Abstract
Folliculocystic and collagen hamartoma is a newly described complex hamartoma characterized by abundant collagen deposition, concentric perifollicular fibrosis, and keratin- filled infundibular cysts that are visible on histopathological examination. Here, we report the case of a 19-year-old Korean man who had large brownish infiltrated plaques with numerous follicular comedo-like openings and subcutaneous cystic masses on his right temporal scalp and ear since birth. Histopathological examination showed abundant collagen deposition in the dermis that extended up to the subcutaneous fat layer, multifocal infundibular cysts packed with keratin, and perifollicular inflammation and fibrosis. Hence, we describe a new type of hamartoma with folliculocystic and collagen components but without tuberous sclerosis.
Folliculocystic and collagen hamartoma is newly described as a term for a complex hamartoma characterized by thick collagen deposition, concentric perifollicular fibrosis, and a keratin-filled infundibular cyst. In 2012, Torrelo et al.1 first reported on six patients with skin lesions consisting of large, painless, infiltrated plaques that had appeared at birth and became studded with multiple follicular comedo-like openings and large keratin-containing cysts over time. On histopathological examination, they showed three main components in common: abundant collagen deposition, concentric perifollicular fibrosis, and keratin-filled infundibular cysts. The authors proposed the term "folliculocystic and collagen hamartoma" for this new type of hamartoma with folliculocystic and collagen components. Five of the six patients had a clinical diagnosis of tuberous sclerosis. Here, we report a case of folliculocystic and collagen hamartoma in a patient without tuberous sclerosis.
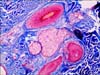
A 19-year-old Korean man visited us with large, infiltrated plaques on his right temporal scalp and soft cystic masses on the ear. The lesions had been present since birth and grew slowly over time. Dermatologic examination showed large, brownish infiltrated plaques studded with numerous follicular comedo-like openings and multiple, various-sized subcutaneous cystic masses on the right temporal scalp and ear (Fig. 1). Mature hairs were barely seen on the lesional scalp. The lesions occurred on the right temporal scalp and ear only, and no other cutaneous lesion was observed in the whole body, including the face, trunk, extremities, and oral mucosa. He had no specific history and familial history of tuberous sclerosis. Moreover, laboratorytests including complete blood count, blood chemistry analysis, and urine analysis showed no other abnormality. He underwent incisional biopsy of a subcutaneous cystic mass on his right temporal scalp under the impression of nevus sebaceous (Fig. 1). The incisional biopsy specimen showed variable-sized multifocal cysts packed with keratin and lined by an infundibular epithelium, comedones plugged with keratin, and sebum in the papillomatous epidermis. The amount and thickness of hyalinized, eosinophilic collagen bundles in the papillary dermis had increased markedly and extended into the subcutaneous fat tissues as fibrous stands. Mature sebaceous glands and hair follicles surrounded by variable concentric fibrosis were observed in the mid dermis. Concentric fibrosis as well as perifollicular fibrosis also involved the small and medium vessels (Fig. 2). Masson's trichrome staining confirmed the increased collagen bundles and the variable concentric fibrosis of hair follicles and other skin appendages (Fig. 3). These characteristic histopathologic findings were not consistent with collagen nevus, nevus sebaceous, and other well-known diseases; thus, we concluded a diagnosis of folliculocystic and collagen hamartoma, on the basis of a literature search revealing this new disease entity. After biopsy, the patient was transferred to the plastic surgery department and the remnant lesions were removed through a wide excision; the resulting defect was repaired with a local advancement flap.
Folliculocystic and collagen hamartoma was suggested as a new type of complex hamartoma related with tuberous sclerosis complex (TSC) in 2012 by Torrelo et al.1. They reported six cases of complex hamartomas showing thick collagen deposition, concentric perifollicular fibrosis, and keratin-filled infundibular cysts, and that clinically appeared as a large thickened plaque studded with multiple comedo-like openings and keratin-containing cysts. Among the six patients, five had central nervous system and/or cardiac manifestations of TSC, and had a diagnosis of TSC according to the currently accepted diagnostic criteria; therefore, it seems that the two disorders are causally related.
The typical skin findings of TSC are facial angiofibromas, periungual fibromas (Koenen's tumor), gingival fibromas, shagreen patches (plaque of collagenoma), fibrous plaque of the forehead, and ashleaf macules. Shagreen patches, a form of collagenoma associated with tuberous sclerosis, are hamartomatous proliferative lesions consisting of collagen. Histopathologically, collagenoma shows the proliferation of connective tissue due to increased collagen fibers with either normal or decreased elastic fibers2. In terms of abundant collagen deposition in the dermis of TSC, folliculocystic and collagen hamartoma might be considered an atypical type of shagreen patches3. It may show perifollicular fibrosis and microscopic pilosebaceous involvement, such as comedo-like dilatations and abnormal hair follicles in collagen nevi4. However, this new complex hamartoma involves not only collagen deposition but also hair follicle components and infundibular cyst formation. Infundibular cyst formation is not observed in shagreen patches of TSC and other TSC-unrelated collagen nevi; thus, these characteristic histopathologic features are recognized to forma distinctive hamartomatous skin lesion1.
Buschke-Ollendorff syndrome (BOS) is another form of connective tissue nevi with circumscribed hamartomatous malformation. It is an autosomal dominant disease characterized by disseminated connective tissue nevi of the elastic type, and osteopoikilosis5. Connective tissue nevi in BOS present at birth and consist of either elastin or collagen, are mostly elastomas6. The lesions are asymptomatic, firm flesh- or yellow-colored papules and nodules that may coalesce into plaques, similar to our case in clinical features. However, it involves typically the trunk and extremities. Although histological findings vary greatly, an increased number of elastic fibers or thickened collagen bundle is commonly observed. Osteopoikilosis is an asymptomatic skeletal dysplasia with osetosclerotic foci in the metaphyses and epiphyses of the long bone, pelvis, and hands7. Radiologic findings in addition to cutaneous lesions and a positive family history are helpful in diagnosing BOS; however, these are not compatible with our case.
Concerning clinical features, our case might mimic plexiform neurofibroma, nevus sebaceous, or epidermal nevus occurring on the scalp. The plexiform variant of neurofibroma, considered to be pathognomonic of neurofibromatosis type 1 (NF1), is usually present at birth as a noncircumscribed baggy, thick, irregular, and pedunculated dermal and subcutaneous tumor, and may result in significant disfigurement and dysfunction8. It involves single or multiple nerve fascicles that often arise from the branches of major nerves and form a mass of tangled, rope-like structures9. It became apparent during the first year of life in 30% of patients with NF19. However, our case didnot have any other features of NF1, including café-au-lait spots, axillary freckling, cutaneous neurofibroma, neurologic abnormalities, and histologic features.
Nevus sebaceous is a complex cutaneous hamartoma involving the pilosebaceous follicle and often other adnexal structures. Clinically, it appears as a yellowish verrucous plaque usually on the scalp or forehead. It may appear at birth or develop during childhood as smooth, yellowish, hairless patches, and change into elevated verrucous plaque during puberty1011. On histopathology, the epidermis shows acanthosis and papillomatosis, and sebaceous gland hyperplasia; immature hair follicles are observed in the dermis12. The appearance of immature hair follicles may be a feature of diagnostic importance in nevus sebaceous. However, mature hair follicles surrounded by variable concentric fibrosis with perifollicular inflammation and infundibular cyst are key components of this new complex hamartoma.
The precise pathogenesis and mechanism are unknown, although it is supposed to be related to tuberous sclerosis. However, in our case, the patient had no history of extracutaneous manifestations such as skeletal abnormality, neurologic defects, and ocular disorders, and had no familial history. After excision, neither recurrence nor newly developed lesions have been reported, thus we concluded that the disease occurred without tuberous sclerosis. To the best of our knowledge, there has been no previous report like our case in Korea. We demonstrated a new type of hamartoma with folliculocystic and collagen components in a patient without tuberous sclerosis. Here, we call it folliculocystic and collagen hamartoma.
Figures and Tables
 | Fig. 1Brownish infiltrated plaques with numerous follicular comedo--like opening and subcutaneous cystic masses on the right temporal scalp and ear. |
 | Fig. 2(A) Variable-sized multifocal infundibular cysts packed with keratin and comedones (×40). (B) Abundant, thick, eosinophilic collagen deposition in the dermis extending into the subcutaneous fat layer as fibrous strands (×40). (C) Perifollicular concentric fibrosis (×100). (D) Concentric fibrosis also involved some small and medium vessels in the surrounding tissue (×100). A~D: H&E. |
References
1. Torrelo A, Hadj-Rabia S, Colmenero I, Piston R, Sybert VP, Hilari-Carbonell H, et al. Folliculocystic and collagen hamartoma of tuberous sclerosis complex. J Am Acad Dermatol. 2012; 66:617–621.

