Abstract
Background
Dermatofibroma (DF) comprises a heterogeneous group of mesenchymal tumors, with fibroblastic and histiocytic elements present in varying proportions. The cell of origin of DF has been investigated, but remains unclear.
Objective
The present study attempted to investigate the expression of leukocyte-specific protein 1 (LSP1), a marker of fibrocytes, in DF. Additionally, we evaluated the effectiveness of LSP1 in the differential diagnosis of DF from dermatofibrosarcoma protuberans (DFSP).
Methods
Immunohistochemical staining was performed on 20 cases of DF using antibodies against LSP1, CD68, and factor XIIIa (FXIIIa). In addition, the expression of LSP1 and FXIIIa was evaluated in 20 cases of DFSP.
Results
Eighteen of 20 cases (90%) of DF stained positive for LSP1, with variation in the intensity of expression. CD68 was positive in 10 cases (50%), and FXIIIa was expressed in all cases of DF. There were differences between the regional expression patterns of the three markers in individual tumors. In contrast, only 2 of 20 cases of DFSP expressed LSP1, and none of DFSP cases stained positive for FXIIIa.
Conclusion
The LSP1-positive cells in DF could potentially be fibrocyte-like cells. FXIIIa and CD68 expression suggests that dermal dendritic cells and histiocytes are constituent cells of DF. It is known that fibrocytes, dermal dendritic cells and histiocytes are all derived from CD14+ monocytes. Therefore, we suggest that DF may originate from CD14+ monocytes. Additionally, the LSP1 immunohistochemical stain could be useful in distinguishing between DF and DFSP.
Dermatofibroma (DF) is a common skin tumor, predominantly occurring on the extremities or trunk of a young adult. Histopathologically, DF is characterized by the presence of different cell types in varying proportions, including fibroblastic cells, histiocytic cells, and even multinucleated giant cells1. In some instances, the tumor may take on a pattern resembling that of dermatofibrosarcoma protuberans (DFSP). Therefore, based on the clinical presentation and routine hematoxylin and eosin-stained sections, the differential diagnosis of DF versus DFSP can be problematic2. A large number of ancillary laboratory techniques have been investigated as potential aids in this differential diagnosis. In the previous and present studies, the combined immunohistochemical results of CD34 and factor XIIIa (FXIIIa) were found to be reliable, but the diagnostic value of this combination is still not considered absolute3,4.
There is also considerable controversy regarding the cell of origin of DF. A number of previous studies showed that DF lesions originate from fibroblasts, whereas others pointed to an origin from histiocytes, perivascular cells, or primitive mesenchymal cells5. Recently, it was suggested that dermal dendritic cells play an important role in the histogenesis of DF6.
Fibrocytes are a recently identified cell population that represent 0.1%~0.5% of peripheral blood leukocytes. Fibrocyte biology has been implicated in wound healing and in many aberrant fibrosis diseases states, including hypertrophic scarring and keloids; airway remodeling in asthma; interstitial pulmonary fibroses; systemic fibroses; atherosclerosis; and the stromal response to tumor invasion7. We postulated that fibrocytes might be associated with DF because they are derived from CD14+ monocyte as dermal dendritic cells8 and histiocytes are. However, there has been no study of the association between fibrocytes and DF to date.
The present study attempted to determine the expression of leukocyte-specific protein 1 (LSP1), a fibrocyte marker9, in DF. Additionally, we evaluated the usefulness of LSP1 in the differential diagnosis of DF from DFSP.
Formalin-fixed, paraffin-embedded (FFPE) blocks from 20 cases of DF and 20 cases of DFSP were obtained from biopsy records in two university hospitals in Korea. Cases were selected based on the original diagnosis, and hematoxylin and eosin-stained sections were reviewed to confirm these findings.
Immunohistochemical staining was performed on FFPE tissue sections from each DF and DFSP case using antibodies against LSP1 and FXIIIa. Additionally, to evaluate the immunophenotypes of the constituent cells in DF, we performed immunohistochemistry with a CD68 antibody. Four-micron-thick sections were obtained from FFPE tissues, transferred onto adhesive slides, and dried at 60℃ for 25 min. The immunohistochemical procedures were performed using a BOND-MAX automatic immunohistochemical staining instrument (Leica Biosystems, Wetzlar, Germany). In brief, following deparaffinization and rehydration of the tissue sections, antigen retrieval was carried out; endogenous peroxidase was blocked; and the slides were then incubated for 15 min at room temperature with primary antibodies against LSP1 (mouse monoclonal antibody 16/LSP-1, 1 : 250; BD Transduction Laboratories, San Jose, CA, USA), FXIIIa (mouse monoclonal antibody E980.1, 1 : 100; Novocastra, Newcastle, United Kingdom), and CD68 (mouse monoclonal antibody PG-M1, 1 : 500; DAKO, Glostrup, Denmark). Thereafter, sections were incubated with a polymer detection kit. Diaminobenzidine was used as a chromogen, and the sections were counterstained with hematoxylin.
