Abstract
Background
Vitamin D insufficiency could be associated with the prevalence of atopic dermatitis (AD).
Objective
To examine vitamin D status and the relations between serum 25-hydroxyvitamin D levels, SCORAD score, serum LL-37 level, and body mass index (BMI) in Korean AD patients, and to explore whether these associations differ between adults and children.
Methods
Serum 25-hydroxyvitamin D levels, serum LL-37, and clinical features were analyzed in a total of 72 Korean patients with AD (39 adults and 33 children) and 140 healthy control subjects (70 adults and 70 children).
Results
Serum 25-hydroxyvitamin D levels were significantly reduced in children with AD (15.06±4.64 ng/ml) compared with normal children in the control group (16.25±6.60 ng/ml) (p=0.036). Significant inverse correlations were found between BMI and 25-hydroxyvitamin D level (r=-0.315, p=0.007) and between the SCORAD score and serum LL-37 level (r=-0.3, p=0.011) in the total AD patients.
Conclusion
The results showed that serum vitamin D levels were lower in children with AD than in healthy children; however, the same relation was not observed between adults with AD and healthy adults. Serum 25-hydroxyvitamin D concentration was not significantly correlated with AD severity or serum LL-37 levels in our study population.
Vitamin D insufficiency is an increasingly recognized problem among the general population, and has been largely attributed to dietary, lifestyle, and behavioral changes1. Although its musculoskeletal consequences are well established, a new hypothesis has linked atopic dermatitis (AD) to lower vitamin D levels2,3. Vitamin D has several effects on the skin that can enhance keratinocyte differentiation, increase wound healing, decrease inflammation, and induce cathelicidin (LL-37) production4,5, and these effects might be relevant in the primary prevention of AD6. LL-37 deficiency in the skin, in particular, has a known association with AD6. Recently, several studies have investigated the serum vitamin D levels of AD patients, and the correlation between serum vitamin D level and AD severity7,8,9,10; however, the results have been conflicting. Therefore, the aims of the current study are to investigate vitamin D status and the relations between serum 25-hydroxyvitamin D (25(OH)D3) level, AD severity (SCORAD score), serum LL-37 level, and body mass index (BMI) in Korean AD patients, and to explore whether these associations differ between adults (≥18 years old) and children (<18 years old).
Seventy-two Korean patients with AD, including 39 adults (age range, 18~51 years) and 33 children (age range, 12 months~16 years) participated in this study. The diagnosis was based on the classification of Hanifin and Rajka. The control group consisted of 140 healthy, age- and sexmatched subjects, including 70 adults and 70 children. All patients and control subjects were Koreans with phototype IV or V skin according to the Fitzpatrick classification. The study was performed from December 2012 to February 2013 to avoid seasonal variations in vitamin D levels. The demographic characteristics of the study population are shown in Table 1. None of the patients received oral or topical corticosteroids, calcineurin inhibitors, or systemic immunosuppressives for at least 4 weeks before enrollment. In addition, subjects were excluded from the study if they had received oral vitamin D or any medication known to interact with calcium in the previous 6 months. Approval for this study was obtained from the institutional review board of Eulji General Hospital (IRB No. 12-61).
The same physician evaluated the severity of AD in all patients by using the SCORAD index. Eczema was scored in each patient as mild (<25), moderate (25~50), or severe (>50), as defined in previous studies11. Levels of 25(OH)D3 were analyzed with a chemiluminescent method (LIAISON 25-OH Vitamin D Total; DiaSorin, Saluggia, Italy). Values were used as a continuous variable and vitamin D amounts were also categorized, in a descriptive analysis, as follows: sufficient, ≥30 ng/ml; insufficient, 21~29 ng/ml; and deficient, ≤20 ng/ml. Cathelicidin expression was determined by using a human LL-37 ELISA kit (Hycult Biotech, Uden, the Netherlands).
Comparisons between the healthy control group and the AD group were made by using independent t-tests for vitamin D levels. Correlations among variables were investigated with the Pearson's correlation coefficient. Among groups presenting different AD severities as determined with the SCORAD index, a comparison of vitamin D levels was performed with ANOVA. p-values ≤ 0.05 were considered statistically significant. A commercially available software was used for data analysis (SPSS 14.0; SPSS Inc., Chicago, IL, USA).
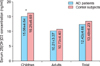
Serum 25(OH)D3 levels, representing systemic vitamin D3 status, were significantly reduced in children with AD (15.06±4.64 ng/ml) compared with the normal children in the control group (16.25±6.60 ng/ml) (p=0.036). Serum 25(OH)D3 levels were not statistically different (p>0.05) between the 72 patients with AD (12.43±4.66 ng/ml) and the 140 control subjects (13.49±6.23 ng/ml), or between adults with AD (10.21±3.37 ng/ml) and the normal adult controls (10.73±4.40 ng/ml) (Fig. 1). Levels of 25(OH)D3 in AD patients and control subjects were considered deficient in 65 of 72 (90%) and 116 of 140 (83%) subjects, respectively, and were insufficient in 7 of 72 (10%) and 23 of 140 (16%) subjects. All adults with AD (39 of 39, 100%) and 26 of 33 children with AD (78.8%) showed deficient 25(OH)D3 levels. Only one child in the control group had a sufficient 25(OH)D3 level. On SCORAD examination, 1 (1.4%) patient had mild AD, 36 (50%) patients had moderate AD, and 36 (48.6%) patients had severe AD. Differences in serum vitamin D levels among the different eczema severity groups were not statistically significant (p>0.05). Fig. 2 shows the correlations between 25 (OH)D3 levels, SCORAD scores, BMI, and serum LL-37 levels in all patients with AD. Significant inverse correlations were found between BMI and vitamin D levels (r=-0.315, p=0.007), and between SCORAD scores and serum LL-37 levels (r=-0.3, p=0.011). In the control group, a significant inverse correlation between BMI and vitamin D level was found (r=-0.335, p=0.009). After subdividing the group into adults and children, only the correlation between SCORAD score and serum LL-37 levels of adult group remained significant (r=-0.359, p=0.025).
