Abstract
Background
Basal cell carcinoma (BCC) is the most common form of skin cancer and possesses various clinical features including translucency, ulceration, pigmentation, telangiectasia, and rolled borders. Accordingly, many cutaneous lesions can mimic BCCs and differential diagnosis is difficult.
Objective
To clarify the differences in clinical characteristics between BCCs and BCC-mimicking lesions (BMLs), and to determine which clinical characteristics are helpful for an accurate clinical diagnosis of BCC.
Methods
We performed clinicopathologic analysis of cutaneous lesions that received a clinical diagnosis of BCC. All lesions included in this study showed more than one of the following characteristics of BCCs: translucency, ulceration, flecked pigmentation, black or blue hue, telangiectasia, and rolled borders. We compared six clinical characteristics between the BCC group and the BML group.
Results
Among 48 lesions in the BML group, there were 15 premalignant or malignant lesions and 33 benign lesions. Various dermatoses mimicking BCC that have not been reported in the dermatological literature were identified, including angiosarcoma, vulvar intraepithelial neoplasm, foreign body granuloma, intravascular papillary endothelial hyperplasia, sarcoidosis, and others. Compared to the BML group, the BCC group had a significantly higher frequency of translucency (76.3% vs. 52.1%, p<0.001), ulceration or erosion (44.2% vs. 27.1%, p=0.022), black or blue hue (40.0% vs. 22.9%, p=0.020), and rolled borders (49.5% vs. 14.6%, p<0.001). Cutaneous lesions with two or less clinical features of BCC were significantly more likely to be BMLs.
Basal cell carcinoma (BCC) is the most common form of skin cancer, and its prevalence has been consistently increasing. BCCs have several textbook clinical characteristics such as translucency, ulceration, pigmentation, telangiectasia, and rolled borders. These characteristics are shared by many skin diseases and each subtype of BCCs should therefore be differentiated from a variety of other cutaneous disorders (Table 1)1. A variety of cutaneous lesions can mimic the clinical features of BCCs, including adult-onset xanthogranuloma, rhabdomyomatous mesenchymal hamartoma, Darier's disease, epidermal cysts, lymphoma, and several others (Table 2)2,3,4,5,6,7,8,9,10,11,12,13,14,15. Therefore, the differential diagnosis of BCC and BCC-mimicking lesions (BMLs) is complex, yet there have been no studies clarifying the differences in clinical characteristics between BCCs and BMLs, and which clinical characteristics are most helpful for making accurate clinical diagnoses of BCC. Accordingly, we conducted a comparative study between BCCs and BMLs.
There are six textbook clinical characteristics of BCCs: translucency, ulceration, pigmentation, telangiectasia, and rolled borders1. In this study, "pigmentation" was divided into flecked pigmentation and black or blue hue since pigmented BCCs, which are frequent in Asia, possess various degrees of pigmentation16. We defined "flecked pigmentation" as multiple small spots of pigmentation, and "black or blue hue" as homogenous pigmentation. More than one of these six clinical characteristics of BCCs was present in all cases reported as a BML, or in cases mistakenly reported as BCC, in the dermatological literature (Table 2).
We enrolled 656 patients with cutaneous lesions, of which the first clinical diagnosis was BCC at the Skin Cancer Clinic of the Department of Dermatology at Pusan National University Hospital, from August 2002 to July 2011. The study was approved by the ethics committee of PNUH (E-2013023). All lesions showed more than one of the six characteristics listed above. The number of patients in the BCC group was 608, and in the BML group was 48. The demographic data are shown in Table 3.
After histopathologic evaluation, we analyzed which cutaneous diseases can mimic BCC.
On the basis of clinical photographs, we evaluated how often each characteristic (translucency, telangiectasia, flecked pigmentation, ulceration or erosion, black or blue hue, and rolled borders) was found in the BCC group and the BML group. All statistical analyses were performed by means of IBM SPSS Statistics 21.0 (IBM Co., Armonk, NY, USA).
To compare the six characteristics between the BCC group and the BML group, statistical analysis was performed using Fisher's exact test. The level of significance in this study was set at a p-value of below 0.05.
