Abstract
Background
Although the therapeutic mechanism of balneotherapy for atopic dermatitis has not been clarified, many atopic patients who visit thermomineral springs have shown clinical improvements.
Objective
This study was aimed to evaluate the immunomodulatory effect of thermomineral water balneotherapy on the atopic dermatitis murine model.
Methods
The oxazolone-induced atopic dermatitis murine model was used to evaluate the therapeutic effect of balneotherapy with Deokgu thermomineral water compared with distilled water. Histologic evaluation and confocal microscopic imaging were performed to analyze the lesional expression of cluster-of-differentiation (CD)4 and forkhead box p3 (Foxp3). Lesional mRNA expression of interleukin (IL) 33, thymic stromal lymphopoietin (TSLP), and Foxp3 was evaluated by real-time reverse transcription polymerase chain reaction.
Results
Compared with the distilled water bath group, confocal microscopic evaluation of CD4 and Foxp3 merged images showed increased expression of regulatory T cells in the thermomineral balneotherapy group. The lesional mRNA level of IL-33 showed a reduced trend in the thermomineral balneotherapy group, whereas the level of mRNA of Foxp3 was increased. TSLP showed a decreased trend in both distilled water and thermomineral water bath groups. There was a trend of reduced expression in lesional IL-33 mRNA but increased cell count of CD4+ Foxp3+ regulatory T cells in thermomineral balneotherapy compared with distilled water bath.
Atopic dermatitis is a chronic disease that can persist for an entire lifetime. It strongly impairs the quality of life of affected patients. Local and systemic treatments including glucocorticoid are effective. However, their effects are transient, with possible side effects that cause concern. Many patients with atopic dermatitis request alternative therapies because they perceive these alternatives as being helpful. One of the promising alternative therapies for atopic dermatitis is thermomineral balneotherapy. This treatment modality offers a natural, multifactorial, complementary, and nontoxic alternative to traditional pharmacologic treatment.
Balneotherapy refers to immersion in baths or pools of thermomineral water. Although balneotherapy is not accepted as a well-established treatment modality, it seems to have therapeutic potentials in various diseases. Atopic dermatitis is one of the most frequently treated diseases by balneotherapy. Korea is known to have sufficient resources of thermomineral water. Several thermomineral springs in Korea are known for their therapeutic effects on skin disease. Onyang Spa is famous because Sejong the Great (reigned from 1418 to 1450) of the Joseon Dynasty cured his chronic skin disease by bathing in it1. Despite a long history of balneotherapy in Korea, few reports have evaluated the mechanism involved in its therapeutic effects.
Balneotherapy is known to have chemical, thermal, mechanical, and immunomodulatory effects. The chemical components of the thermal water that are known to have beneficial effects on skin include sulfur, magnesium, and selenium2. Heat may have an anti-inflammatory effect3. Thermal stimulation can cause vasodilatation, enhance blood circulation, and decrease blood pressure. The moisturizing effect of bathing on the stratum corneum and the desquamation of dead keratinocytes can be beneficial to the skin. In addition, the psychological effects of balneotherapy cannot be overlooked.
The therapeutic effects of balneotherapy on refractory atopic dermatitis in Japan have been reported4. Minerals such as manganese and iodide ions in thermal water have been reported to have bactericidal activity against Staphylococcus aureus56. Although Japan is geographically near Korea, the Korean peninsula, located distant from the circum-Pacific volcanic belt, rests on a firm foundation. In Korea, it is difficult to find hot spring water related to volcanoes as in Japan. The areas of distribution of thermomineral water in Korea coincide with the areas of granite, where the water temperature is lower than in hot springs, which derive heat from magma as in Japan1. The Deokgu thermomineral water is derived from low-temperature springs located on the southeast area of the Korean peninsula. The therapeutic mechanism of balneotherapy in Deokgu has not been evaluated.
The oxazolone-induced atopic dermatitis murine model, a well-established murine model, has been used in many studies on atopic dermatitis7. In the present study, the effect of mineral water bath versus distilled water bath was evaluated using the oxazolone-induced atopic dermatitis murine model. The mRNA expression of inflammatory cytokines was measured in the skin. Histologic evaluations and confocal microscopic evaluation of lesional cluster-of-differentiation (CD)4+ forkhead box p3 (Foxp3)+ regulatory T cells were performed.
