Abstract
Background
Keloids and hypertrophic scars represent excessive scarring. They require different therapeutic approaches, which can be hampered because of an apparent lack of morphologic difference between the two diseases.
Objective
This study investigated the clinical and dermoscopic features of keloids and hypertrophic scars in order to help dermatologists distinguish these lesions better.
Methods
A total of 41 keloids and hypertrophic scars in 41 patients were examined clinically and by performing dermoscopy with a digital imaging system. Lesions were evaluated for vascular structures.
Results
Dermoscopy revealed vascular structures in most keloid lesions (90%) but in only 27% of hypertrophic scar lesions. The most common dermoscopic vascular structures in keloids were arborizing (52%), followed by linear irregular (33%) and commashaped (15%); these features were present but less evident in hypertrophic scars (9% for all types). The distribution frequency of the vascular structures differed significantly between diseases (p<0.001).
Keloids and hypertrophic scars are abnormal wound responses characterized by the overgrowth of fibroblastic tissues during skin healing. They not only cause esthetic problems, but also symptomatic problems such as pruritus and pain1. Keloids and hypertrophic scars are thought to have the same clinical course2,3. However, the discovery of their different pathological pathways, which require unique treatment approaches, has made it critical to distinguish between them1,3,4.
Dermoscopy can provide up to 10 times greater magnification than the unaided eye and can show the structure of the upper layer of the dermis, thus yielding many diagnostically relevant findings. Although dermoscopy has many advantages for the diagnosis of various skin diseases5, it has been difficult to identify characteristics for distinguishing between keloids and hypertrophic scars.
Although known pathological and radiological examinations can be used to distinguish between keloids and hypertrophic scars, it is difficult to apply them in clinical settings because of their high cost and lengthy preparation time. Therefore, we searched for a characteristic finding to distinguish between keloids and hypertrophic scars by using dermoscopy-a simple, noninvasive, and powerful diagnostic tool5.
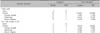
From July 2011 to April 2012, 41 typical lesions were selected from among 41 patients who visited our dermatology clinic and were diagnosed with keloids or hypertrophic scars; there were 18 men, and the average age of the patients was 33.1 years (range, 8~75 years) (Table 1). Keloids were defined as a dermis tumor that extends beyond the original wound without regression. Hypertrophic scars were defined as erythematous scar tissue that remains within the confines of the original wound. In this study, senior dermatology staff performed the diagnostic evaluation of individual lesions, and atypical or ambiguous cases were excluded.
Demographic factors (i.e. sex and age) and lesion-related factors (i.e. scar location and duration, etiology, treatment history, family and medical history, and symptoms) were investigated through patient interviews and medical record reviews (Table 1). Before the analysis, intralesional corticosteroid injections were considered to cause telangiectasia6,7, while cryotherapy and pulsed dye laser were considered to destroy the local vascular system7. All patients who had received cryotherapy or pulsed dye laser therapy had also received intralesional corticosteroid injection therapy. Statistical analysis with and without participants who had received intralesional corticosteroid injection therapy was done.
In order to reduce superficial reflection, ultrasound gel was applied to the lesions. Lesions were observed by using dermoscopy, and the observations were recorded with a connected digital camera (Olympus PEN E-PL2; Olympus, Tokyo, Japan). Lesion findings were analyzed on the basis of the recorded digital images. Dermoscopy was performed with the Dermlite II Pro (3Gen Inc., San Juan Capistrano, CA, USA) with an attached 10× magnifying mirror. The observed vascular structures were sorted into the following 3 categories according to the morphological vascular structure classification system of Zalaudek et al.8: comma-shaped, arborizing, and linear irregular. Comma-shaped vessels are coarse vessels that are slightly curved with little branching. Arborizing vessels are bright red large-diameter stem vessels that branch irregularly into fine terminal capillaries. Finally, a linear irregular pattern is defined as a linear red vessel of irregular shape and size (Fig. 1).
To determine the relationships of observed vascular structures with keloids and hypertrophic scars, Fisher's exact test was applied in cross-tabulation analysis. Odds ratios were calculated to determine the associations of vascular structures with keloids and hypertrophic scars. In addition, cross-tabulation analysis was performed for factors related to lesions (e.g. family history). IBM SPSS Statistics 20.0 (IBM Co., Armonk, NY, USA) was used for all statistical analysis, and the level of significance was set at p<0.05.
