Abstract
Background
An antibiotic-free, fixed-dose combination gel with adapalene (A) 0.1% and benzoyl peroxide (BPO) 2.5% has been developed for treatment of acne vulgaris.
Objective
To compare the clinical outcomes of A-BPO combination gel with vehicle gel for treatment or maintenance therapy of patients with acne vulgaris.
Methods
An electronic search of the database PubMed (1966 to September 2012), Embase (1984 to September 2012), and Cochrane Controlled Trials Register (CENTRAL; 3rd Quarter, 2012) was undertaken to identify relevant studies. Main clinical outcomes were success rate, treatment-related adverse events (AEs), AEs leading to discontinuation, satisfaction with the effectiveness, and overall satisfaction.
Results
Six studies were finally included in this meta-analysis. The A-BPO group yielded better clinical outcomes regarding the success rate (p<0.00001), satisfaction with the effectiveness of treatment (p=0.005), and overall satisfaction (p=0.005) compared to the vehicle group. The incidence of treatment-related AEs in the A-BPO group was comparable with that of vehicle group (p=0.09), while the A-BPO group was associated with a slightly increase in the incidence of AEs leading to discontinuation when compared with the vehicle group (p=0.02).
Conclusion
A-BPO combination gel yields better clinical outcomes including success rate, satisfaction with the effectiveness, and overall satisfaction compared to vehicle gel, despite an increased incidence of AEs leading to discontinuation. The A-BPO combination agent most likely contributes to the treatment of moderate acne vulgaris rather than severe acne vulgaris, but it may be useful in maintenance therapy of patients with severe acne vulgaris.
Acne vulgaris is a complex skin disorder involving multiple abnormalities of the pilosebaceous unit, including ductal hyperkeratinization and increased cohesiveness of keratinocytes, increased sebum production, Propionibacterium acnes hypercolonization, and inflammation1. Duration of acne varies from 3 months to 5~40 years, and for 80% of patients the disease does not spontaneously regress until they are in their thirties2. Conventional therapies recommended for the treatment of acne vulgaris include retinoids, benzoyl peroxide (BPO), antibiotics, and hormonal therapy. Due to the multifactorial pathogenesis of acne vulgaris and the limitations of the conventional therapies, combination therapy utilizing agents with complementary mechanisms provides the opportunity to target multiple pathogenetic causes of acne vulgaris3. One well-established combination therapy is a topical retinoid and an antimicrobial for the treatment of mild to moderately severe inflammatory acne vulgaris4. However, various combination therapies do not act against all 4 of the major pathophysiologic features of acne vulgaris.
As far as overcoming this limitation is concerned, an antibiotic-free, fixed-dose combination gel with adapalene 0.1% and BPO 2.5% has been recently developed for the once-daily treatment of acne vulgaris. In several double-blind, randomized controlled trials (RCTs)5-7, the adapalene-BPO (A-BPO) combination therapy applied once daily for 12 weeks significantly reduced the number of both inflammatory and noninflammatory lesions in subjects with moderate acne vulgaris, with a rapid onset of action and a good safety profile when compared with the adapalene and BPO monotherapies. The effect of A-BPO was sustained for 4 months, and was safe as a long-term treatment for up to 12 months8.
The complementary modes of action as well as the efficacy and safety profiles of these two agents make A-BPO a rational choice for treatment for all but the most severe cases of acne vulgaris. Adapalene is a receptor-selective naphthoic acid derivative with anti-inflammatory, comedolytic, and anticomedogenic properties9-11, while BPO exhibits a potent and rapid bactericidal effect against P. acnes4. Adapalene and BPO do not create selective pressure for resistance. Hence, this combination may be expected to decrease the incidence of bacterial resistance relative to antibiotics12. Furthermore, unlike tretinoin, adapalene is stable when combined with BPO, even in the presence of light13.
Some RCTs have compared the clinical outcomes of A-BPO combination gel with the vehicle gel in the treatment or maintenance therapy of moderate or severe acne vulgaris5-7,14. Recently, several such trials compared the clinical outcomes of a combination treatment using doxycycline or lymecycline and A-BPO compared with doxycycline or lymecycline and vehicle in the treatment of severe acne vulgaris15,16. However, neither trial was sufficiently large enough to confirm the outcomes within subgroups. A meta-analysis that allows for the pooling and quantification of results from different studies is required to overcome this limitation.
To comprehensively compare the clinical outcomes of the A-BPO combination gel with the vehicle gel for the treatment or maintenance therapy of patients with moderate or severe acne vulgaris, we performed the present meta-analysis.
Databases including PubMed (1966 to September 2012), Embase (1984 to September 2012), and Cochrane Controlled Trials Register (CENTRAL; 3rd Quarter, 2012) were searched. The search strategy consisted of a combination of keywords concerning the pharmacotherapy (A-BPO) and keywords regarding the disease (acne vulgaris, acne). These keywords were used as MeSH headings and free text words. The search was limited to humans, clinical trials, reviews, and meta-analyses. In addition, manual searching of reference lists from potentially relevant papers was performed based on the computer-assisted strategy, to identify any additional studies that may have been missed.
Using a predefined protocol, two reviewers (ZRY and JX) independently selected studies for evaluation, with disagreements resolved through consensus decision. The inclusive criteria were: (1) studies comparing the clinical outcomes of A-BPO combination gel with vehicle gel for the treatment or maintenance therapy of patients with moderate or severe acne vulgaris; (2) prospective, randomized, and controlled fashion; (3) studies published in English; (4) studies with the full-text available; (5) studies involving subjects over 12-years-of-age; and (6) data not duplicated in another manuscript. Trials with less than 30 patients were excluded from this study.