The hydrochemical analysis of Deokgu thermomineral water was performed as described previously8. Temperature, pH, electrical conductivity, and alkalinity were measured in situ. Collected water samples were preserved in polyethylene bottles after filtering with 0.45-µm cellulose membrane. Samples for cation analysis were acidified to pH <2 by adding a few drops of ultra-pure nitric acid. Alkalinity was measured in the field using an acid-neutralizing titration technique and then converted to equivalent HCO3- and CO32- concentrations. Water samples were analyzed for Na+, K+, Ca+, Mg2+, SiO2, and total Fe concentrations using induced coupled plasma-atomic emission spectrometry (PerkinElmer Optima 3000XL; Meinhard, Golden, CO, USA) and atomic adsorption spectrometry (Perkin Elmer Analyst 100; Meinhard). Anions such as Cl-, SO42-, PO43-, and F- were analyzed by ion chromatography (Dionex 120; Dionex, Sunnyvale, CA, USA). Careful quality control was achieved by checking sample containers and reagents for background readings by preparing and analyzing blank samples and using duplicate or triplicate subsamples and standard materials.
Female hairless mice (Hos:HRM-2, 6~8 weeks old, total n=30; Saeron Bio Inc., Seoul, Korea) were housed for 2 weeks in a temperature-controlled room at 25℃ with 60% relative humidity and free access to standard laboratory diet and water. Mice were treated according to the ethical guidelines of the animal laboratory of Uijeongbu St. Mary's Hospital. All animal procedures were approved by the Ethics of Animal Care and Use Committee of Uijeongbu St. Mary's Hospital, College of Medicine, Catholic University of Korea (UJA 12-11A) and conformed to international standards. Thirty mice were divided into the following five groups with six mice in each group: Group 1, normal control mice group; Group 2, oxazolone-induced atopic dermatitis mice group sacrificed at treatment day 0; Group 3, oxazolone-induced atopic dermatitis mice with distilled water bath for 1 week; Group 4, oxazolone-induced atopic dermatitis mice with mineral water balneotherapy for 1 week; Group 5, oxazolone-induced atopic dermatitis mice without treatment sacrificed at day 7.
Oxazolone (4-ethoxymethylene-2-phenyl-2-oxazolin-5-one) was purchased from Sigma-Aldrich (St. Louis, MO, USA). Six mice were sacrificed before oxazolone application as normal control (Group 1). For other 24 mice, atopic dermatitis-like skin lesions were induced by repeated oxazolone challenge, as described previously7. Briefly, mice were topically sensitized by 10 µl of 5% oxazolone. A week later, 60 µl 0.1% oxazolone was topically applied on both flanks once every other day for an additional 2 weeks. Six mice were sacrificed after induction of atopic dermatitis by oxazolone (Group 2, positive control). Group 3 mice (n=6) underwent bathing with distilled water for 5 minutes once daily for 1 week. Another six mice (Group 4) underwent bathing with Deokgu thermomineral water for 5 minutes once daily for 1 week. Water was kept at a constant temperature of 38℃ during the bath. The other six mice without treatment (Group 5) were sacrificed on day 7 to study spontaneous healing without bath.
For histologic evaluation, skin samples were fixed with 10% paraformaldehyde and embedded in paraffin. Paraffin-embedded tissue sections were deparaffinized in xylene and rehydrated in a graded series of alcohol solution. Slides were stained with standard hematoxylin and eosin (H&E, Sigma-Aldrich).
For confocal fluorescence microscopic evaluation, paraffin-embedded tissue sections were deparaffinized in xylene, rehydrated in a graded series of alcohol solution, and underwent antigen retrieval process in 10 mM citrate buffer. Sample slides were washed with phosphate-buffered saline. The blocking solution used in this study was purchased from Invitrogen (Carlsbad, CA, USA). Slides were stained for regulatory T cells using phycoerythrin-labeled anti-Foxp3 (eBioscience, San Diego, CA, USA) and PerCP-labeled anti-CD4 (Biolegend, San Diego, CA, USA). 4',6-Diamidino-2-phenylindole was purchased from Invitrogen. After incubation overnight at 4℃, slides were analyzed using an LSM 510 Meta confocal microscopy system (Carl Zeiss, Oberkochen, Germany).
On the day of sacrifice, the dorsal skin of each mouse was excised and divided into two specimens: one for histopathological evaluation and another for mRNA extraction. The total mRNA was extracted from the back skin using TRIzol (Invitrogen), followed by isopropanol precipitation and washing with 70% ethanol. RNA pellets were dissolved in diethylpyrocarbonate-treated water. RNA was quantified, and the purity was evaluated by measuring the optical density at 260 and 280 nm and calculating the 260/280 ratio with a target ratio of more than 1.8. Using 1 µg of total RNA template, cDNA was prepared using reverse transcription system (Promega, Madison, WI, USA), oligo (dT), and random hexamer primers. Reaction mixtures were amplified with SYBR® Premix Ex Taq™ (Tli RNaseH Plus) kit (Takara, Shiga, Japan) using an iQ5 real-time polymerase chain reaction (PCR) detection system (Bio-Rad, Hercules, CA, USA). The housekeeping gene glyceraldehydes-3-phosphate dehydrogenase (GAPDH) was used as an internal control. The sequences for PCR primers and reference numbers for probes (Universal Probe Library; Roche Applied Science) were as follows: interleukin (IL) 33, forward primer, 5'-TCC AAC TCC AAG ATT TCC CC-3', reverse primer, 5'-CAT GCA GTA CAC ATG GCA CA-3'; thymic stromal lymphopoietin (TSLP), forward primer, 5'-ACG GAT GGG GCT AAC TTA CA-3', reverse primer, 5'-AGT CCT CGA TTT GCT CGA AC-3'; Foxp3, forward primer, 5'-CCC ATC CCC AGG AGT CTT G-3', reverse primer, 5'-ACC ATA CTA GGG GCA CTG T-3'; GAPDH, forward primer, 5'-TCC ACT GGC GTC TTC AC, reverse primer-3', 5'-GGC AGA GAT GAT GAC CCT TTT-3', probe 9. Cytokines and GAPDH levels were calculated relative to the amounts found in standard sample. Cytokine levels were normalized using GAPDH mRNA levels as internal control.