The male to female ratio of patients was 1:1.27 (18 men, 23 women), and age ranged from 8~75 years old (mean±standard deviation, 33.1±16.9). Scar lesion duration ranged from 1 month to 30 years. The trunk including the scapular area was the most commonly involved area. The most common causes of scaring were surgery and trauma. Most patients (63%) received previous treatment; patients with keloids experienced more treatments (22/30, 73.3%) than patients with hypertrophic scars (4/11, 36.3%). The most common therapy was intralesional steroid injection. More patients with keloids (10/30, 33.3%) had a family history of excessive scarring and a personal medical history of scarring than patients with hypertrophic scars (1/11, 9.1%). Approximately 40% patients of both groups had either pruritus or pain.
A total of 30 cases out of 41 lesions exhibited some vascular structure on dermoscopic examination. Among the 30 patients with keloids, 14 (47%), 9 (30%), and 4 (13%) had arborizing, linear irregular, and comma-shaped findings, respectively (Fig. 1). Among 11 patients with hypertrophic scars, the number of either observed comma shaped, arborizing, or linear irregular finding was only one (9%) (Fig. 2). Thus, patients with keloids were 24 times more likely to be associated with a vascular structure than patients with hypertrophic scars. The analysis of vascular structure types showed that only arborizing findings were significantly related to keloids (odds ratio, 8.75) (Table 2).
A total of 10 and 9 patients with keloids and hypertrophic scars, respectively, were analyzed separately after excluding patients who had received treatment that could have affected vascular structure. Two comma-shaped (20%), 3 arborizing (30%), and 4 linear irregular (40%) findings were observed in the keloid group; meanwhile, 1 of each (11%) was observed in the hypertrophic scar group. Differential diagnosis based on the specific vascular structures revealed by using dermoscopy was statistically significant according to Fisher's exact test, with an odds ratio of 18, indicating a strong association. Nevertheless, there was no significant association in the analysis of vascular structure type (Table 2).
Cross-tabulation analysis showed no significant relationship between patient characteristics (family history, medical history among others) and symptoms (pruritus and pain) with diagnosis keloids or hypertrophic scars.
In dermoscopic examination, placing fluid (e.g. mineral oil) on the lesion eliminates surface reflection and renders the stratum corneum translucent to a beam of light falling on the cutaneous surface, thus allowing the examiner to observe the size and shape of the blood vessels of the superficial vascular plexus5,9. In the present study, ultrasound gel was applied to the lesions, revealing characteristic vascular structures. Dermoscopy differs from using typical magnifying devices such as a magnifying glass or loupe because the instrument is pressed against the surface of lesion being examined. Because of this effect, which is similar to pressing a glass slide to the skin and applying minimal downward pressure, erythema disappears, enhancing the appearance of vascular, pigmented, or similar skin lesions.
Keloids and hypertrophic scars are abnormal wound responses characterized by excessive scarring. Clinically, most appear as reddish solid masses on the skin10. These diseases are sometimes considered to have the same pathological pathway, as they are hard to distinguish in the early scarring stage and exhibit only small differences when viewed under a light microscope2,3. However, the pathological and immunochemical differences of these diseases are becoming clearer with increasing knowledge of wound healing11. The development of treatment approaches targeting the unique factors and pathways involved in scar formation are predicted in the near future. Therefore, it will become necessary to tailor treatments specific to keloids and hypertrophic scars1,3,4. In addition, as hypertrophic scars can regress spontaneously, it is critical to distinguish the diseases when evaluating treatment response12. Immunochemical examination, electron microscopy, and magnetic resonance imaging can be used to distinguish between keloids and hypertrophic scars13. However, it is difficult to adopt these methods in clinical settings because of time and cost constraints. Therefore, we investigated the feasibility of using dermoscopy-a simple, noninvasive, and powerful5,8 diagnostic tool-to aid the differential diagnosis of these lesions. Dermoscopy is mostly used in the differential diagnosis of malignant melanoma. It is also helpful for a diverse range of other diseases including benign melanocytic lesions, basal cell carcinoma, seborrheic keratosis, and hemangiomas; typical findings for each of these diseases are reported in detail in the literature5. To our knowledge, the dermoscopic findings of keloids or hypertrophic scars have not been reported.
In the present study, dermoscopy showed that keloids appeared to have vascular structures in most cases (27/30 cases, 90%), whereas hypertrophic scars only appeared to have vascular structures in a few cases (3/11 cases, 27%). This tendency was confirmed by using the Fisher's exact test and suggests these typical dermoscopic vascular structures are more frequently observed in keloids than hypertrophic scars. According to the classification of Zalaudek et al.8, the most common dermoscopic vascular structure in this study was arborizing, followed by linear irregular and comma-shaped. The analysis excluding patients who had received previous treatment that could have affected vascular structures also confirmed this association, with 9/10 cases (90%) of keloids and 3/9 cases (33%) of hypertrophic scars showing vascular structures.
