Abstract
Background
The oral mucosa is constantly exposed to several irritants and allergens including dental materials, but the role of contact allergy in oral disease is obscure.
Objective
To analyze positive patch test results in patients with oral diseases and evaluate the clinical relevance of oral diseases with contact allergy to dental materials.
Methods
We retrospectively analyzed patch test results with dental screening series in 44 patients with oral disease from 2004~2011.
Results
Oral diseases included oral lichen planus (54.5%), cheilitis (27.3%), burning mouth syndrome (9.1%), and others (9.1%). Thirty-one of 44 patients (70.5%) had positive reactions to one or more allergens. The most commonly detected allergens were gold sodium thiosulfate (25.0%) and nickel sulfate (25.0%), followed by potassium dichromate (22.7%), cobalt (15.9%), palladium (6.8%), mercury (4.5%), copper (4.5%), and methylhydroquinone (4.5%). Six of 24 patients with oral lichen planus had a symptom in areas adjacent to dental materials and positive patch test reactions to allergens contained in the suspected dental materials.
The oral mucosa including the lips is constantly exposed to several irritants and allergens. In particular, dental materials including antiseptics, metals, impression materials, local anesthetics, ultraviolet radiation, cements, latex gloves, rubber dams, acrylics, adhesives, mouthwashes, and other dental hygiene materials may provoke oral disease. The role of contact allergy to dental materials in oral disease has not fully been elucidated, and the usefulness of the patch test in oral disease remains unclear12. Gawkrodger3 report that patch testing for delayed-type hypersensitivity and tests for immediate-type allergies are useful methods for evaluating patients who present with oral or facial symptoms possibly related to dental procedures as well as dental personnel who present with chronic hand or facial dermatitis. Some studies about patch tests in oral diseases report that metal contained in dental materials, such as nickel and gold, is clinically related with oral symptoms456. However, there is no report about contact allergy to dental metals in patients with oral disease in Korea. Therefore, this study analyzed positive patch test reactions with dental screening series and evaluated the clinical relevance of oral diseases with contact allergy to dental materials.
This study was based on patch test results from February 2004 to February 2011. All patients underwent patch tests with dental screening series. We also recorded age, sex, clinical symptoms, lesion sites, occupation, and history of allergic disease.
Dental screening series were supplied by Chemotechnique Diagnostics (Tygelsjö, Sweden). All allergens were applied with Finn Chambers (Epitest Ltd. Oy, Tuusula, Finland) and Scanpor tape (NorgesplasterAlpharma AS, Vennesla, Norway) on the upper back. The strips were removed after 48 hours. Readings were performed at 48 and 96 hours, and reactions were graded according to the standard scoring system7. This study was given an exemption for ethical approval from the institutional review board of Pusan National University Hospital (IRB No. E-2013088).
Forty-four patients were included, including 27 women and 17 men with a mean age of 51.6 years (range: 20~71 years). None of them had an atopic history or history of allergies for specific materials such as gold and nickel. The most common oral disease was oral lichen planus (n=24, 54.5%), followed by cheilitis (n=12, 27.3%), burning mouth syndrome (n=4, 9.1%), and others (n=4, 9.1%) such as recurrent aphthosis, glossodynia, stomatitis, and perioral dermatitis.
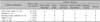
Thirty-one of 44 patients (70.5%) had a positive reaction to one or more allergens. The most common allergens were gold sodium thiosulfate (25.0%) and nickel sulfate (25.0%), followed by potassium dichromate (22.7%), cobalt (15.9%), palladium (6.8%), mercury (4.5%), copper (4.5%), and methylhydroquinone (4.5%) (Fig. 1). The common allergens with respect to each oral disease are listed in Table 1. Thirteen patients (29.5%) had multiple positive reactions; frequent combinations of allergens were gold/nickel (n=6, 46.2%), cobalt/nickel (n=4, 30.8%), and palladium/nickel (n=3, 23.1%).
Sixteen of 24 (66.7%) patients with oral lichen planus had a history of dental procedures, and 12 patients had a positive patch test reaction to one or more allergen. Potassium dichromate (58.3%), gold sodium thiosulfate (41.6%), and nickel sulfate (41.6%) were the most frequent allergens. Five of 12 (41.7%) patients with cheilitis had a history of dental procedures, and 4 patients had a positive patch test reaction. The most common allergens were cobalt (50.0%), gold sodium thiosulfate (25.0%), potassium dichromate (25.0%), and mercury (25.0%).
Clinical relevance was defined as the presentation of oral symptoms in an area adjacent to dental filling or alloys and a positive patch test reaction to allergens contained in those dental materials8. Six of 12 patients with oral lichen planus had a history of dental procedures and a positive patch test reaction to one or more allergens exhibited clinical relevance with contact allergy to dental materials. Nickel sulfate (83.3%), gold sodium thiosulfate (66.7%), and potassium dichromate (66.7%) were the most common allergens. One patient with oral lichen planus had clinical relevance with contact allergy to dental materials, and their oral manifestation improved after changing the dental fillings. Patients with oral diseases besides lichen planus had no clinical relevance with positive patch test reactions.