The mRNA expression levels of cytokines in the dermis were expressed as mean±standard deviation. Kruskal-Wallis test was used for statistical analysis. All analyses were performed using Statistical Analysis Software version 9.1 (SAS Institute, Cary, NC, USA). Differences were considered statistically significant when p<0.05.
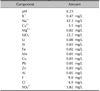
Deokgu thermomineral water was classified as sodium bicarbonate-type thermomineral water with pH 8.23 and low mineral content of 160 mg/L. However, the level of fluoride was up to 9.8 mg/L. In South Korea, excessive fluoride concentrations are frequently encountered in deep thermomineral water, especially in sodium bicarbonate-type bedrock groundwater. The relationship between fluoride concentration and water-rock interaction in various aquifers with different geologic setting has been reported previously (Table 1)9.
Compared with normal mice (Group 1), oxazolone-induced atopic dermatitis mice (Group 2) showed epidermal hyperplasia and inflammatory cell infiltration in the dermis. After 1 week of balneotherapy, the distilled water bath (Group 3) and mineral water bath (Group 4) groups showed reduced inflammation in the dermis. However, inflammation was not substantially decreased in oxazolone-induced mice without treatment (Group 5) (Fig. 1).
To find Foxp3+ regulatory T cell, CD4 (green) and Foxp3 (red) were stained for confocal microscopic evaluation. The yellow spot in merged images representing mixture of CD4 (green) and Foxp3 (red) was considered as CD4+ Foxp3+ regulatory T cells. The number of CD4+ T cells including inflammatory lymphocytes was increased after oxazolone induction (Group 2) but decreased after 1 week of bath (Group 3 and Group 4). As in the histologic evaluation, the inflammatory cell infiltrates in oxazolone-induced mice without treatment group (Group 5) remained, compared with the treatment groups (Group 3 and 4).
Interestingly, in the Foxp3 stain, the red spot was remarkable in the mineral water bath group (Group 4) compared with that in Groups 3 and 5. In CD4 and Foxp3 merged images, the number of yellow spots was relatively high in the mineral water bath group (Group 4) (Fig. 1).
Compared with the normal control group (7.54±4.11-fold in Group 1), oxazolone-induced hairless mice showed a marked increase in IL-33 mRNA expression (24.17±17.93-fold in Group 2). Elevated mRNA expression of IL-33 was maintained for a week with distilled water bath (22.29±8.76-fold in Group 3) or without bath (25.85±22.19-fold in Group 5). However, a decrease in IL-33 mRNA expression in the skin was observed in the mineral water bath group (2.83±1.50-fold in Group 4). There was no significant statistical difference among groups (p>0.05) (Fig. 2A).
The relative mRNA expression of TSLP in the normal mice group was 0.48±0.13-fold (Group 1). After oxazolone induction, the mRNA level of TSLP increased 1.14±0.42-fold (Group 2). Without treatments, the level of TSLP was 1.10±1.80-fold in Group 5. However, both distilled water and mineral water bath groups (0.60±9.68- and 0.45±0.41-fold in Group 3 and Group 4, respectively) showed decreased levels of TSLP compared with the normal group. There was no significant (p>0.05) difference in TSLP expression levels among groups (Fig. 2B).
Compared with Foxp3 expression in the normal control group (1.00±1.31-fold), a slightly increased trend of Foxp3 expression was observed in Group 2 (1.56±0.60-fold) and Group 5 (1.76±0.70-fold). A moderately increased trend of Foxp3 expression was observed in the distilled water bath group (2.93±0.89-fold in Group 3). A substantially increased trend was observed in the mineral water bath group (4.42±3.99-fold in Group 4). However, there was no statistically significant (p>0.05) difference among groups in terms of Foxp3 expression levels (Fig. 2C).
Several studies evaluated the therapeutic effect of mineral water bath on atopic dermatitis10111213. A large cohort study demonstrated the efficacy of thermal spring water bath on atopic dermatitis patients (n=5,916) in France10. Clinical improvement was observed using the scoring atopic dermatitis (SCORAD) index. Thermal mineral water therapy has been known to have immunomodulatory effects on Th1- and Th2-dependent cytokine productions11. Avène Thermal Spring Water was observed to have an anti-Th2 effect that was beneficial for the management of atopic dermatitis12. Inhibition of tumor necrosis factor α-induced E-selectin and intercellular adhesion molecule 1 expression in human endothelial cells was attributed as the mechanism of the immunomodulatory effect of Avène Thermal Spring Water13.