Two reviewers independently extracted relevant data from the included studies regarding the details of authors, year of publication, patient demography (number, mean age, and sex ratio), location of study population, inclusion criteria of acne vulgaris, treatment details, and the length of follow-up. The relevant clinical outcomes pooled in this analysis included: (1) success rate (the percentage of subjects rated 'clear' or 'almost clear' on the investigator's global assessment scale [IGA] of acne severity), (2) treatment-related adverse events (AEs), (3) AEs leading to discontinuation, (4) the rate of satisfaction with the effectiveness of treatment, and (5) the rate of overall satisfaction of treatment.
To establish inconsistency in the study results, a test for heterogeneity (Cochrane Q) was performed. However, because the test is susceptible to the number of trials included in the meta-analysis, we also calculated I2. I2, directly calculated from the Q statistic, describes the percentage of variation across the studies due to heterogeneity rather than change. I2 ranges from 0% to 100%, with 0% indicating the absence of any heterogeneity. Although absolute numbers for I2 are not available, values <50% are considered low heterogeneity. When I2 is <50%, low heterogeneity is assumed, and the effect is thought to be due to change. Conversely, when I2 exceeds 50%, then heterogeneity is thought to exist and the effect is random.
Two independent investigators evaluated the risk of bias of the included studies according to the Collaboration's recommended tool (Chapter 8, Section 8.5)17. Briefly, the risk of bias of each study was assessed using the following methodological components: (1) randomization and generation of the allocation sequence (for selection bias), (2) allocation concealment (for selection bias), (3) patients blinding (for performance bias) and examiner blinding (for detection bias), and (4) description of the follow-up (for attrition bias). The details of each methodological item are shown in Table 1. Trials with all four methodological items adequate are considered to be with low risk of bias.
We conducted the meta-analysis using the software Revman 5.1 (provided by the Cochrane Collaboration, Oxford, UK) for an outcome where data are available from more than one study. The analyses included all patients irrespective of compliance or follow-up following the 'intention-to-treat' principle and using the last reported observed response. Results were expressed as risk ratio (RR) and/or odds ratio (OR) with 95 percent confidence interval (CI) for the dichotomous outcomes. A fixed effects model was initially used; however, a random effects model was planned to be used if there was evidence of significant heterogeneity across trials (p<0.1 and I2> 50%). A sensitivity analysis was performed to explore the potential source of heterogeneity. In addition, according to the severity of acne vulgaris, subgroup meta-analysis was also performed to assess whether it could influence the pooled estimates.
Fig. 1 shows details of study identification, inclusion, and exclusion. The search on PubMed, Embase, and the Cochrane Library under the defined terms yielded 281 articles. By screening the titles and abstracts, 268 references were excluded due to their irrelevance to this topic. After the comprehensive evaluation of the remaining 13 potentially relevant references, seven studies were excluded with the raw data duplicated18-24. Finally, six studies were included in the present meta-analysis5-7,14-16. The main characteristics of the six studies are shown in Table 1. The six studies enrolled 2,970 patients with moderate or severe acne vulgaris. Patients of 1,529 were randomly assigned to the A-BPO group, while other 1,441 patients were assigned to the vehicle group.
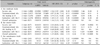
The assessment of risk of bias in all included studies is shown in Table 2. Adequate method of generation of the allocation sequence was described in two trials14,16, while in the other trials it was either not described or unclear. Packaging the topical medication in identical tubes for allocation concealment was applied in four trials5,6,15,16. The patient blinding and the examiner blinding was clearly described in four trials5,6,15,16, and the description of the follow-up was considered adequate (numbers and reasons for dropouts and withdrawals) in all included trials. As a result, all these included trials except one16, with one or more methodological components unclear, were regarded as high-bias risk trials.
The success rate, defined as the percentage of subjects rated 'clear' or 'almost clear' on the IGA of acne severity, was investigated across all the included trials. Totally, the success rate in the A-BPO and vehicle group was 37.67% (576/1,529) and 17.49% (252/1,441), respectively. The chi-square test for heterogeneity revealed that there was a substantial heterogeneity across the trials (p=0.002, I2=74%). Pooled estimates showed that a significant difference was detected between the two groups (RR=2.25, 95% CI: 1.73 to 2.92, p<0.00001; Fig. 2), suggesting that the success rate was significant higher in the A-BPO group than in the vehicle group. Sensitivity analysis showed that the main contributor to heterogeneity was the study by Dréno et al.16. The exclusion of this study could eliminate the heterogeneity among the studies (p=0.17, I2=38%), and pooled estimates of the remaining five trials in a fixed effects model still revealed a significant statistical difference between the two groups (p<0.00001).
