INTRODUCTION
Bowen disease (BD) is a malignancy that is pathologically confined to the epidermis. Treatments for BD include topical 5-fluorouracil or imiquimod cream application, surgery, cryotherapy, and photodynamic therapy (PDT)1. Although surgery is preferred because of the low recurrence rate, it can result in hypertrophic scarring or contracture, particularly in hand lesions. Herein, we report a case of BD in the first web space of the hand treated with PDT as an alternative to surgery.
CASE REPORT
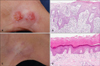
A 78-year-old man presented with an asymptomatic 2.0-cm erythematous round scaly plaque in the first web space of his right hand; the plaque had been present for 1 year. Skin biopsy revealed keratinocyte atypia throughout the epidermis. The patient was diagnosed with BD and treated with ablative fractional laser (AFXL)-assisted PDT, because he did not wish to undergo surgery. Prior to the photosensitizer application, the lesion surface was pretreated with a single pass of a fractional CO2 laser (eCO2; Lutronic Inc., Seoul, Korea) with the following parameters: pulse energy, 50 mJ; density, 100 spots/cm2; power, 30 W. Afterwards, topical methyl aminolevulinate (MAL) cream (Metvix; Galderma, Hertfordshire, UK) was applied to the pretreated lesion. An occlusive dressing was applied and maintained for 90 minutes. The lesion was then irradiated with a 630-nm light-emitting diode (AktiliteCL128; Galderma) at a light dose of 37 J/cm2. After 4 PDT treatment sessions, the lesion showed partial improvement, but the patient was subsequently lost to follow-up for 11 months. When he visited again, we noted an aggravation of the lesion, which split and formed 2 round plaques (Fig. 1A). Each lesion was biopsied, and the findings were consistent with BD (Fig. 1B). The lesions were then retreated with 9 sessions of AFXL-assisted PDT administered at 2~4-week intervals. No clinical or pathological abnormalities were noted 3 months after the last treatment (Fig. 1C, D). Furthermore, as of 9 months after the final treatment, the lesion was clinically cleared without evidence of recurrence.
DISCUSSION
AFXL-assisted PDT was designed to shorten the incubation time of conventional PDT. AFXL produces microscopic vertical holes that facilitate an acceleration of photosensitizer absorption into the lesion, thereby reducing incubation time. A randomized study on actinic keratosis indicated that AFXL-assisted PDT achieves greater photosensitizer penetration and is more effective than conventional PDT (complete response rate: 90% vs. 67%, respectively)2. Furthermore, a previous study revealed that AFXL-assisted PDT for BD with 70 minutes of incubation time has similar treatment efficacy to conventional PDT3. European guidelines recommend topical PDT for large and/or multiple BD lesions. The average clinical clearance rate of BD at 3 months after 1 or 2 MAL-PDT sessions is approximately 76%~93%1. A previous study described the successful treatment of 4 patients with BD of the digits by 5-aminolevulinic acid (ALA)-PDT4. Compared to previous studies, the present patient required a greater number of treatments for several reasons. First, Asian patients required more sessions of PDT to achieve complete remission than Caucasian patients because Asian skin, which generally contains more pigment in the epidermis, tends to more resistant to penetration than Caucasian skin3,5. Second, the study of BD treatment with ALA-PDT mentioned above involved a much higher irradiation energy (240 J/cm2 divided into 2 fractions with a 90-minute interval)4. Third, a prior study indicated that acral BD has a lower clearance rate than nonacral BD, although the difference is not significant (69% vs. 81%, respectively)6. Although the present case required multiple treatments, we believe that PDT can be an alternative treatment for BD occurring in the first web space of the hand.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download