Semiquantification of positive cells was based on the average cell number of 10 high-power fields per section, using a ×10 eyepiece and ×10 objective lens. Scores were assigned as follows: 0, <5% positive cells; 1+, 6%~33% positive cells; 2+, 34%~66% positive cells; and 3+, >67% positive cells. Statistical analysis was performed using IBM SPSS Statistics 20.0 (IBM Co., Armonk, NY, USA). The chi-squared test was performed to determine a significant difference in the expressions of LSP1 and FXIIIa among the cases of DF and DFSP. A value of p<0.05 was considered statistically significant.
There were 20 cases of DF, comprising 12 female and 8 male patients, with an average age of 34.3 years (range, 20~79 years). In addition, there were 20 cases of DFSP, comprising 4 female and 16 male patients, with an average age of 37.2 years (range, 14~60 years). The results of the immunohistochemical studies with antibodies for LSP1, FXIIIa, and CD68 are summarized in Table 1 and displayed in Fig. 1, 2, 3. Most cases of DF can be divided into cellular lesions composed of a significant number of histiocytic cells and fibrous lesions composed almost entirely of fibroblastic cells and collagen fibers. The proportion of these cells varied between the tumors. Four of the 20 cases of DF in the current study contained numerous histiocytic cells.
Furthermore, 18 cases (90%) of DF expressed LSP1. In comparison, 10 cases (50%) expressed CD68, and all cases showed expression of FXIIIa. There was some variation in the expression of the three proteins between the lesions of individual DF cases. Expression of LSP1 was observed in both cellular lesions, composed of significant numbers of histiocytic cells, and fibrous lesions, composed of fibroblastic cells and collagen fibers (Fig. 1A, B). In comparison, the expression of CD68 was observed mainly in cellular lesions (Fig. 1E, F). Staining results for LSP1 and CD68 were strong in the cellular lesions, but the number of LSP1-positive cells was greater than the number of CD68-positive cells in the same lesions. Furthermore, some cases of DF showed expression of LSP1, but not CD68. FXIIIa was strongly expressed in both cellular lesions and fibrous lesions of DF (Fig. 1C, D), but the expression showed a different pattern from that observed for LSP1 expression (Fig. 2A, B). In the normal dermis, FXIIIa-positive cells could be observed, whereas LSP1-positive cells could be detected only in a few lymphocytes (Fig. 2C, D).
In 18 of 20 cases of DFSP, the tumor cells were negative for LSP1 (Fig. 3). Two of the DFSP cases showed weakly positive (1+) LSP1 staining. The preferential staining for LSP1 in DF compared to DFSP was statistically significant (p<0.01). None of the DFSP cases (0%) stained positive for FXIIIa. The preferential staining for FXIIIa in DF compared to DFSP was also statistically significant (p<0.01).
The term fibrocyte was first used in 1994 to define a subpopulation of leukocytes that accumulate at sites of tissue injury and show fibroblast-like properties10. They were found to circulate as a subpopulation of peripheral blood monocytes and were shown to be capable of entering wound chambers implanted in the subcutaneous tissue. Recently, more attention has focused upon the study of human fibrocytes and the potential role of fibrocyte abnormalities in diseases such as systemic fibrosis, atherosclerosis, airway remodeling in asthma, interstitial pulmonary fibrosis, stromal response to tumor invasion, hypertrophic scarring, and keloid formation7. However, the exact role fibrocytes play in tissue regeneration, or how they might participate in the formation of fibrosis, is still uncertain.
Phenotypic examination of fibrocytes reveals a unique cytokine and chemokine profile distinct from that of fibroblasts, T- and B-lymphocytes, monocytes, epithelial cells, endothelial cells, and dendritic cells11. Fibrocytes in peripheral blood coexpress hematopoietic stem cell antigens, markers of the monocyte lineage and fibroblast products. That is to say, they are found to express the hematopoietic stem cell/progenitor marker CD34, the leukocyte common antigen CD45 (a pan-hematopoietic marker) and several markers of the monocyte lineage, in addition to vimentin and collagens. However, it has been reported that fibrocytes infiltrate injured target tissues undergoing remodeling and, in doing so, they appear to lose their surface expression of progenitor markers7. Recently, LSP1 was identified as a fibrocyte marker9. LSP1 is an F-actin-binding protein and a substrate of p38 mitogen-activated protein kinase and protein kinase C. It has been reported to be important in leukocyte migration and chemotaxis12.