The majority of treatment-related AEs were of a dermatological nature, with none being severe or serious. Overall, there were five trials reported the outcome of treatment-related AEs5,6,14-16, and it occurred in 203 of 1,114 patients (18.22%) in A-BPO group, as compared with 81 of 1,023 patients (7.92%) in vehicle group. The chi-square test for heterogeneity detected a substantial heterogeneity across the five trials (p=0.002, I2=74%), which could not be eliminated by a sensitivity analysis and a random-effects model was performed. Pooled estimates showed that there was no significant difference between the two groups (OR=2.24, 95% CI: 0.87 to 5.77, p=0.09; Fig. 3A).
Data required for this meta-analysis was available from three trials6,7,15. In total, the incidence of AEs leading to discontinuation in the A-BPO and vehicle group was 2.25% (24/1,066) and 0.94% (10/1,063), respectively. The chi-square test for heterogeneity revealed that no evidence of heterogeneity was detected across the three trials (p=0.10, I2=57%). Using a fixed-effects model, pooled estimates showed that there was a significant difference between the two groups (OR=2.42, 95% CI: 1.15 to 5.07, p=0.02; Fig. 3B), indicating that A-BPO group was associated with an increase in the incidence of AEs leading to discontinuation when compared with vehicle group.
The satisfaction measured by the question "How satisfied were you with the effectiveness of the treatment?" was reported in four trials6,7,15,16. Overall, the rate of satisfied or very satisfied with the effectiveness of the treatment in the A-BPO group was 71.04% (893/1,257) and in the vehicle group was 51.20% (640/1,250). Pooled estimates revealed that a significant difference was detected between the two groups (RR=1.35, 95% CI: 1.09 to 1.66, p=0.005; Fig. 4A), with a substantial heterogeneity across the four trials (p<0.00001, I2=90%). Sensitivity analysis revealed that the study by Dreno et al.16 influenced the pooled estimates. With this study excluded, pooled estimates of the remaining three trials in a fixed-effects model still demonstrated a significant difference between the two groups (p<0.00001), indicating that A-BPO-treated patients had a higher satisfaction rate with the effectiveness.
The satisfaction measured by the question "Overall, are you satisfied with the treatment?" was also reported in four trials6,14-16. According to our meta-analysis, 576 and 252 patients (who received A-BPO [n=1,529] and vehicle [n=1,441] respectively) were satisfied or very satisfied with the treatment. Pooled estimates showed that there was a significant difference between the two groups (RR=1.35, 95% CI: 1.09 to 1.66, p=0.005; Fig. 4B), and a substantial heterogeneity was detected across the four trials (p<0.00001, I2=90%). Sensitivity analysis also revealed that the study by Dreno et al.16 influenced the pooled estimates. The exclusion of this study could eliminate the heterogeneity among the studies (p=0.34, I2=8%), and pooled estimates of the remaining three trials in a fixed effects model still revealed a significant statistical difference between the two groups (p<0.00001).
Among these included trials, three RCTs (moderate trials) compared the A-BPO with vehicle in the treatment of patients with moderate acne vulgaris5-7, two RCTs (severe trials) compared the A-BPO and doxycycline or lymecycline with vehicle and doxycycline or lymecycline in the treatment of patients with severe acne vulgaris15,16, and one RCTs (maintenance trials) compared the A-BPO with vehicle for the maintenance therapy of patients with severe acne vulgaris14. To investigate whether there was an effect with regard to the severity of acne vulgaris on the clinical results of both treatment groups, we performed a subgroup analysis.
For moderate trials, there was a significant difference regarding the success rate between the two groups (three RCTs, n=1,890, 33.06% in A-BPO group vs. 14.22% in vehicle group, p<0.00001), and there was also a significant difference between the two groups irrespective of treatment-related AEs (two RCTs, n=1,057, 27.46% in A-BPO group vs. 7.57% in vehicle group, p<0.00001) or AEs leading to discontinuation (two RCTs, n=1,670, 2.64% in A-BPO group vs. 0.72% in vehicle group, p=0.004). In addition, a significant difference between the two groups was detected with regard to satisfaction with the effectiveness (two RCTs, n=1,670, 70.62% in A-BPO group vs. 47.25% in vehicle group, p<0.00001) and overall satisfaction (one RCT, n=837, 75.89% in A-BPO group vs. 55.98% in vehicle group, p<0.00001). These pooled results are detailed in Table 3 (A).
For severe trials, no significant difference regarding the success rate was found between the two groups (two RCTs, n=837, 38.77% in A-BPO group vs. 19.81% in vehicle group, p=0.11), and there was also no significant difference between the two groups with regard to treatment-related AEs (two RCTs, n=837, 9.93% in A-BPO group vs. 10.39% in vehicle group, p=0.83) and AEs leading to discontinuation (one RCT, n=459, 0.86% in A-BPO group vs. 1.76% in vehicle group, p=0.41). Besides, there was no significant difference between the two groups in term of satisfaction with the effectiveness (two RCTs, n=837, 71.87% in A-BPO group vs. 59.18% in vehicle group, p=0.35) and overall satisfaction (two RCTs, n=837, 76.60% in A-BPO group vs. 61.11% in vehicle group, p=0.26). These pooled results are detailed in Table 3 (B).
For maintenance trials, there was a significant difference regarding the success rate between the two groups (one RCT, n=243, 70.73% in A-BPO group vs. 34.17% in vehicle group, p<0.00001); however, there was no significant difference between the two groups with regard to treatment-related AEs (one RCTs, n=243, 4.07% in A-BPO group vs. 0.83% in vehicle group, p=0.14). In addition, a significant difference between the two groups was detected regarding satisfaction with the effectiveness (one RCTs, n=243, 83.74% in A-BPO group vs. 55.00% in vehicle group, p<0.00001). These pooled results are detailed in Table 3 (C).