The histological findings of blood vessels in keloids have been reported several times. Enlarged blood vessels in the healing process in keloids and hypertrophic scars appear as erythema with apparently related microvessel regeneration and tissue hypertrophy14. Keloids exhibit tissue hypoxia; vascular endothelial growth factor (VEGF) production may be stimulated by hypoxia in this disease pathway. In addition, tissues have increased VEGF levels and vessels, as observed with immunohistochemical staining15. Histologically, keloids have a typical pattern of dispersed, extended vessels7, and subepidermal vessels with luminal bulging of the endothelial lining are conspicuous on electron microscopy16. Therefore, vessels located just under the epidermis are brought into sharp focus by using dermoscopy, which allows the visualization of their bright red color like that of arborizing vessels8. In contrast to keloids, hypertrophic scars have a characteristic nodular structure comprising cells and collagen-forming hard nodules with scant vascularity11. In addition, unlike keloids, hypertrophic scars tend to have vertically oriented vessels relative to the skin surface17. Dermoscopy only provides a horizontal view of the upper dermis. The vascular structures of keloids appear linear and relatively parallel to the skin surface, whereas vascular structures are usually not apparent in hypertrophic scars. The present study clearly demonstrates these dermoscopic findings. Thus, the vascular structures revealed by using dermoscopy could help distinguish keloids and hypertrophic scars even without biopsy.
Family history and symptom presentation are other clinical characteristics that can help distinguish between these diseases. Both diseases are reported to have a genetic predisposition, although keloids are more strongly associated with a positive family history than hypertrophic scars7,18. In this study, patients in the keloid group tended to have a positive family or medical history of excessive scarring compared to patients in the hypertrophic scar group, but this trend was not significant. Both diseases cause pruritus, while keloids can also cause pain7. However, the two disease groups in this study did not show any symptomatic differences. Thus, it seems clinical symptoms and family history alone cannot be used to distinguish these diseases.
In this study, we used dermoscopy, which is readily available in dermatologic outpatient clinics, to help distinguish between keloids and hypertrophic scars. The results show that vascular structures are characteristic of keloids. Even though the analysis did not consider cost-effectiveness, dermoscopy is a simple, inexpensive, quick, noninvasive, and powerful5,8 diagnostic tool.
One limitation of this study is that the lesions studied were limited to only clinically distinguishable keloids and hypertrophic scars. To reduce the uncertainty of diagnosis, we adopted strict clinical criteria used in similar studies19. Nevertheless, in the early stage of scar formation, it may be difficult to diagnose many potential hypertrophic scars and keloids3. Furthermore, we were unable to perform additional specific examination in most cases, although it is impossible to fully differentiate between the two diseases histologically or immunochemically. Therefore, the characteristics of early-stage scars were not analyzed, and therefore, they are not reflected in the results. In addition, the association between scar progression stage and vascular structure findings was unclear because of the small number of subjects, especially those with hypertrophic scars. The association with vascular structure morphology was also unclear in the analysis excluding previously treated patients. These limitations should be considered when applying dermoscopy in the clinical differential diagnosis of scars. Therefore, additional large-scale studies are required to elucidate how vascular structure is influenced by disease stage and previous treatment. A prospective study to observed scar formation and progression immediately after patient receives skin surgery could be one option. Moreover, if such a study includes clinically difficult-to-diagnose lesions with additional specific examinations, results that are more robust can be obtained.
Dermoscopic findings of vascular structures appear to be more characteristic of keloids than hypertrophic scars. This suggests dermoscopic findings can be helpful when distinguishing between keloids and hypertrophic scars in clinical settings. However, as the present study is limited by the small number of patients and use of clinical diagnosis, further investigations of early keloid lesions should be performed.
Figures and Tables
 | Fig. 1Clinical and dermoscopic findings with schematic drawing of the morphological types of vascular structures of patients with keloids. (A) Large erythematous hard nodules on the chest; comma-shaped vessels are visible. (B) Multiple erythematous hard nodules on the chest; arborizing vessels are visible. (C) Multiple erythematous hard nodules on the chest; linear irregular vessels are visible. |
 | Fig. 2Clinical and dermoscopic findings of patients with hypertrophic scars. (A) Dome-shaped hard nodules on the chin; no vascular structures are apparent. (B) Dome-shaped erythematous hard nodules on the back; no vascular structures are apparent. (C) Dome-shaped erythematous hard nodules on the chest; no vascular structures are apparent. |
References
2. Craig RD, Schofield JD, Jackson DS. Collagen biosynthesis in normal and hypertrophic scars and keloid as a function of the duration of the scar. Br J Surg. 1975; 62:741–744.