Peroni et al.9 reported a correlation between vitamin D deficiency and the severity of AD in children, which seemed to support previous epidemiological observations suggesting a possible inverse association between vitamin D nutritional intake or exposure to the sun and AD disease prevalence12. However, other studies found no association between serum vitamin D levels and the SCORAD score7,8. In accordance with these later studies, our study did not demonstrate an inverse correlation between serum 25(OH)D3 concentration and AD severity. In asthma, another representative allergic disease, several studies have indicated that low 25(OH)D3 levels are correlated with poor disease control, reduced lung function, reduced glucocorticoid response, and consequent increased steroid use13,14,15. Goleva et al.16 reported that this association was mainly significant in pediatric patients, and not in the adult asthma group. Thus, we analyzed these correlations among variables after subdividing the patients into the adults group and the children group. However, a correlation between serum 25(OH)D3 concentration and AD severity was not found in the two groups17.
Several studies in Korea have indicated a high prevalence of vitamin D deficiency in healthy Koreans17,18,19. Koreans are theoretically at an increased risk for vitamin D insufficiency because of living at high latitudes and because of their increased use of sunscreen, reduced outdoor activities, and a lack of intake of vitamin D-fortified foods17,20.
According to one investigation during winter, the prevalence of vitamin D deficiency in Koreans was >90%18. In agreement with these results, our study revealed that 90% of patients with AD and 83% of healthy controls were vitamin D deficient. The difference in serum vitamin D levels between these two groups was not statistically significant; however, in subgroup analysis, children with AD showed significantly lower serum vitamin D levels than age- and sex-matched healthy controls. Most allergies begin in childhood; thus, the significantly lower level of vitamin D observed in young AD patients might be related to the initiation of AD.
In this study, serum LL-37 was used as a vitamin D-regulated target. LL-37 is one of the most well-known antimicrobial peptides, and it acts against bacteria, viruses, and fungi6,21. Reduced expression of antimicrobial peptides may cause recurrent infections, and decreased LL-37 expression is known to be associated with AD6,21. Vitamin D enhances LL-37 production in keratinocytes because promoters of cathelicidin genes contain consensus vitamin D response elements4. Oral vitamin D3 has been shown to increase cathelicidin expression in AD lesions22. Kanda et al.10 recently reported that serum LL-37 levels correlated with 25(OH)D3 in AD patients. However, in the present study, we did not observe a positive correlation between 25(OH)D3 and serum LL-37 level in any group. We assume that these conflicting results may be because serum LL-37 is produced by multiple cell types, and a number of vitamin D-independent pathways control LL-37 production23. Of interest, a significant inverse correlation was found between the SCORAD score and serum LL-37 level in all AD patients and in the adult AD subgroup. This finding is in contrast with the results of Leung et al.24, who reported that serum LL-37 levels show a positive correlation with eczema severity in children, suggesting that circulating LL-37 might be a biomarker for eczema severity. The basis for the differences between these studies remains unclear; however, our results suggest that LL-37 production decreases in proportion to AD severity.
As previously reported25,26, we observed a significant negative correlation between BMI and serum 25(OH)D3 concentration. One reason proposed for this relation has been the presumed lesser physical activity and, therefore, reduced sun exposure of overweight and obese persons27. Another possible explanation is that body fat may act as a sink for vitamin D, which could be deposited in an almost irreversible manner, and is not bioavailable28.
In conclusion, we observed that most participants in both the AD and control groups were vitamin D deficient. Vitamin D levels were lower in children with AD than in controls; however, the same relation was not observed in adults with AD. There were statistically significant correlations between BMI and serum 25(OH)D3 concentration in all participants, and between the SCORAD score and serum LL-37 level in all AD patients and in the adult AD subgroup; however, we were unable to detect an inverse correlation between serum vitamin D level and the SCORAD score.
Recently, the beneficial effect of oral supplementation with vitamin D has been reported in several studies8,29,30. However, additional investigations on the association between vitamin D and AD, as well as on the effects of vitamin D supplementation are needed in a larger study population before vitamin D can be recommended as a treatment option for AD.
Figures and Tables
Fig. 1
Mean serum 25-hydroxyvitamin D concentration in the atopic dermatitis (AD) and control groups. *p<0.05.
References
1. Benson AA, Toh JA, Vernon N, Jariwala SP. The role of vitamin D in the immunopathogenesis of allergic skin diseases. Allergy. 2012; 67:296–301.