When compared with the vehicle gel, the A-BPO combination gel yields better clinical outcomes for the treatment of patients with moderate acne vulgaris5-7,20-22, and prevents the occurrence of relapse among patients with severe acne vulgaris14,23. Several recent studies also demonstrated that the clinical outcomes of a combination treatment using doxycycline or lymecycline and A-BPO are superior to those of doxycycline or lymecycline and vehicle in treatment of patients with severe acne vulgaris15,16,24. However, each of these trials was not large enough to confirm the outcomes within subgroups.
According to the Cochrane Handbook for systematic reviews, it is recommended to create a single pair-wise comparison in a particular meta-analysis, which combines all relevant experimental intervention groups of the study into a single group (A-BPO group), and to combine all relevant control intervention groups into a single control group (vehicle group). Therefore, the present meta-analysis was done to comprehensively compare the clinical outcomes of A-BPO combination gel with vehicle gel for the treatment or maintenance therapy of patients with moderate or severe acne vulgaris. The most important finding of the present study was that the A-BPO group yielded better clinical outcomes not only regarding the success rate (p<0.00001) but also with regard to the results of satisfaction with the effectiveness (p=0.005) and overall satisfaction (p=0.005) compared to the vehicle group. The incidence of treatment-related AEs in A-BPO group was comparable with that of vehicle group (p=0.09), while the A-BPO group was associated with a slightly increase in the incidence of AEs leading to discontinuation when compared with the vehicle group (p=0.02).
However, the chi-square test detected a substantial heterogeneity in the combined analysis of success rate (p=0.002, I2=74%), treatment-related AEs (p=0.002, I2=74%) as well as satisfaction with the effectiveness and overall satisfaction (p<0.00001, I2=90%, respectively). Sensitivity analysis revealed that the heterogeneity in the analysis of treatment-related AEs could not be eliminated, while the major contributor to the heterogeneity of the remaining three analyses was the study by Dréno et al.16. The possible explanation for this was that the sample size in this study included both patients with moderate and severe acne vulgaris, while other trials only included patients with moderate or severe acne vulgaris.
We first performed a meta-analysis ignoring the severity of acne vulgaris, which might introduce bias in the analysis. We then performed a subgroup analysis according to the severity of acne vulgaris, which showed that the A-BPO combination gel provided superior efficacy and satisfaction outcomes compared to the vehicle gel for treatment of patients with moderate acne vulgaris, despite an increased incidence of AEs. However, a combination treatment using doxycycline or lymecycline and A-BPO did not seem to yield better clinical outcomes for treatment of patients with severe acne vulgaris when compared with doxycycline or lymecycline and vehicle. But the A-BPO combination gel was more efficacious than the vehicle gel for maintenance therapy of patients with severe acne vulgaris, and the treatment was also safe and subjects were satisfied. This subgroup analysis led to the conclusion that the A-BPO combination gel is a rational choice for treatment for all but the most severe acne vulgaris, and different severity of acne vulgaris may contribute to the substantial heterogeneity in the previous combined analysis.
The present meta-analysis still has several potential limitations. One potential limitation is that the severity of acne vulgaris of patients in all of the included trials was not completely consistent, which might cause an inherent bias. A second potential limitation that exists for some included trials that used a vehicle gel as a comparator is that the side-effects could have potentially affected the blinding of both subjects and investigators, which may introduced performance bias and detection bias, respectively. A third potential limitation is that the duration of follow-up of all included trials was not long enough. In addition, as the number of included trials for this metaanalysis was relatively small, a funnel plot for pooled estimates is not performed. Thus, a publication bias cannot be excluded.
In conclusion, the present meta-analysis of RCTs reveals that A-BPO group yields better clinical outcomes such as success rate, satisfaction with the effectiveness, and overall satisfaction compared to the vehicle group, despite increased incidence of AEs leading to discontinuation. Moreover, the A-BPO combination agent most likely contributes to the treatment of moderate acne vulgaris rather than severe acne vulgaris, but may have an effect on the maintenance therapy of patients with severe acne vulgaris. However, due to a small number of eligible studies in this meta-analysis, more RCTs of high quality with a longer follow-up are needed to further confirm the clinical benefits in the treatment of the most severe acne vulgaris with the use of antibiotics in combination with A-BPO.
Figures and Tables
 | Fig. 2Forest plot of the meta-analysis for success rate. A-BPO: adapalene-benzoyl peroxide, M-H: Mantel-Haenszel, CI: confidence interval. |
 | Fig. 3Forest plot of the meta-analysis for safety outcomes. (A) Treatment-related adverse events. (B) Adverse events leading to discontinuation. A-BPO: adapalene-benzoyl peroxide, M-H: Mantel-Haenszel, CI: confidence interval. |
 | Fig. 4Forest plot of the meta-analysis for satisfaction outcomes. (A) Satisfaction with the effectiveness. (B) Overall satisfaction. A-BPO: adapalene-benzoyl peroxide, M-H: Mantel-Haenszel, CI: confidence interval. |
References
1. Pawin H, Beylot C, Chivot M, Faure M, Poli F, Revuz J, et al. Physiopathology of acne vulgaris: recent data, new understanding of the treatments. Eur J Dermatol. 2004; 14:4–12.
2. Gollnick HP, Finlay AY, Shear N. Global Alliance to Improve Outcomes in Acne. Can we define acne as a chronic disease? If so, how and when? Am J Clin Dermatol. 2008; 9:279–284.
3. Leyden JJ. A review of the use of combination therapies for the treatment of acne vulgaris. J Am Acad Dermatol. 2003; 49:3 Suppl. S200–S210.

