Abstract
Nuchal-type fibroma is a rare, benign, fibrous, tumor-like proliferation characterized by dense hypocellular bundles of collagen, with sparsely scattered fibroblasts, interspersed fat tissue, and entrapped nerve fibers. It usually develops in the posterior neck as a solitary, firm, poorly circumscribed, subcutaneous mass. Herein, we report about a 32-year-old man who presented with a 6-year history of multiple nodules on the scalp. Histopathological features were consistent with those of nuchal-type fibroma. The tumors were surgically excised.
A nuchal-type fibroma (NTF) is a rare, benign, fibrous, tumor-like proliferation of unknown pathogenesis1. An NTF is characterized by dense hypocellular bundles of collagen interspersed with fat tissue, entrapped adnexal structures, and peripheral nerve fibers2. NTFs usually develop as solitary, hard, poorly circumscribed, subcutaneous masses in the posterior aspect of the neck3. However, approximately one-third of all cases occur at other sites. Most extranuchal tumors arise in the back, scapular region, shoulder, and face, but cases have been reported to occur in other parts of the body, including the axilla, forearm, trunk, anterior neck, knee, ankle, and scalp4,5. NTFs present as single lesions in most cases; only a few cases involving multiple lesions have been reported6. Herein, we report an unusual case of NTF that arose in the scalp, an uncommon extranuchal site, and presented as 6 distinct lesions.
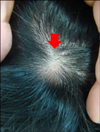
A 32-year-old man presented to our department with a 6-year history of multiple nodules on the scalp. The patient had experienced intermittent pain and an itching sensation on the lesions. On physical examination, 6 protruding, subcutaneous, firm nodules of varying size were observed on the scalp (Fig. 1). The nodules were several centimeters in size. An earlier ultrasonographic examination at a different hospital had indicated that the lesions could be suspected lipomas. For a further diagnosis, an excisional biopsy was performed for a single lesion. Histopathological examination revealed a poorly circumscribed, paucicellular lesion composed of thick, haphazardly arranged collagen fibers with sparsely scattered fibroblast-like cells in the subcutis (Fig. 2A, B). Adipose tissue islands and peripheral nerve fibers were entrapped by the collagen fibers (Fig. 2C, D). These findings were consistent with those of NTF. The other lesions were also excised, and they displayed the same histopathological features.
Nuchal fibromas are rare, benign, fibrous tumors, first described in 1988 by Enzinger and Weiss7. Nuchal fibromas characteristically present as asymptomatic, firm, poorly circumscribed, subcutaneous masses that generally develop in the posterior neck8. Histopathologically, nuchal fibromas are composed of thick, haphazardly arranged collagen fibers, with sparsely scattered fibroblasts. The entrapment of adnexal structures, adipose tissue, and peripheral nerve fibers by the collagen bundles is a notable histologic feature9. Nuchal fibromas typically develop in the nuchal region, but in approximately one-third of the cases, it occurs at extranuchal sites. The extranuchal lesions are morphologically and histologically indistinguishable from those of the nuchal region; therefore, in 1999, Michal et al.2 proposed the term 'nuchal-type fibroma' to encompass all lesions histologically similar to nuchal fibroma, irrespective of their site of origin. The most common extranuchal sites of NTF are the back (particularly the interscapular region), shoulder, and face. In addition, cases have been reported to occur in other parts of the body including the axilla, forearm, trunk, anterior neck, knee, ankle, and scalp4.
In most cases, NTF presents as a single lesion. However, 3 cases with 2 distinct lesions have been described6. Recently, a case of NTF presenting as multiple lesions on the posterior neck and upper back was also reported10.
The pathogenesis of NTF remains unknown, but some cases of NTF have been associated with trauma2, diabetes mellitus11 and Gardner syndrome12,13. When NTF occurs at multiple sites or unusual locations, the possibility of a Gardner-associated fibroma prior to NTF should be considered14. However, our patient had neither diabetes mellitus nor Gardner syndrome.
Wide surgical excision is the most acceptable treatment for NTF10. However, the unencapsulated nature of NTF lesions15 makes complete excision difficult, potentially contributing to their propensity for local recurrence. Alternatively, recurrence could be owing to the persistent presence of factors that triggered the initial development of the NTF lesion, including repetitive trauma16.
Many cases of NTF have been misdiagnosed because of its indolent clinical course and histopathological similarity to other benign fibrous tumors15. NTF needs to be distinguished from other fibrous tumors and tumor-like conditions, including desmoid-type fibromatosis; circumscribed storiform collagenoma; connective tissue nevus; collagenous fibroma; fibroma of the tendon sheath; scleredema; and scar tissue. NTF differs from theses tumors by its marked hypocellularity, poor circumscription, and presence of entrapped adipose tissue4.
The case described here was a rare NTF that presented as multiple lesions on the scalp, an uncommon extranuchal site.
Figures and Tables
 | Fig. 2(A) Infiltration of poorly circumscribed, dense, collagen bundles in the subcutis. (B) Fibroblast-like cells are sparsely interspersed between the collagen fibers. (C, D) Adipose tissue islands and peripheral nerve fibers were entrapped by the collagen fibers (H&E; A: ×10, B: ×400, C: ×40, D: ×200). |
References
1. Abe M, Nagai Y, Okada E, Aoyama K, Tamura A, Ishikawa O. Case of nuchal fibroma. J Dermatol. 2007; 34:498–500.