3. Paul G, Brehm JM, Alcorn JF, Holguín F, Aujla SJ, Celedón JC. Vitamin D and asthma. Am J Respir Crit Care Med. 2012; 185:124–132.

4. Wang TT, Nestel FP, Bourdeau V, Nagai Y, Wang Q, Liao J, et al. Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J Immunol. 2004; 173:2909–2912.

5. Gurlek A, Pittelkow MR, Kumar R. Modulation of growth factor/cytokine synthesis and signaling by 1alpha,25-dihydroxyvitamin D(3): implications in cell growth and differentiation. Endocr Rev. 2002; 23:763–786.

6. Ong PY, Ohtake T, Brandt C, Strickland I, Boguniewicz M, Ganz T, et al. Endogenous antimicrobial peptides and skin infections in atopic dermatitis. N Engl J Med. 2002; 347:1151–1160.

7. Chiu YE, Havens PL, Siegel DH, Ali O, Wang T, Holland KE, et al. Serum 25-hydroxyvitamin D concentration does not correlate with atopic dermatitis severity. J Am Acad Dermatol. 2013; 69:40–46.

8. Samochocki Z, Bogaczewicz J, Jeziorkowska R, Sysa-Jędrzejowska A, Glińska O, Karczmarewicz E, et al. Vitamin D effects in atopic dermatitis. J Am Acad Dermatol. 2013; 69:238–244.

9. Peroni DG, Piacentini GL, Cametti E, Chinellato I, Boner AL. Correlation between serum 25-hydroxyvitamin D levels and severity of atopic dermatitis in children. Br J Dermatol. 2011; 164:1078–1082.

10. Kanda N, Hau CS, Tada Y, Sato S, Watanabe S. Decreased serum LL-37 and vitamin D3 levels in atopic dermatitis: relationship between IL-31 and oncostatin M. Allergy. 2012; 67:804–812.