Dental restorative materials include dental alloys, amalgam, and tooth-colored fillings9. Dental alloys are divided into noble and base metal alloys. Noble metals used for dental castings include alloys of gold, palladium, and silver (not a noble metal), with smaller amounts of iridium, ruthenium, and platinum10. Meanwhile, the base metal alloy systems most commonly used in dentistry include stainless steels, nickel-chromium, cobalt-chromium, titanium, and nickel-titanium alloys11. Amalgam is metallic filling material comprising a mixture of mercury and powdered alloy mostly made of silver, tin, zinc, and copper. Tooth-colored filling includes composite resin (bisphenol A-glycidyl methacrylate and urethane dimethacrylate), glass ionomer cement, and porcelain (i.e., ceramic). Dental screening series cover most components of dental restorative materials (Table 2).
This present study evaluated a heterogeneous group of patients with oral disease to clarify the role of contact allergy to dental materials. The most common oral diseases in the present study were oral lichen planus, cheilitis, and burning mouth syndrome. The overall positive patch test reaction rate was 70.5%. Raap et al.9 retrospectively analyzed 206 patients who underwent patch testing with metals used in dentistry and report a 13.6% (28/206) positive reaction rate. Meanwhile, Khamaysi et al.8 report a positive reaction rate of 40.5% (49/121). Thus, the positive patch test reaction rate is higher in the present study than previous studies. This result is probably due to the small number of patients and higher prevalence of oral lichen planus.
The most common allergic contact reactions were to gold sodium thiosulfate, nickel sulfate, and potassium dichromate, similar to previous reports; however, the number of positive patch test results with potassium dichromate was higher in the present study89. Multiple positive patch test reactions were not uncommon in the present study possibly because of cross-reactions such as that between nickel and palladium; accordingly, dental alloys comprise several metals10.
Several studies demonstrate an association between oral lichen planus and contact allergy to mercury, the main component of amalgam fillings1112. Dunsche et al.13 report that 27.7% of 134 patients with oral lichenoid lesion showed positive patch test results to inorganic mercury or amalgam, and amalgam removal led to improvement in 97.1% of patients. However, no patients with oral lichen planus tested positive for mercury allergy in the present study. This might be because of the use of amalgam as a restorative material has decreased in Korea in conjunction with several studies demonstrating its hazards1415. Other common allergens in the present study were gold sodium sulfate, nickel sulfate, and potassium dichromate. This may be associated with the increasing demand by dental patients for precious metal alloys and tooth-colored restoration rather than amalgam. Ahlgren et al.16 report that the frequency of contact allergy to gold was 28.9% in 96 patients with oral lichenoid lesions and suggest that dental gold may be one of several etiological factors for the development or maintenance of oral lichenoid lesions. The present results also indicate gold and nickel are important allergens that have significant relevance in oral lichen planus. Scalf et al.17 report that 49.0% of 51 patients with oral, cutaneous, and genital lichenoid reactions had positive patch test reactions with at least 1 mercurial allergen. Chromate, gold, and thimerosal exhibited significantly higher positive patch test reactions, and 100% reported improvement after metal replacement. They conclude sensitization to dental metals is more common in patients with lichenoid reactions and might be an etiologic or triggering factor. These findings demonstrate the value of the patch test with dental screening series.
Cheilitis usually involves many allergens such as medicaments, lipsticks, sunscreens, and tooth pastes, making it particularly difficult to investigate relevant allergens18. In the present study, 9 of 12 patients with cheilitis had positive patch test reactions with dental metals. This result suggests there is low clinical relevance of contact allergy to dental materials or that dental materials may induce cheilitis. Inoue19 report that palladium is unstable in the oral cavity, releasing metal content into the saliva, which could cause a serious allergic reaction. Thus, constant contact of solubilized dental alloys in saliva could result in contact cheilitis.
It was recently shown that patients with burning mouth syndrome have clinically relevant contact allergies to gold and nickel20. The authors speculate that tiny amounts of nickel and gold in dental metals caused the symptoms of burning mouth syndrome. Accordingly, after replacing the dental metals, the patients recovered quickly. However, in the present study, no patients with burning mouth syndrome had positive patch test reactions with dental metals.
The limitations of this study include its small sample size and skewed incidence of relevant allergens. Therefore, large-scale clinical trials involving patients with oral diseases including oral lichen planus as well as data on the clinical progression of patients with oral diseases after changing dental materials are warranted to validate the use of patch testing in oral diseases.
In summary, the association between oral disease and contact allergy to dental materials remains obscure because of the small number of patients in this study. However, patients with oral lichen planus exhibited clinical significance with contact allergy to dental metals. Therefore, the patch test with dental screening series is recommended for investigating the relevance of contact allergy to dental materials in patients with oral disease, especially oral lichen planus, who have a history of dental procedures.
References
1. De Rossi SS, Greenberg MS. Intraoral contact allergy: a literature review and case reports. J Am Dent Assoc. 1998; 129:1435–1441.