4. Gollnick H, Cunliffe W, Berson D, Dreno B, Finlay A, Leyden JJ, et al. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003; 49:1 Suppl. S1–S37.
5. Thiboutot DM, Weiss J, Bucko A, Eichenfield L, Jones T, Clark S, et al. Adapalene-benzoyl peroxide, a fixed-dose combination for the treatment of acne vulgaris: results of a multicenter, randomized double-blind, controlled study. J Am Acad Dermatol. 2007; 57:791–799.

6. Gollnick HP, Draelos Z, Glenn MJ, Rosoph LA, Kaszuba A, Cornelison R, et al. Adapalene-benzoyl peroxide, a unique fixed-dose combination topical gel for the treatment of acne vulgaris: a transatlantic, randomized, double-blind, controlled study in 1670 patients. Br J Dermatol. 2009; 161:1180–1189.

7. Gold LS, Tan J, Cruz-Santana A, Papp K, Poulin Y, Schlessinger J, et al. A North American study of adapalene-benzoyl peroxide combination gel in the treatment of acne. Cutis. 2009; 84:110–116.
8. Pariser DM, Westmoreland P, Morris A, Gold MH, Liu Y, Graeber M. Long-term safety and efficacy of a unique fixed-dose combination gel of adapalene 0.1% and benzoyl peroxide 2.5% for the treatment of acne vulgaris. J Drugs Dermatol. 2007; 6:899–905.

