Abstract
Sebaceous carcinoma is a very rare and potentially aggressive carcinoma originating from the epithelial lining of the sebaceous gland. More than 70% of all cases are in the head and neck region, especially the periorbita; therefore, they are classified into ocular and extraocular sebaceous carcinoma. The reported risk factors are advanced age, male sex, previous irradiation, and genetic predisposition for Muir-Torre syndrome. The current case is of sebaceous carcinoma found in the suprapubic area of a 67-year-old male patient who had received liver transplantation 6 years before, and had been receiving oral tacrolimus. Examination of the gastrointestinal system did not reveal any other malignancies. Although nonmelanoma skin cancers may occur as a complication after liver transplantation, there have been no previous reports of sebaceous carcinoma after liver transplantation. Furthermore, the sebaceous carcinoma in this case occurred in an uncommon location. We report this case along with a review of the literature.
Sebaceous carcinoma is a rare, potentially aggressive cutaneous malignancy that differentiates from the epithelial lining of the sebaceous gland1,2,3. It predominantly occurs in the periocular region, and masquerades as other benign or malignant lesions, leading to a delayed diagnosis4. More than 70% of sebaceous carcinomas occur in the head and neck region, with other areas of occurrence being the skin of the trunk, upper limb and shoulder, lower limb and hip, genitalia, and descending colon2.
The reported risk factors include advanced age, history of irradiation to the head and neck, and a genetic predisposition for Muir-Torre syndrome (MTS) or possibly familial retinoblastoma3,5. There have been several reports of sebaceous carcinoma occurring after kidney transplantation6,7. The pathogenesis of sebaceous carcinoma is thought to be related to immunosuppression, through changes either in host immunity or via independent mechanisms involving the immunosuppressant drug. Calcineurin inhibitors may enhance tumor development independent of host immunity8.
Herein, we describe a unique case of a solitary sebaceous carcinoma occurring in a patient who underwent liver transplantation, with a review of the literature.
A 67-year-old male patient presented with a protruding suprapubic mass in the upper margin of his pubic hair. The lesion had started as a small nodule 1.5 years before, and the punch biopsy performed 2 weeks before his presentation led to a diagnosis of sebaceous epithelioma. He had undergone cadaveric donor liver transplantation 6 years before for hepatocellular carcinoma and liver cirrhosis owing to type C hepatitis. He was receiving oral tacrolimus as an outpatient.
On physical examination, a round, protruding sessile mass with a 3-cm diameter was observed at the cranial region of the pubic hair. The mass was pinkish with uneven purplish areas and ulcerated on its right upper surface. It was well circumscribed, rubbery, and movable, with the base easily palpable deep in the skin. The patient did not report any pain. No tenderness or signs of surrounding infection were noted (Fig. 1).
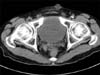
Computed tomography of the pelvic area revealed an oval fat-containing skin nodule measuring 2 cm in diameter, in the left lower abdominal wall (Fig. 2). The patient refused magnetic resonance imaging because of cost issues.
The excision was performed with the patient in supine position, as an elliptical incision line with a horizontal axis distanced at the closest 5-mm margin from the mass to prevent dog-ear deformity when excising along the suprapubic area. Full-thickness skin incision and dissection of the mass from the surrounding subcutaneous tissues were performed with the patient under local anesthesia. The mass was well circumscribed and rubbery, and no particular increase in surrounding vascularity was noted (Fig. 3). Further excision was not performed because of the preoperative biopsy results of sebaceous epithelioma and the well-defined characteristics of the mass.
Histopathological analysis revealed a multilobular tumor composed of basaloid cells at the periphery of lobules, with vacuolated cells presenting sebaceous differentiation in its central area. The tumor was well encapsulated and mostly well differentiated, but showed an area of regional matrix invasion. This portion showed an increase in the number of basaloid cells, nuclear atypism, and a decrease in sebocyte differentiation (Fig. 4). Histopathological findings suggested a diagnosis of sebaceous carcinoma.
Examinations of the gastrointestinal tract, including endoscopy and colonoscopy, were performed to search for additional visceral tumors and rule out the possibility of MTS. Positron emission topography was also performed, and no underlying malignancies were detected in any of these evaluations. Radiation therapy with a total dose of 54 Gy was delivered in 27 fractions as an adjuvant therapy after surgery. The patient was followed-up for 6 months after the operation, with no evidence of recurrence. Short-term follow-up is still being performed.