The present study demonstrated the presence of LSP1-positive cells in DF. FXIIIa-positive dermal dendritic cells located in normal dermis did not express LSP1, and within a single specimen the degree of expression of FXIIIa was different from that of LSP1. These findings suggested that LSP1 and FXIIIa were expressed respectively in different cells. In terms of CD68 expression, CD68-positive cells were found mainly in histocytic lesions, whereas LSP1-positive cells were scattered in both fibrous lesions and histiocytic lesions. This showed that CD68 also exhibited a different expression pattern to LSP1. As already known, FXIIIa and CD68 are differentially expressed in DF. As known previously FXIIIa-positive cells and CD68-positive cells exhibit characteristics of dermal dendritic cells and histiocytes respectively5,12. Therefore, our study suggests that LSP1-positive cells exhibit the characteristics of fibrocytes.
In previous reports, the cell of origin in DF was identified as the dermal dendritic cell based on the following evidence: (i) the majority of DF cellular components are reactive with anti-FXIIIa antibody, similar to the dermal dendritic cells in normal skin6, and (ii) cellular components of DF and dermal dendritic cells express HLA-DR antigen13 and several co-stimulatory molecules such as CD80 and CD8614. Recently, Aiba and Tagami8 reported that, in a dose-dependent fashion, phorbol 12-myristate 13-acetate can transform monocyte-derived dermal dendritic cells into cell types that are characteristically observed in DF, such as fibroblastic cells, histiocytic cells, and multinucleated giant cells. The expression of CD68 suggests that histiocytes are constituent cells of DF. Fibrocytes, dermal dendritic cells, and histiocytes are all known to be derived from CD14+ monocytes. Therefore, we suggest that DF could originate from CD14+ monocytes.
The 47-kDa heat-shock protein (HSP47) is a collagen-specific molecular chaperone localized in the endoplasmic reticulum. It plays an essential role in collagen biosynthesis in skin fibroblasts15. Kuroda and Tajima5 reported that HSP47-positive skin fibroblasts were major constituent cells in DF. Transforming growth factor-β1 (TGF-β), which plays an important role in fibrosis, was found to accelerate fibrocyte differentiation into cells that are phenotypically similar to mature fibroblasts7. Interestingly, diffuse expression of TGF-β and increased expression of TGF-β-RI and TGF-β-RII were shown in DF16. Therefore, we think that fibrocytes are a potential source of HSP47-positive skin fibroblasts observed in DF.
The distinction between DF and DFSP may be very difficult in some cases because of the close clinical and histopathological similarities between these two lesions. Traditionally, CD34 and FXIIIa have been widely used to distinguish between these two conditions. However, according to several previous reports, CD34 is expressed in approximately 80% of DFSP cases and in approximately 20% of DF, while FXIIIa is detected in 80% of DF and 20% of DFSP4. For these reasons, a more precise marker for the differential diagnosis of DF and DFSP is needed. Additional or alternative markers such as stromelysin-317, tenascin18, CD16319, and TGF-β16 have been studied to help distinguish between these two lesions. In the present study, we found that 18 out of 20 cases (90%) of DF, and 2 out of 20 cases of DFSP, stained positive for LSP1. The preferential LSP1 staining in DF compared to DFSP was statistically significant.
In summary, LSP1 was expressed in DF. We suggest that LSP1-positive cells are fibrocyte-like cells. It is possible that DF originates from CD14+ monocytes, which can differentiate into dermal dendritic cells, histiocytes, and fibrocytes. The degree of LSP1 expression was significantly different between DF and DFSP; therefore, an immunohistochemical stain for LSP1 may be useful in distinguishing between these tumors.
Figures and Tables
 | Fig. 1Histological sections of dermatofibroma stained with antibodies against (A, B) leukocyte-specific protein 1 (LSP1), (C, D) factor XIIIa (FXIIIa), and (E, F) CD68. Expression of LSP1 and FXIIIa was observed in both (A, C) cellular lesions and (B, D) fibrous lesions. In contrast, immunoreactivity of CD68 was stronger in (E) cellular lesions than (F) fibrous lesions (A~F: ×200). |
 | Fig. 2Histological sections of dermatofibroma and normal skin stained with antibodies to (A, C) factor XIIIa (FXIIIa) and (B, D) leukocyte-specific protein 1 (LSP1). The expression patterns of (A) FXIIIa and (B) LSP1 were different in the same specimen of dermatofibroma. (C) FXIIIa-positive cells could be observed sporadically in the normal dermis, whereas (D) LSP1-positive cells could not be observed except for in a few lymphocytes in the normal dermis (A, B: ×40, C, D: ×100). |
 | Fig. 3Histological sections of dermatofibrosarcoma protuberans stained with leukocyte-specific protein 1 (LSP1) antibody. LSP1 staining in the lesion was negative (×200). |
Table 1
Immunohistochemical staining results for DF and DFSP
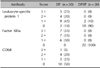
Values are presented as number (%). DF: dermatofibroma, DFSP: dermatofibrosarcoma protuberans. Based on the immunohistochemical profile, the lesions were evaluated and scored as: 3+, >67% of cells stained positive; 2+, 34%~66% of cells stained positive; 1+, 6%~33% of cells stained positive; 0, <5% of cells stained positive.
References
1. Song Y, Sakamoto F, Ito M. Characterization of factor XIIIa+ dendritic cells in dermatofibroma: Immunohistochemical, electron and immunoelectron microscopical observations. J Dermatol Sci. 2005; 39:89–96.

