Dear Editor:
Benign lichenoid keratosis (BLK) usually presents as a solitary lesion that occurs predominantly on the trunk and upper extremities in middle-aged women. The pathogenesis of BLK is unclear; however, it has been suggested that BLK may be associated with the inflammatory stage of regressing solar lentigo (SL)1. Here, we report an interesting case of porokeratosis presenting with a BLK-like appearance.
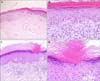
A 56-year-old female patient visited our clinic with a skin lesion on the right elbow that had appeared 3 years ago. The skin lesion was found by accident and gave no trouble to the patient except for a sense of a slowly spreading lesion. The skin lesion consisted of two relatively well-defined erythematous to dark brownish, about 20×10 mm, flat patches with a slightly elevated border on her right elbow (Fig. 1). The skin lesion histologically revealed hyperkeratosis, parakeratosis, and acanthosis with vacuolar alteration of the basal cell layer, and a dense band-like lymphocytic infiltration (Fig. 2). In addition, on another side, the epidermis also showed dermal lichenoid infiltration together with a parakeratotic column (Fig. 2). On the basis of these clinical and histological features, we diagnosed the lesions as porokeratosis presenting with a BLK-like appearance.
In 2005, Morgan et al.1 defined five different clinical and pathologic subtypes of BLK, and three-fourth of classic-type cases showed at least focal changes of lentigo especially at the periphery of the lesion, providing evidence that BLK represents a lymphocyte-mediated regression of a pre-existing lentigo. In our case, the clinicopathologic findings were close to a classic type; however, the preexisting lentigo was not remarkable and an unusual finding of cornoid lamella was found.
Disseminated superficial actinic porokeratosis (DSAP) is the most common type of porokeratosis, with multiple lesions localized predominantly on the sun-exposed surface of the limbs. Berger et al.2 suggested that actinic porokeratosis should be considered as a potential primary lesion giving rise to BLK. In addition, 61 cases of DSAP showed lichenoid infiltrate in 23 (38%) cases3. Recently, Aydingöz et al.4 reported a case of a rare presentation of BLK as a lichenoid interphase tissue response to porokeratosis.
The exact pathogenesis and causes of BLK is unclear. To date, it has been proposed that BLK represents a regressive form of preexisting epidermal tumors such as SL and seborrheic keratosis. Moreover, BLK is referred to as "sunlight-induced clonal growths of abnormal epidermal cells." together with SL, large cell acanthoma, and actinic keratosis5. As a result, we thought that BLK might be triggered by ultraviolet light and considered as a spectrum of sequential sun-exposed reactions in previous skin lesions such as porokeratosis. Regression is a phenomenon present in a variety of cutaneous lesions, and BLK has been generally considered a regressive pattern. Our case suggests that a regressive pattern of porokeratosis should be reconsidered and be included in the pathogenesis of BLK. However, it still needs to be considered that BLK might be a phenomenon resulting from dermo-epidermal changes induced by sun-exposure rather than a regressing stage of specific skin diseases.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download