INTRODUCTION
Axillary bromhidrosis is a condition that generates an offensive odor due to interactions between apocrine gland secretions and bacteria. Topical treatment, laser therapy, ultrasonic and/or liposuction curettage, and surgical intervention are currently being used to treat this condition. Laser therapy for axillary bromhidrosis with either a CO2 laser or 1,064 nm Nd:YAG laser has been reported1. However, treatment using a 1,444 nm Nd:YAG laser has not been reported. Herein, we report a patient treated with a 1,444 nm Nd:YAG laser for axillary bromhidrosis and compared its effectiveness and complications with those of conventional surgical intervention.
CASE REPORT
A 25-year-old female presented with malodor in both axillae aggravated since adolescence. She had no medical history, but a maternal family history of axillary bromhidrosis was present. On examination, wet earwax in both ears was noted. Serious hyperhidrosis was diagnosed based on the clinical findings.
We decided to treat the left axilla with the 1,444 nm Nd:YAG laser (Accusculpt™; Lutronic Corp., Seoul, Korea), and the right axilla with a modified Inaba's method2 and compared the effectiveness and complications of each modality.
Both axillary areas were anesthetized with 24 ml of 0.5% lidocaine mixed with 1:100,000 epinephrine. As the 1,444 nm Nd:YAG laser is highly absorbed by water which becomes heat energy, tumescent anesthesia was not used to avoid unwanted thermal damage via heated tumescence.
Laser irradiation areas of 10×5 cm in size were marked on the left axilla. Apocrine glands in the subcutaneous and dermal layers were destroyed by irradiating 1,254 J of laser at 1,444 nm with 175 mJ of pulse energy at a pulse rate of 40 Hz (power 7 W) using a fiber type internal probe via 18-G needle puncture sites (Fig. 1). The amount of energy applied was based on the surface temperature elevation and the extent of fat dissolution assessed by the operator's hands. No liposuction was performed. The 18-G needle puncture sites were not sutured, and the operative area was not compressed.
Modified Inaba's surgery was performed on the right side. After local anesthesia, a 2-cm long single incision line was made, and subdermal dissection was done. Subdermal apocrine glands were manually shaved with a modified Inaba's shaver, and a compression dressing was applied to avoid hematoma or seroma formation.
The patient revisited our hospital on postoperative days 3 and 10 and after 6 and 12 months. Relatively less ecchymosis and scars were observed on the left axilla treated with the laser (Fig. 2). The right and left axillae, including acute complications, were compared at long-term follow-up (Table 1). Other than a serious bruise in the right axilla lasting about 2 weeks and a mild bruise in the left axilla lasting less than 1 week, no major complications were noted. Pain score was measured on a scale of 0 to 10, and the patient experienced no pain in the left axilla. However, the patient experienced moderate to severe pain (7 to 8 out of 10) with activity limitations on the modified Inaba's operation side. As the postoperative compression dressing had to be applied for 2 weeks, activity limitations continued for 2 weeks on the right side. Additionally, postoperative pain continued for 7 to 10 days. The remnant malodor in the left axilla was deemed 'tolerable' (scale 3) and the right axilla was deemed 'none' (scale 0). After the 1 year follow-up, the remaining odor was <10% to 15% compared with the initial grade. Other complications, such as restriction of movement and pain, were completely cleared. The patient's level of satisfaction with the left, laser treated side, was generally high in terms of quality of life.
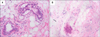
Histological examinations were also done on the subcutaneous fat layer of the laser-irradiated side immediately after the procedure and at 6 months postoperatively (Fig. 3). Immediately after the procedure, the exam showed ablated adipose tissue and apocrine glands. The 6 month histologic examination showed more ablated apocrine glands than previously, which resulted in decrease in malodor.
DISCUSSION
Surgical intervention for bromhidrosis such as Inaba's operation destroys hypodermic fat cells and reduces the number of active apocrine glands2-4. Surgical intervention can lead to higher complete treatment rates and lower recurrence rates but may result in complications, such as axillary nerve plexus damage, postoperative pain, hemorrhage, edema, hematoma, and serious limitations in postoperative mobility3. In addition, the outcome of surgery is surgeon-dependent. For these reasons, no consensus exists on the appropriate surgical method3,4. In our experience, Inaba's method results in the lowest rate of complications and recurrence3.
Minimally invasive therapies have been introduced as patients prefer to be treated by minimally invasive techniques when possible1,4. Among them, laser therapy, which dissolves hypodermic fat and removes apocrine glands, has been highlighted. A 1,064 nm and 1,320 nm Q-switched Nd:YAG laser (Smartlipo® and Coollipo®, Cooltouch®; Lutronic Corp.) are currently being used to dissolve fat1.
However, these two wavelengths are not highly specific for fat cells, and wavelengths of 1,444 nm are more markedly absorbed in fat more than water compared to other wavelengths5. We therefore hypothesized that apocrine glands in fatty tissues would be more specifically destroyed by the 1,444 nm laser. Data show that epidermal temperature is elevated less with 1,444 nm beam therapy, which gives identical energy at the same depth in the hypodermic fat layer as other wavelengths5.
We compared post-laser treatment side effects, recurrence, and patient satisfaction with that of surgical intervention and noted no significant differences between them. Except for crusting and mild ecchymosis on the laser-treated side due to heat-induced skin injury, the patient did not experience other side effects. Although no skin necrosis or other injuries were noted, over-treatment or over-coagulation increases the risk of skin necrosis. Therefore, laser operators should assess superficial skin color changes and measure the superficial temperature in real-time.
We recommend this modality as a possible treatment of choice of osmidrosis because acute phase complications such as pain and restriction of movement were much less than the surgical method. However, if a prepubertal patient strongly hopes for total removal of malodor without recurrence, we would recommend that the patient choose the surgical method, as apocrine glands proliferate during puberty.
In conclusion, subdermal coagulation treatment with a 1,444 nm Nd:YAG laser may be the least invasive but most effective therapy for axillary bromhidrosis. We are now performing a prospective clinical study in a larger cohort population to investigate the ideal laser configuration and to define systematic and standardized protocols.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download