Sebaceous carcinoma is a rare, potentially aggressive cutaneous malignancy1,2. It usually occurs in the periocular region where there is an abundance of sebaceous glands, and has a diverse spectrum of clinical presentations that delay diagnosis9. The most common finding is a gradually enlarging, firm nodule10. Histopathological examination is the only definitive diagnostic method for sebaceous carcinoma. The disease is classified as either ocular or extraocular depending on the location of the primary lesion, with extraocular lesions accounting for 25% of the total cases. These 2 tumor types are known to have a similar prognosis2.
Reported risk factors include advanced age, history of irradiation to the head and neck, and possibly familial retinoblastoma. Furthermore, sebaceous carcinoma is commonly associated with a genetic predisposition for MTS, an autosomal dominant hereditary disease characterized by the association of a skin tumor of sebaceous lineage, with or without a keratoacanthoma associated with one or more visceral neoplasms3,5. Several cases have been reported after kidney transplantation and immunosuppression6,7.
The pathogenesis of sebaceous carcinoma occurring in other reported organ transplant recipients is thought to be through the somatic mutation of deoxyribonucleic acid (DNA) mismatch repair genes due to the effects of immunosuppressants. Some recipients may have had undetected MTS that is unmasked by the use of immunosuppressants. An association between microsatellite instability and sebaceous carcinoma in immunosuppressed patients who underwent organ transplantation and who do not have MTS has been suggested11. Kaminska et al.7 reported a case of sebaceous carcinoma mixed with sebaceous adenoma after kidney transplantation, suggesting the possibility of a sebaceous adenoma-sebaceous carcinoma neoplastic sequence. The present patient also had a specimen consisting mostly of well-differentiated sebaceous gland-forming sebocytes, with a focal region of infiltrative growth, mitotic figures, pleomorphic nuclei, and atypia, all of which may implicate a similar pathological sequence.
The patient in this report was a liver transplant recipient and had been receiving oral tacrolimus, a calcineurin inhibitor related to enhanced tumor development. Immunosuppressive drugs reduce immune surveillance and some even exert a carcinogenic effect. Cyclosporine and tacrolimus are calcineurin inhibitors, and have been hypothesized to increase tumor growth through the increase of transforming growth factor (TGF)-β, and interleukin-6, and by accelerating angiogenesis through elevated levels of vascular endothelial growth factor12. Maluccio et al.13 found that tacrolimus has a dose-dependent effect on tumor progression and TGF-β1 expression in mice. TGF-β1 is a multifunctional cytokine related to tumor invasiveness and metastatic progression.
In Western countries, the most frequently diagnosed malignancy after liver transplantation is nonmelanoma skin cancer (NMSC)14. However, Asians have a lower incidence of skin cancer in the general population, and a relatively low incidence of NMSC after organ transplantations. Stomach cancer, followed by colorectal cancer, was the most frequently observed de novo malignancy after liver transplantation in the Korean population, in a study reported by Park et al.15. De novo sebaceous carcinoma occurring in a liver transplant recipient has never been reported in the literature.
The mainstay treatment for sebaceous carcinoma consists of wide excisions with margins of 5 to 6 mm and frozen section control to confirm sufficient margins16. There have been no reports on the difference of safety margins between ocular and extraocular sebaceous lesions. Mohs micrographic surgery has been considered a useful method by some authors16. Radiation therapy is used in medically inoperable patients; however, the optimal dosage has not been established. Some reports suggest that radiotherapy is useful in controlling microscopic disease, as an adjuvant therapy17. The clinical utility of sentinel node biopsy has not been established18.
There have been several reports of sebaceous carcinoma occurring after kidney transplantation, but none in a liver transplant recipient. Sebaceous carcinoma should always be considered when a patient presents with a newly noticed skin lesion after any organ transplantation.
Figures and Tables
 | Fig. 1A pink, well-circumscribed suprapubic mass with a diameter of 3 cm. Ulceration is seen on its right upper surface. |
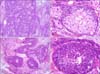 | Fig. 4Histopathological findings. (A) The well-differentiated areas show small lobular aggregations of sebocytes (H&E, ×40). (B) The margins consist of basaloid cells and the central portions are fully differentiated vacuolated sebocytes, as in normal sebaceous glands (H&E, ×400). (C) Poorly differentiated areas have high cellularity and invasion into the surrounding tissue (H&E, ×40). (D) Atypism (nuclear pleomorphism, prominent nucleoli, high nucleus-to-cell ratio) is seen, and mitosis is observed, with almost no differentiation into normal sebocytes (H&E, ×400). |
References
1. Jo MS, Kwon KH, Shin HK, Choe J, Jang TJ. Sebaceous carcinoma arising from the nevus sebaceous. Arch Plast Surg. 2012; 39:431–433.