2. Uitto J, Santa Cruz DJ, Eisen AZ. Connective tissue nevi of the skin. Clinical, genetic, and histopathologic classification of hamartomas of the collagen, elastin, and proteoglycan type. J Am Acad Dermatol. 1980; 3:441–461.
3. Wataya-Kaneda M, Tanaka M, Hamasaki T, Katayama I. Trends in the prevalence of tuberous sclerosis complex manifestations: an epidemiological study of 166 Japanese patients. PLoS One. 2013; 8:e63910.

4. Nickel WR, Reed WB. Tuberous sclerosis. Special reference to the microscopic alterations in the cutaneous hamartomas. Arch Dermatol. 1962; 85:209–226.
5. Morrison JG, Jones EW, MacDonald DM. Juvenile elastoma and osteopoikilosis (the Buschke--Ollendorff syndrome). Br J Dermatol. 1977; 97:417–422.

6. Umaretiya PJ, Miest RY, Tollefson MM. A 5-year-old with connective tissue nevi: Buschke-Ollendorff syndrome. J Pediatr. 2014; 165:206.

7. Surrenti T, Callea F, De Horatio LT, Diociaiuti A, El Hachem M. Buschke-Ollendorff syndrome: sparing unnecessary investigations. Cutis. 2014; 94:97–100.
9. Ward BA, Gutmann DH. Neurofibromatosis 1: from lab bench to clinic. Pediatr Neurol. 2005; 32:221–228.

10. Kantrow SM, Ivan D, Williams MD, Prieto VG, Lazar AJ. Metastasizing adenocarcinoma and multiple neoplastic proliferations arising in a nevus sebaceus. Am J Dermatopathol. 2007; 29:462–466.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download