In Korea, a clinical study evaluated the therapeutic efficacy of Haeundae hot spring water therapy in 28 atopic dermatitis patients14. A study that used a murine model revealed that the immunomodulatory effect of Suanbo thermomineral water was through the modification of the Th2 response, suggesting that regulatory T cell might be involved in anti-inflammation15. Thermomineral water was suggested to decrease proinflammatory cytokines in HaCaT cells with an effect on differentiation of CD4+ T cells16. However, the therapeutic mechanisms of balneotherapy with Korean thermal water on atopic dermatitis remain to be elucidated.
In this study, we observed the therapeutic effect of atopic dermatitis by Deokgu thermomineral water (sodium bicarbonate type) using lesional mRNA expression of IL-33 and TSLP as well as confocal microscopy of Foxp3+ regulatory T cells. Since Man et al.7 introduced the hapten-induced atopic murine model, the oxazolone-induced atopic dermatitis murine model has been used in many studies. In this study, IL-33 and TSLP were found to be expressed in oxazolone-induced murine model.
IL-33 is an important cytokine in atopic dermatitis17. Recently, a relationship between serum IL-33 level and disease severity of atopic dermatitis was reported18. Anti-IL-33 therapy was considered as a new therapeutic target in atopic dermatitis treatment19. The level of lesional IL-33 mRNA showed decreased trend after Deokgu thermomineral balneotherapy, suggesting that thermomineral hydrotherapy can be used as a safe and effective adjuvant treatment option for atopic dermatitis.
TSLP, an IL-7-like cytokine, is linked to the pathogenesis of allergic diseases including atopic dermatitis2021. In this study, the level of lesional TSLP expression was decreased after bath with both distilled water and thermomineral water, suggesting that the bathing itself can have therapeutic effect on atopic dermatitis regardless of the active ingredients in water.
Although the role of regulatory T cell in atopic dermatitis is controversial, it is obvious that regulatory T cells have anti-inflammatory effects on the skin. In this study, the presence of CD4+ Foxp3+ regulatory T cells in the skin was investigated by confocal microscopic evaluation. Oxazolone-induced atopic skin showed an increased number of CD4+ Foxp3+ regulatory T cells that might explained the increase in oxazolone-induced inflammation. Regulatory T cells disappeared when the inflammation subsided and was controlled after a week. However, the higher number of regulatory T cells in the mineral water bath group remained for a longer duration compared with the distilled water bath group. The results of mRNA expression of Foxp3 in the skin coincided with the confocal microscopic evaluation. Recently, the role of regulatory T cells has been evaluated, and the importance of anti-inflammation by regulatory T cells is evident in several studies. Our results suggest that the immunomodulatory effects of thermomineral balneotherapy are moderated by the prolonged effect of regulatory T cells.
There are several limitations of this study. First, the number of mice (n=6 in each group) was too small to find statistical significance. However, the present study was experimental study that had strict control of the environment of the subjects. The description of decreased trend in IL-33 mRNA fold expression and increased trend of CD4+ Foxp3+ regulatory T cell by confocal microscopic evaluation are appropriate for experimental murine study. Second, the duration of treatment for a week is relatively short to find the efficacy of balneotherapy. Third, the active components of thermomineral balneotherapy that might have contributed to the therapeutic effects remain to be elucidated.
Despite these limitations, this study seems to provide the scientific evidence for thermomineral therapy with alkalic sodium bicarbonate-type hot spring water to treat atopic dermatitis in the Korean peninsula. Balneotherapy can be a safe and effective adjuvant treatment option for atopic dermatitis patients.
Figures and Tables
 | Fig. 1Histologic and confocal microscopic evaluation (×40). Cluster-of-differentiation (CD) 4 and forkhead box p3 (Foxp3) were stained green and red, respectively, for confocal microscopic evaluation. The yellow spot in the merged images represented the CD4+ Foxp3+ regulatory T cells. In the merged image, yellow CD4+ Foxp3+ regulatory T cells showed an increased trend in Group 4. |
 | Fig. 2mRNA fold expression of interleukin (IL) 33 (A), thymic stromal lymphopoietin (TSLP) (B), and forkhead box p3 (Foxp3) (C) in the skin. Although there was no statistical significance among groups (p>0.05), Group 4 showed a decreased trend in lesional mRNA fold expression of IL-33 and TSLP but increased trend in lesional mRNA fold expression of Foxp3. |
Table 1
Hydrochemical analysis of Deokgu thermomineral water
References
2. Kim JW. Therapeutic effectiveness and its underlying immunologic mechanisms of Korean hot spring water on atopic dermatitis. J Korean Acad Hot Spring. 2012; 1:48–54.
3. Cozzi F, Lazzarin P, Todesco S, Cima L. Hypothalamic-pituitary-adrenal axis dysregulation in healthy subjects undergoing mud-bath applications. Arthritis Rheum. 1995; 38:724–726.