3. Köse O, Waseem A. Keloids and hypertrophic scars: are they two different sides of the same coin? Dermatol Surg. 2008; 34:336–346.

4. Bran GM, Goessler UR, Hormann K, Riedel F, Sadick H. Keloids: current concepts of pathogenesis (review). Int J Mol Med. 2009; 24:283–293.

5. Campos-do-Carmo G, Ramos-e-Silva M. Dermoscopy: basic concepts. Int J Dermatol. 2008; 47:712–719.

6. Roques C, Téot L. The use of corticosteroids to treat keloids: a review. Int J Low Extrem Wounds. 2008; 7:137–145.

7. Gauglitz GG, Korting HC, Pavicic T, Ruzicka T, Jeschke MG. Hypertrophic scarring and keloids: pathomechanisms and current and emerging treatment strategies. Mol Med. 2011; 17:113–125.

8. Zalaudek I, Kreusch J, Giacomel J, Ferrara G, Catricalà C, Argenziano G. How to diagnose nonpigmented skin tumors: a review of vascular structures seen with dermoscopy: part I. Melanocytic skin tumors. J Am Acad Dermatol. 2010; 63:361–374.

9. Ruocco E, Argenziano G, Pellacani G, Seidenari S. Noninvasive imaging of skin tumors. Dermatol Surg. 2004; 30:301–310.

10. Bouzari N, Davis SC, Nouri K. Laser treatment of keloids and hypertrophic scars. Int J Dermatol. 2007; 46:80–88.

11. Ehrlich HP, Desmoulière A, Diegelmann RF, Cohen IK, Compton CC, Garner WL, et al. Morphological and immunochemical differences between keloid and hypertrophic scar. Am J Pathol. 1994; 145:105–113.
13. Babu M, Bai RP, Suguna L, Ramachandran K, Ramakrishnan KM. Differentiation of keloid and hypertrophic scar; correlation of the water proton relaxation times with the duration of the scar. Physiol Chem Phys Med NMR. 1993; 25:113–120.
14. Kischer CW, Shetlar MR, Chvapil M. Hypertrophic scars and keloids: a review and new concept concerning their origin. Scan Electron Microsc. 1982; 1699–1713.
15. Le AD, Zhang Q, Wu Y, Messadi DV, Akhondzadeh A, Nguyen AL, et al. Elevated vascular endothelial growth factor in keloids: relevance to tissue fibrosis. Cells Tissues Organs. 2004; 176:87–94.

16. Lametschwandtner A, Staindl O. Angioarchitecture of keloids. A scanning electron microscopy study of a corrosion specimen. HNO. 1990; 38:202–207.
17. Lee JY, Yang CC, Chao SC, Wong TW. Histopathological differential diagnosis of keloid and hypertrophic scar. Am J Dermatopathol. 2004; 26:379–384.

18. Atiyeh BS, Costagliola M, Hayek SN. Keloid or hypertrophic scar: the controversy: review of the literature. Ann Plast Surg. 2005; 54:676–680.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download