2. Dasgupta T, Wilson LD, Yu JB. A retrospective review of 1349 cases of sebaceous carcinoma. Cancer. 2009; 115:158–165.

3. Chao AN, Shields CL, Krema H, Shields JA. Outcome of patients with periocular sebaceous gland carcinoma with and without conjunctival intraepithelial invasion. Ophthalmology. 2001; 108:1877–1883.

4. Sakol PJ, Simons KB, McFadden PW, Harris GJ, Massaro BM, Koethe S. DNA flow cytometry of sebaceous cell carcinomas of the ocular adnexa: introduction to the technique in the evaluation of periocular tumors. Ophthal Plast Reconstr Surg. 1992; 8:77–87.
5. Kivelä T, Asko-Seljavaara S, Pihkala U, Hovi L, Heikkonen J. Sebaceous carcinoma of the eyelid associated with retinoblastoma. Ophthalmology. 2001; 108:1124–1128.

6. Harwood CA, McGregor JM, Swale VJ, Proby CM, Leigh IM, Newton R, et al. High frequency and diversity of cutaneous appendageal tumors in organ transplant recipients. J Am Acad Dermatol. 2003; 48:401–408.

7. Kaminska EC, Iyengar V, Tsoukas M, Shea CR. Borderline sebaceous neoplasm in a renal transplant patient without Muir-Torre syndrome. J Cutan Pathol. 2013; 40:336–340.

8. Euvrard S, Morelon E, Rostaing L, Goffin E, Brocard A, Tromme I, et al. TUMORAPA Study Group. Sirolimus and secondary skin-cancer prevention in kidney transplantation. N Engl J Med. 2012; 367:329–339.

9. Gaskin BJ, Fernando BS, Sullivan CA, Whitehead K, Sullivan TJ. The significance of DNA mismatch repair genes in the diagnosis and management of periocular sebaceous cell carcinoma and Muir-Torre syndrome. Br J Ophthalmol. 2011; 95:1686–1690.

10. Nelson BR, Hamlet KR, Gillard M, Railan D, Johnson TM. Sebaceous carcinoma. J Am Acad Dermatol. 1995; 33:1–15. quiz 16-18.

11. Harwood CA, Swale VJ, Bataille VA, Quinn AG, Ghali L, Patel SV, et al. An association between sebaceous carcinoma and microsatellite instability in immunosuppressed organ transplant recipients. J Invest Dermatol. 2001; 116:246–253.

12. Guba M, Graeb C, Jauch KW, Geissler EK. Pro- and anti-cancer effects of immunosuppressive agents used in organ transplantation. Transplantation. 2004; 77:1777–1782.

13. Maluccio M, Sharma V, Lagman M, Vyas S, Yang H, Li B, et al. Tacrolimus enhances transforming growth factor-beta1 expression and promotes tumor progression. Transplantation. 2003; 76:597–602.

14. Euvrard S, Kanitakis J, Claudy A. Skin cancers after organ transplantation. N Engl J Med. 2003; 348:1681–1691.

15. Park HW, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. De novo malignancies after liver transplantation: incidence comparison with the Korean cancer registry. Transplant Proc. 2012; 44:802–805.

16. Buitrago W, Joseph AK. Sebaceous carcinoma: the great masquerader: emgerging concepts in diagnosis and treatment. Dermatol Ther. 2008; 21:459–466.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download