4. Kubota K, Machida I, Tamura K, Take H, Kurabayashi H, Akiba T, et al. Treatment of refractory cases of atopic dermatitis with acidic hot-spring bathing. Acta Derm Venereol. 1997; 77:452–454.
5. Inoue T, Inoue S, Kubota K. Bactericidal activity of manganese and iodide ions against Staphylococcus aureus: a possible treatment for acute atopic dermatitis. Acta Derm Venereol. 1999; 79:360–362.

6. Akiyama H, Yamasaki O, Tada J, Kubota K, Arata J. Antimicrobial effects of acidic hot-spring water on Staphy-lococcus aureus strains isolated from atopic dermatitis patients. J Dermatol Sci. 2000; 24:112–118.

7. Man MQ, Hatano Y, Lee SH, Man M, Chang S, Feingold KR, et al. Characterization of a hapten-induced, murine model with multiple features of atopic dermatitis: structural, immunologic, and biochemical changes following single versus multiple oxazolone challenges. J Invest Dermatol. 2008; 128:79–86.

8. Lee YB, Lee JY, Lee HJ, Yun ST, Lee JT, Kim HJ, et al. Immunomodulatory effects of balneotherapy with hae-un-dae thermal water on imiquimod-induced psoriasis-like murine model. Ann Dermatol. 2014; 26:221–230.