10. Michel S, Jomard A, Démarchez M. Pharmacology of adapalene. Br J Dermatol. 1998; 139:Suppl 52. 3–7.

11. Shroot B, Michel S. Pharmacology and chemistry of adapalene. J Am Acad Dermatol. 1997; 36:S96–S103.

12. Bikowski JB. Clinical experience results with clindamycin 1% benzoyl peroxide 5% gel (Duac) as monotherapy and in combination. J Drugs Dermatol. 2005; 4:164–171.
13. Martin B, Meunier C, Montels D, Watts O. Chemical stability of adapalene and tretinoin when combined with benzoyl peroxide in presence and in absence of visible light and ultraviolet radiation. Br J Dermatol. 1998; 139:Suppl 52. 8–11.

14. Poulin Y, Sanchez NP, Bucko A, Fowler J, Jarratt M, Kempers S, et al. A 6-month maintenance therapy with adapalene-benzoyl peroxide gel prevents relapse and continuously improves efficacy among patients with severe acne vulgaris: results of a randomized controlled trial. Br J Dermatol. 2011; 164:1376–1382.

15. Gold LS, Cruz A, Eichenfield L, Tan J, Jorizzo J, Kerrouche N, et al. Effective and safe combination therapy for severe acne vulgaris: a randomized, vehicle-controlled, double-blind study of adapalene 0.1%-benzoyl peroxide 2.5% fixed-dose combination gel with doxycycline hyclate 100 mg. Cutis. 2010; 85:94–104.
16. Dréno B, Kaufmann R, Talarico S, Torres Lozada V, Rodríguez-Castellanos MA, Gómez-Flores M, et al. Combination therapy with adapalene-benzoyl peroxide and oral lymecycline in the treatment of moderate to severe acne vulgaris: a multicentre, randomized, double-blind controlled study. Br J Dermatol. 2011; 165:383–390.

17. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.0.2 [Internet]. London: The Cochrane Collaboration;2008. updated September 2009. Available via DIALOG from: http://www.cochranehandbook.org.
18. Loesche C, Pernin C, Poncet M. Adapalene 0.1% and benzoyl peroxide 2.5% as a fixed-dose combination gel is as well tolerated as the individual components alone in terms of cumulative irritancy. Eur J Dermatol. 2008; 18:524–526.
19. Andres P, Pernin C, Poncet M. Adapalene-benzoyl peroxide once-daily, fixed-dose combination gel for the treatment of acne vulgaris: a randomized, bilateral (split-face), dose-assessment study of cutaneous tolerability in healthy participants. Cutis. 2008; 81:278–284.
20. Eichenfield LE, Jorizzo JL, Dirschka T, Taub AF, Lynde C, Graeber M, et al. Treatment of 2,453 acne vulgaris patients aged 12-17 years with the fixed-dose adapalene-benzoyl peroxide combination topical gel: efficacy and safety. J Drugs Dermatol. 2010; 9:1395–1401.
21. Feldman SR, Tan J, Poulin Y, Dirschka T, Kerrouche N, Manna V. The efficacy of adapalene-benzoyl peroxide combination increases with number of acne lesions. J Am Acad Dermatol. 2011; 64:1085–1091.

22. Tan J, Gollnick HP, Loesche C, Ma YM, Gold LS. Synergistic efficacy of adapalene 0.1%-benzoyl peroxide 2.5% in the treatment of 3855 acne vulgaris patients. J Dermatolog Treat. 2011; 22:197–205.

23. Tan J, Stein Gold L, Schlessinger J, Brodell R, Jones T, Cruz A, et al. Short-term combination therapy and long-term relapse prevention in the treatment of severe acne vulgaris. J Drugs Dermatol. 2012; 11:174–180.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download