2. Michal M, Fetsch JF, Hes O, Miettinen M. Nuchal-type fibroma: a clinicopathologic study of 52 cases. Cancer. 1999; 85:156–163.
3. Kang TW, Lee SE, Kim SC. A case of nuchal fibroma. Korean J Dermatol. 2007; 45:168–170.
5. Balachandran K, Allen PW, MacCormac LB. Nuchal fibroma. A clinicopathological study of nine cases. Am J Surg Pathol. 1995; 19:313–317.
6. Lee SE, Kim YC, Kim SC. Nuchal fibroma presenting as two posterior neck masses. J Dermatol. 2007; 34:262–263.

7. Enzinger FM, Weiss SW. Benign tumors and tumorlike lesions of fibrous tissue. In : Enzinger FM, Weiss SW, editors. Soft tissue tumors. 2nd ed. St. Louis: Mosby;1988. p. 102–135.
8. Abraham Z, Rozenbaum M, Rosner I, Naschitz Y, Boss Y, Rosenmann E. Nuchal fibroma. J Dermatol. 1997; 24:262–265.

9. Linos K, Sedivcová M, Cerna K, Sima R, Kazakov DV, Nazeer T, et al. Extra nuchal-type fibroma associated with elastosis, traumatic neuroma, a rare APC gene missense mutation, and a very rare MUTYH gene polymorphism: a case report and review of the literature. J Cutan Pathol. 2011; 38:911–918.

10. LeBlanc KG Jr, Wenner M, Davis LS. Multiple nuchal fibromas in a 2-year-old without Gardner syndrome. Pediatr Dermatol. 2011; 28:695–696.

11. Banney LA, Weedon D, Muir JB. Nuchal fibroma associated with scleredema, diabetes mellitus and organic solvent exposure. Australas J Dermatol. 2000; 41:39–41.

12. Diwan AH, Graves ED, King JA, Horenstein MG. Nuchal-type fibroma in two related patients with Gardner's syndrome. Am J Surg Pathol. 2000; 24:1563–1567.

13. Dawes LC, La Hei ER, Tobias V, Kern I, Stening W. Nuchal fibroma should be recognized as a new extracolonic manifestation of Gardner-variant familial adenomatous polyposis. Aust N Z J Surg. 2000; 70:824–826.

14. Wehrli BM, Weiss SW, Yandow S, Coffin CM. Gardnerassociated fibromas (GAF) in young patients: a distinct fibrous lesion that identifies unsuspected Gardner syndrome and risk for fibromatosis. Am J Surg Pathol. 2001; 25:645–651.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download