Among 48 BMLs, there were 15 premalignant or malignant lesions and 33 benign lesions. Cases of precancerous and malignant lesions included six cases of actinic keratosis; four cases of squamous cell carcinoma; two cases of malignant melanoma; and one case each of angiosarcoma, Paget's disease, and vulvar intraepithelial neoplasia. Benign disorders included six cases of seborrheic keratosis; four cases of intradermal nevus; three cases each of keratoacanthomas, trichoblastoma, and scars; two cases each of trichoepithelioma, compound nevus, and apocrine hidrocystoma; and one case each of cutaneous myxoma, dilated pore of Winer, foreign body granuloma, intravascular papillary endothelial hyperplasia, lymphomatoid keratosis, rosacea, sarcoidosis, and sebaceous hyperplasia.
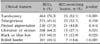
Compared to the BML group, the BCC group had a significantly higher frequency of translucency (76.3% vs. 52.1%, p<0.001), ulceration or erosion (44.2% vs. 27.1%, p=0.022), black or blue hue (40.0% vs. 22.9%, p=0.020), and rolled borders (49.5% vs. 14.6%, p<0.001). In the case of telangiectasia (41.6% vs. 52.1%, p=0.158) and flecked pigmentation (37.9% vs. 43.8%, p=0.416), there was no statistically significant difference between the two groups (Table 5).
With respect to the number of clinical characteristics in each case, when the number present was two or less, the relevant lesions were highly likely to belong to the BML group (35.7% vs. 72.9%, p<0.001). When the number was three or more, they were highly likely to belong to the BCC group (64.3% vs. 27.1%, p<0.001; Fig. 1).
The clinical characteristics of BCC are commonly known to include translucency, ulceration, pigmentation, telangiectasia, and a rolled border. Of these, ulceration, pigmentation, and telangiectasia are commonly seen in daily dermatological practice. Therefore, various diseases, including infectious skin disorders, can mimic BCC (Table 1, 2), and diagnostic pitfalls might exist between BCC and BMLs. However, there has been no systematic trial to analyze and resolve these issues.
In this study, the BML group included various malignant and benign dermatoses. Among these, there were a variety of additional cutaneous disorders that have not yet been reported: angiosarcoma, vulvar intraepithelial neoplasm, foreign body granuloma, intravascular papillary endothelial hyperplasia, sarcoidosis, and others (Fig. 2, 3).
Among the six main clinical characteristics, translucency, ulceration or erosion, black or blue hue, and rolled borders were found more frequently in the BCC group and this was statistically significant. In the case of telangiectasia and flecked pigmentation, there was no significant difference between the BCC group and the BML group. Telangiectasia and flecked pigmentation could therefore be less reliable clinical characteristics for the diagnosis of BCCs in Korean clinical practice than the other four. Over the past two decades, laser ablation of benign skin lesions such as nevi or seborrheic keratosis on the face has gained wide popularity in Korea. Accordingly, some patients with BCCs are likely to be treated by laser ablation after being diagnosed with these benign skin tumors17. In this respect, the results of this study may be helpful for the early detection of BCCs in Korea.
In addition, when a lesion shows two or fewer of the six textbook characteristics of BCCs, it is highly likely to be a BML. When three or more clinical characteristics are present, it is highly likely to be a BCC. Therefore, when one or two clinical characteristics of BCCs are observed at the time of cutaneous lesion examination, other cutaneous disorders should be considered before BCC.
In conclusion, we identified more cutaneous disorders capable of mimicking BCCs than have been previously reported in the literature. In cases of BCC in Korea, translucency, ulceration or erosion, black or blue hue, and rolled borders could be more reliable as diagnostic clinical characteristics than telangiectasia and flecked pigmentation. If a cutaneous lesion suspected to be a BCC possesses three or more clinical characteristics of BCCs, including translucency, telangiectasias, flecked pigmentation, ulceration or erosion, black or blue hue, and rolled borders, it is significantly more likely to be a BCC. The results of this study are thought to contribute to the accurate clinical diagnosis of BCC and provide more detailed information compared to dermoscopic findings alone.
Figures and Tables
Fig. 1
Percentage according to number of clinical characteristics of basal cell carcinoma (BCC) in cases of BCCs and BCC-mimicking lesions. *p<0.05.