2. Eisen D, Eisenberg E. Oral lichen planus and the burning mouth syndrome. Is there a role for patch testing? Am J Contact Dermat. 2000; 11:111–114.

4. Van Hoogstraten IM, Andersen KE, Von Blomberg BM, Boden D, Bruynzeel DP, Burrows D, et al. Reduced frequency of nickel allergy upon oral nickel contact at an early age. Clin Exp Immunol. 1991; 85:441–445.

5. Laeijendecker R, van Joost T. Oral manifestations of gold allergy. J Am Acad Dermatol. 1994; 30:205–209.

6. Ditrichova D, Kapralova S, Tichy M, Ticha V, Dobesova J, Justova E, et al. Oral lichenoid lesions and allergy to dental materials. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2007; 151:333–339.

7. Lee EK, Lee JY, Kim HO. A study of as is patch test in cosmetic contact dermatitis. Ann Dermatol. 1999; 11:207–213.

8. Khamaysi Z, Bergman R, Weltfriend S. Positive patch test reactions to allergens of the dental series and the relation to the clinical presentations. Contact Dermatitis. 2006; 55:216–218.

9. Raap U, Stiesch M, Reh H, Kapp A, Werfel T. Investigation of contact allergy to dental metals in 206 patients. Contact Dermatitis. 2009; 60:339–343.

10. Watsky KL. Occupational allergic contact dermatitis to platinum, palladium, and gold. Contact Dermatitis. 2007; 57:382–383.

11. Laine J, Kalimo K, Happonen RP. Contact allergy to dental restorative materials in patients with oral lichenoid lesions. Contact Dermatitis. 1997; 36:141–146.

12. Wong L, Freeman S. Oral lichenoid lesions (OLL) and mercury in amalgam fillings. Contact Dermatitis. 2003; 48:74–79.

13. Dunsche A, Kästel I, Terheyden H, Springer IN, Christophers E, Brasch J. Oral lichenoid reactions associated with amalgam: improvement after amalgam removal. Br J Dermatol. 2003; 148:70–76.

14. Choi EJ, Jung TR, Kim CC, Kim YJ. The changes in practice pattern and patient distribution for last 5 years (2000-2005) in the department of pediatric dentistry at Seoul National University dental hospital. J Korean Acad Pediatr Dent. 2006; 33:673–677.
15. Mutter J, Naumann J, Walach H, Daschner F. Amalgam risk assessment with coverage of references up to 2005. Gesundheitswesen. 2005; 67:204–216.
16. Ahlgren C, Bruze M, Möller H, Gruvberger B, Axéll T, Liedholm R, et al. Contact allergy to gold in patients with oral lichen lesions. Acta Derm Venereol. 2012; 92:138–143.

17. Scalf LA, Fowler JF Jr, Morgan KW, Looney SW. Dental metal allergy in patients with oral, cutaneous, and genital lichenoid reactions. Am J Contact Dermat. 2001; 12:146–150.

18. Freeman S, Stephens R. Cheilitis: analysis of 75 cases referred to a contact dermatitis clinic. Am J Contact Dermat. 1999; 10:198–200.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download