2. Horenstein MG, Prieto VG, Nuckols JD, Burchette JL, Shea CR. Indeterminate fibrohistiocytic lesions of the skin: is there a spectrum between dermatofibroma and dermatofibrosarcoma protuberans. Am J Surg Pathol. 2000; 24:996–1003.
3. Yan X, Takahara M, Xie L, Tu Y, Furue M. Cathepsin K expression: a useful marker for the differential diagnosis of dermatofibroma and dermatofibrosarcoma protuberans. Histopathology. 2010; 57:486–488.

4. Goldblum JR, Tuthill RJ. CD34 and factor-XIIIa immunoreactivity in dermatofibrosarcoma protuberans and dermatofibroma. Am J Dermatopathol. 1997; 19:147–153.

5. Kuroda K, Tajima S. Proliferation of HSP47-positive skin fibroblasts in dermatofibroma. J Cutan Pathol. 2008; 35:21–26.

6. Cerio R, Spaull J, Jones EW. Histiocytoma cutis: a tumour of dermal dendrocytes (dermal dendrocytoma). Br J Dermatol. 1989; 120:197–206.

7. Bellini A, Mattoli S. The role of the fibrocyte, a bone marrow-derived mesenchymal progenitor, in reactive and reparative fibroses. Lab Invest. 2007; 87:858–870.

8. Aiba S, Tagami H. Phorbol 12-myristate 13-acetate can transform monocyte-derived dendritic cells to different cell types similar to those found in dermatofibroma. A possible in vitro model of the histogenesis of dermatofibroma. J Cutan Pathol. 1998; 25:65–71.

9. Yang L, Scott PG, Dodd C, Medina A, Jiao H, Shankowsky HA, et al. Identification of fibrocytes in postburn hypertrophic scar. Wound Repair Regen. 2005; 13:398–404.

10. Bucala R, Spiegel LA, Chesney J, Hogan M, Cerami A. Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Mol Med. 1994; 1:71–81.

11. Blakaj A, Bucala R. Fibrocytes in health and disease. Fibrogenesis Tissue Repair. 2012; 5:Suppl 1. S6.

12. Jongstra-Bilen J, Misener VL, Wang C, Ginzberg H, Auerbach A, Joyner AL, et al. LSP1 modulates leukocyte populations in resting and inflamed peritoneum. Blood. 2000; 96:1827–1835.

13. Kanitakis J, Schmitt D, Thivolet J. Immunohistologic study of cellular populations of histiocytofibromas ("dermatofibromas"). J Cutan Pathol. 1984; 11:88–94.

14. Nestle FO, Nickoloff BJ, Burg G. Dermatofibroma: an abortive immunoreactive process mediated by dermal dendritic cells. Dermatology. 1995; 190:265–268.

15. Kuroda K, Tsukifuji R, Shinkai H. Increased expression of heat-shock protein 47 is associated with overproduction of type I procollagen in systemic sclerosis skin fibroblasts. J Invest Dermatol. 1998; 111:1023–1028.

16. Kubo M, Ihn H, Yamane K, Tamaki K. The expression levels and the differential expression of transforming growth factor-beta receptors in dermatofibroma and dermatofibrosarcoma protuberans. Br J Dermatol. 2006; 154:919–925.

17. Kim HJ, Lee JY, Kim SH, Seo YJ, Lee JH, Park JK, et al. Stromelysin-3 expression in the differential diagnosis of dermatofibroma and dermatofibrosarcoma protuberans: comparison with factor XIIIa and CD34. Br J Dermatol. 2007; 157:319–324.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download