Fig. 2
Various malignant and premalignant cutaneous lesions mimicking basal cell carcinoma. (A, B) Angiosarcoma. Diagnostic pitfalls; black hue (CD31 ×100). (C, D) Vulvar intraepithelial neoplasm. Diagnostic pitfalls; translucency, telangiectasia, erosion, blue hue, and rolled border (H&E, ×100).

Fig. 3
Various benign cutaneous lesions mimicking basal cell carcinoma (A, B) Intravascular papillary endothelial hyperplasia. Diagnostic pitfalls; blue hue (H&E, ×40). (C, D) Sarcoidosis. Diagnostic pitfalls; translucency, rolled border (H&E, ×100).

Table 1
Differential diagnosis of basal cell carcinoma

Modified from Fitzpatrick's dermotology in general medicine. 8th ed. New York: McGrow-Hill, 2012:1294-13031.
Table 2
Reported cases of other dermatoses mimicking basal cell carcinoma in searching PubMed/MEDLINE*

ACKNOWLEDGMENT
This study was supported by a Medical Research Institute Grant (2011-08), Pusan National University Hospital.
References
1. Carucci JA, Leffel DJ, Pettersen JS. Basal cell carcinoma. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermotology in general medicine. 8th ed. New York: McGrow-Hill;2012. p. 1294–1303.
2. Bohn OL, Sanchez-Sosa S. Rhabdomyomatous mesenchymal hamartoma mimicking basal cell carcinoma. Am J Dermatopathol. 2009; 31:309–310.

3. Lovato L, Salerni G, Puig S, Carrera C, Palou J, Malvehy J. Adult xanthogranuloma mimicking basal cell carcinoma: dermoscopy, reflectance confocal microscopy and pathological correlation. Dermatology. 2010; 220:66–70.

4. Russell DJ, Dutton JJ, Fowler AM. Darier disease mimicking Basal cell carcinoma of the eyelid. Ophthal Plast Reconstr Surg. 2009; 25:144–146.

5. Akinyemi E, Mai L, Matin A, Maini A. Diffuse large B-cell lymphoma mimicking advanced basal cell carcinoma. J Natl Med Assoc. 2007; 99:948–950.

6. Ghaffar SA, Clements SE, Lear JT. Epidermoid cysts mimicking recurrence of superficial basal cell carcinoma following photodynamic therapy. Clin Exp Dermatol. 2007; 32:223–224.

7. Hinz T, Wiechert A, Bieber T, Bauer R, Schmid-Wendtner MH. Lymphoepithelioma-like carcinoma of the skin mimicking a basal cell carcinoma. Eur J Dermatol. 2009; 19:179–180.

8. Lott DG, Akst LM, Greene D, Roberts JK. T-cell primary cutaneous anaplastic large cell lymphoma mimicking appearance of large basal cell carcinoma. Otolaryngol Head Neck Surg. 2006; 135:170–171.

9. Hague J, Ilchyshyn A. Nickel allergy mimicking basal cell carcinoma. Contact Dermatitis. 2006; 54:344–345.

10. Bechara FG, Rotterdam S, Hoffmann K, Altmeyer P, Stücker M, Jansen T. Pomade crust on the scalp mimicking recurrent basal cell carcinoma. Dermatol Nurs. 2003; 15:426–427.
11. Askar S, Kilinc N, Aytekin S. Syringocystadenoma papilliferum mimicking basal cell carcinoma on the lower eyelid: a case report. Acta Chir Plast. 2002; 44:117–119.
12. Goto M, Sonoda T, Shibuya H, Terashi H, Kai Y, Sato T, et al. Digital syringomatous carcinoma mimicking basal cell carcinoma. Br J Dermatol. 2001; 144:438–439.

13. Ingleton R, Koestenblatt E, Don P, Levy H, Szaniawski W, Weinberg JM. Cutaneous cryptococcosis mimicking basal cell carcinoma in a patient with AIDS. J Cutan Med Surg. 1998; 3:43–45.

14. Tsao H, Tahan SR, Johnson RA. Chronic varicella zoster infection mimicking a basal cell carcinoma in an AIDS patient. J Am Acad Dermatol. 1997; 36:831–833.

15. Lobur DM, Bailin PL, Taylor JS. Severe irritant dermatitis mimicking a basal cell carcinoma. Cleve Clin Q. 1983; 50:465–467.

16. Ono T, Egawa K, Yamamoto S, Arao T. Pigmented basal cell carcinoma developing on the lower extremities--three cases masquerading as malignant melanoma. J Dermatol. 1989; 16:325–329.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download