9. Chae GT, Yun ST, Mayer B, Kim KH, Kim SY, Kwon JS, et al. Fluorine geochemistry in bedrock groundwater of South Korea. Sci Total Environ. 2007; 385:272–283.

10. Merial-Kieny C, Mengual X, Guerrero D, Sibaud V. Clinical efficacy of Avène hydrotherapy measured in a large cohort of more than 10,000 atopic or psoriatic patients. J Eur Acad Dermatol Venereol. 2011; 25:Suppl 1. 30–34.

11. Portalès P, Ariès MF, Licu D, Pinton J, Hernandez-Pion C, Gall Y, et al. Immunomodulation induced by Avène spring water on Th1- and Th2-dependent cytokine production in healthy subjects and atopic dermatitis patients. Skin Pharmacol Appl Skin Physiol. 2001; 14:234–242.

12. Merial-Kieny C, Castex-Rizzi N, Selas B, Mery S, Guerrero D. Avène Thermal Spring Water: an active component with specific properties. J Eur Acad Dermatol Venereol. 2011; 25:Suppl 1. 2–5.

13. Castex-Rizzi N, Charveron M, Merial-Kieny C. Inhibition of TNF-alpha induced-adhesion molecules by Avène Thermal Spring Water in human endothelial cells. J Eur Acad Dermatol Venereol. 2011; 25:Suppl 1. 6–11.

14. Lee JH, Jin SY, Choi YS, Kwon HB, Lee SH, Lee J, et al. Therapeutic efficacy of hot spring sea water therapy in atopic dermatitis: a pilot study. Korean J Asthma Allergy Clin Immunol. 2011; 31:124–130.
15. Choi YJ, Lee HJ, Lee DH, Woo SY, Lee KH, Yun ST, et al. Therapeutic effects and immunomodulation of Suanbo mineral water therapy in a murine model of atopic dermatitis. Ann Dermatol. 2013; 25:462–470.

16. Lee HP, Choi YJ, Cho KA, Woo SY, Yun ST, Lee JT, et al. Effect of spa spring water on cytokine expression in human keratinocyte HaCaT cells and on differentiation of CD4(+) T cells. Ann Dermatol. 2012; 24:324–336.

17. Cevikbas F, Steinhoff M. IL-33: a novel danger signal system in atopic dermatitis. J Invest Dermatol. 2012; 132:1326–1329.

18. Tamagawa-Mineoka R, Okuzawa Y, Masuda K, Katoh N. Increased serum levels of interleukin 33 in patients with atopic dermatitis. J Am Acad Dermatol. 2014; 70:882–888.

19. Nabe T. Interleukin (IL)-33: new therapeutic target for atopic diseases. J Pharmacol Sci. 2014; 126:85–91.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download