11. Oranje AP, Glazenburg EJ, Wolkerstorfer A, de Waard-van der Spek FB. Practical issues on interpretation of scoring atopic dermatitis: the SCORAD index, objective SCORAD and the three-item severity score. Br J Dermatol. 2007; 157:645–648.

12. Hyppönen E, Sovio U, Wjst M, Patel S, Pekkanen J, Hartikainen AL, et al. Infant vitamin d supplementation and allergic conditions in adulthood: northern Finland birth cohort 1966. Ann N Y Acad Sci. 2004; 1037:84–95.

13. Brehm JM, Schuemann B, Fuhlbrigge AL, Hollis BW, Strunk RC, Zeiger RS, et al. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J Allergy Clin Immunol. 2010; 126:52–58.e5.

14. Brehm JM, Celedón JC, Soto-Quiros ME, Avila L, Hunninghake GM, Forno E, et al. Serum vitamin D levels and markers of severity of childhood asthma in Costa Rica. Am J Respir Crit Care Med. 2009; 179:765–771.

15. Chinellato I, Piazza M, Sandri M, Peroni D, Piacentini G, Boner AL. Vitamin D serum levels and markers of asthma control in Italian children. J Pediatr. 2011; 158:437–441.

16. Goleva E, Searing DA, Jackson LP, Richers BN, Leung DY. Steroid requirements and immune associations with vitamin D are stronger in children than adults with asthma. J Allergy Clin Immunol. 2012; 129:1243–1251.

17. Kim SH, Oh MK, Namgung R, Park MJ. Prevalence of 25-hydroxyvitamin D deficiency in Korean adolescents: association with age, season and parental vitamin D status. Public Health Nutr. 2014; 17:122–130.

18. Lee YA, Kim HY, Hong H, Kim JY, Kwon HJ, Shin CH, et al. Risk factors for low vitamin D status in Korean adolescents: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008-2009. Public Health Nutr. 2014; 17:764–771.

19. Choi EY. 25(OH)D status and demographic and lifestyle determinants of 25(OH)D among Korean adults. Asia Pac J Clin Nutr. 2012; 21:526–535.
20. Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. CSA) Nutrition Working Group. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009; 20:1807–1820.

21. Howell MD, Wollenberg A, Gallo RL, Flaig M, Streib JE, Wong C, et al. Cathelicidin deficiency predisposes to eczema herpeticum. J Allergy Clin Immunol. 2006; 117:836–841.

22. Hata TR, Kotol P, Jackson M, Nguyen M, Paik A, Udall D, et al. Administration of oral vitamin D induces cathelicidin production in atopic individuals. J Allergy Clin Immunol. 2008; 122:829–831.

23. Gallo RL, Murakami M, Ohtake T, Zaiou M. Biology and clinical relevance of naturally occurring antimicrobial peptides. J Allergy Clin Immunol. 2002; 110:823–831.

24. Leung TF, Ching KW, Kong AP, Wong GW, Chan JC, Hon KL. Circulating LL-37 is a biomarker for eczema severity in children. J Eur Acad Dermatol Venereol. 2012; 26:518–522.

25. Frost M, Abrahamsen B, Nielsen TL, Hagen C, Andersen M, Brixen K. Vitamin D status and PTH in young men: a cross-sectional study on associations with bone mineral density, body composition and glucose metabolism. Clin Endocrinol (Oxf). 2010; 73:573–580.

26. Arunabh S, Pollack S, Yeh J, Aloia JF. Body fat content and 25-hydroxyvitamin D levels in healthy women. J Clin Endocrinol Metab. 2003; 88:157–161.

27. Florez H, Martinez R, Chacra W, Strickman-Stein N, Levis S. Outdoor exercise reduces the risk of hypovitaminosis D in the obese. J Steroid Biochem Mol Biol. 2007; 103:679–681.

28. Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000; 72:690–693.

29. Amestejani M, Salehi BS, Vasigh M, Sobhkhiz A, Karami M, Alinia H, et al. Vitamin D supplementation in the treatment of atopic dermatitis: a clinical trial study. J Drugs Dermatol. 2012; 11:327–330.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download