion of the study.
This was a phase 4, multicenter, open-label observational study designed to determine how patients use ustekinumab in a naturalistic setting in the Asia-Pacific region and to examine efficacy outcomes in Korean patients.
More than half of Asia-Pacific patients used ustekinumab according to the label-recommended schedule; however, higher compliance rates were observed up to week 40 in the Korean population when ustekinumab was provided free of cost; after week 40, compliance declined noticeably. Compliance also declined from week 28 onward in patients from the other Asia-Pacific countries, with cost and efficacy cited as major reasons for discontinuing or delaying treatment. Cost therefore appears to be an important driver for not receiving the drug at the recommended schedule. As such, the results of clinical trials using biologic therapies may differ from real-life clinical situations in which patients are required to self-pay or co-pay for treatment. Patients may be less likely to use non-reimbursed medication regardless of efficacy, or they may delay treatments beyond the recommended intervals in an attempt to reduce costs. Of note, fewer Korean patients in this study had received prior biologic therapy compared with patients in other Asia-Pacific countries—possibly because of lack of reimbursement for these therapies in Korea as a result of health insurance guidelines26, and because of patients' unwillingness or inability to self-pay.
Our study has several important limitations, including small numbers of patients, different entry criteria between patients from Korea and other Asia-Pacific countries, and the provision of the drug for free in Korea up to only week 40 because of lack of reimbursement in Korea at the time of study initiation. The countries involved in the study had different reimbursement criteria from one another, and those criteria are likely to have affected treatment compliance in different ways. As such, only generalized conclusions can be drawn related to how treatment cost may affect whether patients elect to receive treatment at the recommended dosing intervals or instead become noncompliant.
Efficacy evaluations constituted a prespecified endpoint for the Korean population. Although efficacy data were subject to the same limitations described earlier, nevertheless there appears to be a consistent decline in disease severity from as early as week 4. Exploratory analysis also indicated a consistent decline in median PASI scores in patients from other Asia-Pacific countries. However, because of the uncontrolled and open-label nature of the study, analyses of PASI 75 responses are difficult to contextualize accurately. Lack of inclusion criteria that specify prior drug washout periods may suggest that the observations seen at baseline are not true representations of treatment-naive baseline values. Thus, for this study design, the results showing absolute PASI values over time may be more meaningful measures of efficacy.
Safety evaluations were in line with previous reports about ustekinumab. A previous study with ustekinumab indicated that the risk/benefit of ustekinumab treatment should be carefully assessed in patients with hepatitis C virus (HCV) and/or HCC because there is a theoretical risk of virus reactivation during treatment with ustekinumab27. In the present study, one patient with HCV and a history of HCC suffered a relapse of the HCC during the treatment period. However, the patient had an incomplete resection of the prior HCC and was treated with an anti-TNF agent subsequent to the resection and prior to ustekinumab treatment.
In conclusion, more than half of all Asia-Pacific patients used ustekinumab as per label-recommended dose interval, but reimbursement variations between countries may have confounded the overall results. Ustekinumab was efficient in treating patients with plaque psoriasis in the real-world setting in Asia Pacific countries, and compliant patients received slightly greater efficacy benefits. Ustekinumab was generally well tolerated in this population, with a safety profile consistent with that reported in the prescribing information.
Figures and Tables
 | Fig. 3Change in median PASI scores from baseline. (A) Korea. (B) Other Asia-Pacific countries. Compliant=taking ustekinumab in line with the recommended dosing (week 0, week 4, and every 12 weeks thereafter; dose to be taken within ±10 days). PASI: psoriasis area severity index. |
Table 1
Number of reimbursements of ustekinumab by country

Table 2
Baseline demographics at study entry

PASI: psoriasis area severity index, SD: standard deviation. *Includes adalimumab, alefacept, efalizumab, etanercept, infliximab, and ustekinumab. †Data based on prior treatments up to 6 months before the first (baseline) visit. ‡Includes acitretin, cyclosporine, etretinate, fumarates, methotrexate, and systemic corticosteroids. §Includes psoralen ultraviolet A and narrow-band ultraviolet B. ∥Includes daivobet, calcipotriol, xamiol, coal tar, and coal tar solution.
Table 3
Analysis of ustekinumab dosing schedule by study visit
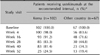
Table 4
Reasons for noncompliance (not receiving study drug as recommended)

Table 5
Treatment-emergent adverse events (TEAEs)

ACKNOWLEDGMENT
The MARCOPOLO study was funded by Janssen Asia-Pacific Medical Affairs, Johnson & Johnson Pty Ltd. Medical writing support and editorial assistance were provided by Sally-Anne Mitchell, PhD, of ApotheCom (Yardley, PA, USA). The authors also thank the following for their assistance with the running of the study: Dr Kwee Eng Tay, Department of Dermatology, Hospital Sultanah Aminah, Johor Bahru, Malaysia; Dr Eun So Lee, Ajou University Medical Center, Suwon, Korea; Dr Seong Jun Seo, Chung-Ang University Hospital, Seoul; Dr Joo Young Rho, Gachon University Gil Hospital, Incheon, Korea; Dr Gwang Seong Choi, Inha University Hospital, Incheon, Korea; Dr So Yun Cho, SMG-SNU Boramae Medical Center, Seoul.
Sang Woong Youn has participated as an advisory board member for AbbVie, Novartis, and Janssen. Tsen-Fang Tsai has conducted clinical trials or received honoraria for serving as a consultant for Pfizer, Novartis, Celgene, Eli Lilly Pharmaceuticals, and Janssen and has received speaking fees from AbbVie. Colin Theng has participated as an advisory board member for Pfizer and Janssen, acted as a consultant for LEO Pharma, and provided research support for Novartis, Pfizer, and LEO Pharma. Siew-Eng Choon has participated as an advisory board member for Pfizer, Janssen, Novartis, AbbVie, and Boehringer Ingelheim and has received payments from Janssen for conducting clinical research. Benny E. Wiryadi has received payments from Janssen for conducting clinical research. Antonio Pires is a full-time employee of Janssen Asia-Pacific. Weihao Tan is a full-time employee of Janssen Asia-Pacific. Min-Geol Lee has acted as a consultant for and received payments from Janssen, Novartis, Pfizer, and Eli Lilly for conducting clinical research.
References
1. Hay RJ, Johns NE, Williams HC, Bolliger IW, Dellavalle RP, Margolis DJ, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014; 134:1527–1534.

2. Parisi R, Symmons DP, Griffiths CE, Ashcroft DM. Identification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project team. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013; 133:377–385.

4. Lee YW, Park EJ, Kwon IH, Kim KH, Kim KJ. Impact of psoriasis on quality of life: relationship between clinical response to therapy and change in health-related quality of life. Ann Dermatol. 2010; 22:389–396.

5. Tsai TF, Wang TS, Hung ST, Tsai PI, Schenkel B, Zhang M, et al. Epidemiology and comorbidities of psoriasis patients in a national database in Taiwan. J Dermatol Sci. 2011; 63:40–46.

6. Na SJ, Jo SJ, Youn JI. Clinical study on psoriasis patients for past 30 years (1982-2012) in Seoul National University Hospital Psoriasis Clinic. J Dermatol. 2013; 40:731–735.

7. Chandran V, Raychaudhuri SP. Geoepidemiology and environmental factors of psoriasis and psoriatic arthritis. J Autoimmun. 2010; 34:J314–J321.

8. Lee H, Lee MH, Lee DY, Kang HY, Kim KH, Choi GS, et al. Prevalence of vitiligo and associated comorbidities in Korea. Yonsei Med J. 2015; 56:719–725.

9. Raychaudhuri SP, Farber EM. The prevalence of psoriasis in the world. J Eur Acad Dermatol Venereol. 2001; 15:16–17.

10. O'Neill JL, Kalb RE. Ustekinumab in the therapy of chronic plaque psoriasis. Biologics. 2009; 3:159–168.
11. Nestle FO, Conrad C. The IL-12 family member p40 chain as a master switch and novel therapeutic target in psoriasis. J Invest Dermatol. 2004; 123:xiv–xv.

12. Lew W, Lee E, Krueger JG. Psoriasis genomics: analysis of proinflammatory (type 1) gene expression in large plaque (Western) and small plaque (Asian) psoriasis vulgaris. Br J Dermatol. 2004; 150:668–676.

13. Cargill M, Schrodi SJ, Chang M, Garcia VE, Brandon R, Callis KP, et al. A large-scale genetic association study confirms IL12B and leads to the identification of IL23R as psoriasis-risk genes. Am J Hum Genet. 2007; 80:273–290.

14. Leonardi CL, Kimball AB, Papp KA, Yeilding N, Guzzo C, Wang Y, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet. 2008; 371:1665–1674.

15. Papp KA, Langley RG, Lebwohl M, Krueger GG, Szapary P, Yeilding N, et al. PHOENIX 2 study investigators. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet. 2008; 371:1675–1684.

16. Zhu X, Zheng M, Song M, Shen YK, Chan D, Szapary PO, et al. LOTUS Investigators. Efficacy and safety of ustekinumab in Chinese patients with moderate to severe plaque-type psoriasis: results from a phase 3 clinical trial (LOTUS). J Drugs Dermatol. 2013; 12:166–174.
17. Tsai TF, Ho JC, Song M, Szapary P, Guzzo C, Shen YK, et al. PEARL Investigators. Efficacy and safety of ustekinumab for the treatment of moderate-to-severe psoriasis: a phase III, randomized, placebo-controlled trial in Taiwanese and Korean patients (PEARL). J Dermatol Sci. 2011; 63:154–163.

18. Igarashi A, Kato T, Kato M, Song M, Nakagawa H. Japanese Ustekinumab Study Group. Efficacy and safety of ustekinumab in Japanese patients with moderate-to-severe plaque-type psoriasis: long-term results from a phase 2/3 clinical trial. J Dermatol. 2012; 39:242–252.

19. Reich K, Papp KA, Griffiths CE, Szapary PO, Yeilding N, Wasfi Y, et al. PHOENIX 1, PHOENIX 2, and ACCEPT investigators. An update on the long-term safety experience of ustekinumab: results from the psoriasis clinical development program with up to four years of follow-up. J Drugs Dermatol. 2012; 11:300–312.
20. Kimball AB, Papp KA, Wasfi Y, Chan D, Bissonnette R, Sofen H, et al. Long-term efficacy of ustekinumab in patients with moderate-to-severe psoriasis treated for up to 5 years in the PHOENIX 1 study. J Eur Acad Dermatol Venereol. 2013; 27:1535–1545.

21. Callis Duffin K, Yeung H, Takeshita J, Krueger GG, Robertson AD, Troxel AB, et al. Patient satisfaction with treatments for moderate-to-severe plaque psoriasis in clinical practice. Br J Dermatol. 2014; 170:672–680.

22. Yeung H, Wan J, Van Voorhees AS, Callis Duffin K, Krueger GG, Kalb RE, et al. Patient-reported reasons for the discontinuation of commonly used treatments for moderate to severe psoriasis. J Am Acad Dermatol. 2013; 68:64–72.

23. Stelara® (Ustekinumab). Highlights of prescribing information [Internet]. Horsham, PA: Janssen Biotech, Inc.;2012. updated 2014. cited 2015 Mar. Available at: http://www.stelarainfo.com/pdf/PrescribingInformation.pdf.
24. Stelara® (Ustekinumab). Summary of product characteristics [Internet]. Beerse: Janssen-Cilag International NV;2014. updated 2013. cited 2015 Mar. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000958/WC500058513.pdf.
25. Youn SW, Choi CW, Kim BR, Chae JB. Reduction of Inter-Rater and Intra-Rater Variability in Psoriasis Area and Severity Index Assessment by Photographic Training. Ann Dermatol. 2015; 27:557–562.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download