Abstract
Background
A variety of hyaluronic acid (HA) fillers demonstrate unique physical characteristics, which affect the quality of the HA filler products. The critical factors that affect the degradation of HA gels have not yet been determined.
Objective
Our objective was to determine the characteristics of HA gels that affect their resistance to the degradation caused by radicals and enzymes.
Methods
Three types of HA fillers for repairing deep wrinkles, Juvederm Ultra Plus (J-U), Restylane Perlane (Perlane), and Cleviel, were tested in this study. The resistance of these HA fillers to enzymatic degradation was measured by carbazole and displacement assays using hyaluronidase as the enzyme. The resistance of these fillers to radical degradation was measured by the displacement assay using H2O2.
Results
Different tests for evaluating the degradation resistance of HA gels can yield different results. The filler most susceptible to enzymatic degradation was J-U, followed by Perlane and Cleviel. The HA filler showing the highest degree of degradation caused by H2O2 treatment was Perlane, followed by J-U, and then Cleviel. Cleviel showed higher enzymatic and radical resistances than J-U and Perlane did. Furthermore, it exhibited the highest resistance to heat and the lowest swelling ratio among all the fillers that were examined.
Currently, soft tissue augmentation by fillers is widely accepted as a treatment for improving the quality of life. Fillers are prepared from diverse materials, including autologous implants, collagens, hyaluronic acids (HAs), and biosynthetic polymers, which are marketed for cosmetic purposes1. Among those fillers, HA fillers have gained the widest popularity due to their volumizing effect, biocompatibility, and easy correction after treatment.
HA is a polysaccharide consisting of disaccharide units of D-glucuronic acid and N-acetyl-D-glucosamine with β-(1→4) glycosidic linkages. HA is a major component of connective tissues abundant especially in the human dermis2,3. However, natural HA can be rapidly degraded by enzymes and radicals existing in the human body. The half life of HA in human tissues generally ranges from 1 to 2 days; therefore, the effect of the treatment for dermal defects such as wrinkles via the injection of free HA into skin only lasts for less than a week4. Despite the excellent biocompatibility of HA, its time-dependent degradation is a severe drawback for its applications. To overcome the limitation of lack of persistence of free HA, HA-based dermal fillers have been produced by chemical modification process, namely crosslinking. HA can be cross-linked by using diverse cross-linking reagents such as 1,4-butanediol diglycidyl ether (BDDE), divinyl sulfone, or diazomethane. Among these agents, BDDE has gained the greatest popularity due to its safety and convenient operation2,3. Although all HA fillers appear to have similar functionality, their physical characteristics and manufacturing methods are distinct. The concentrations of HA and free (unmodified) HA, types and extents of crosslinking, and particle sizes are all different for preparing various HA fillers. Moreover, these factors contribute to essential gel properties such as cohesiveness, hardness, and swelling ratio, which can determine the quality of the final product by affecting its resistance to degradation and usability2,5,6.
Several studies have been conducted to reveal the essential properties of HA gels that affect their rate of degradation. Some reported that the HA content, degree of crosslinking, and cohesive properties of the filler contributed to the degradation resistance7,8. Others reported that the type and extent of crosslinking, gel concentration, and degree of swelling determined the degradation rate of cross-linked HA hydrogels5,9. In addition to the aforementioned factors, it is likely that other attributes are also accountable for the degradation of HA gels. In this study, we investigated three different types of HA fillers and determined the characteristics of HA gels that could affect their resistance to degradation caused by radicals and enzymes.
One monophasic filler (Juvederm Ultra Plus; Allergan Inc., Irvine, CA, USA) and two types of biphasic HA fillers (Restylane Perlane, Q-Med, Uppsala, Sweden; and Cleviel, Pacific Pharm., Seoul, Korea) were tested in this study (Table 1). Both Juvederm Ultra Plus (J-U) and Restylane Perlane (Perlane) contain HA obtained from Streptococcus equi and formulated to a concentration of 24 and 20 mg/ml, respectively. Cleviel (PP-501deep), newly developed HA filler, was manufactured by a novel solid phase crosslinking technology. In this approach, free HA was cross-linked by dissolving it in NaOH solution with BDDE. The solution was then mixed properly and dried in a vacuum oven at 25℃ for 24 hours. Afterwards, the gel was washed and re-dried in the vacuum oven to yield a dry HA matrix, which was ground into a powder. The high molecular weight free HA solution was combined with the HA powder to improve the injectability of the filler. The final product was loaded into the syringes that were then autoclaved.
In cytotoxicity tests, 1 ml of each of HA filler was eluted in 5 ml of opti-MEM media (Gibco, Carlsbad, CA, USA) at 37℃ with 5% CO2 for 72±2 hours to produce the effluent. Approximately 1×104 of L-929 mouse fibroblast cells were seeded into each well of a 96-well plate and cultured overnight. After incubation, the cells were treated with the filler effluent diluted into a concentration of 100, 50, or 25% for 24 hours. The viable cells were quantified using the WST-1 assay at a wavelength of 450 nm.
In the degradation tests, 0.2 ml of each HA filler was added into 5 ml of phosphate buffered saline (pH 7.0). The solution was then incubated with hyaluronidase at the concentration of 10 and 20 IU/mg in an incubator agitated at 100 rpm at 37℃ for 8 hours. The reaction was stopped by the addition of 0.1 N HCl (2 ml) to the solution. The solution was then filtered through a 0.45-µm filter, and the remaining HA was quantified by the carbazole assay10. In addition, we used a modified displacement assay to measure the resistance of HA fillers to enzymatic degradation11. With the use of this assay, we were able to determine the rate of the viscosity change in the HA gel placed between the enzyme and the dye layers by measuring the diffusion velocity of the dye in the gel layer. In this approach, 20 µl of Coomassie blue (1 mM) was loaded into the bottom of a 1.5-ml eppendorf (EP) tube, which was then filled with 0.1 ml of HA filler, followed by the addition of hyaluronidase solution at a concentration of 35 IU per 1 mg of HA gel. After 3, 6, 12, and 24 hours of reaction, the absorbance of hyperphase solution was read separately at 590 nm using a spectrophotometer (Synergy2; BioTek instrument Inc., Winooski, VT, USA).
A dry-type Yellow 203 dye was placed at the bottom of an EP tube, which was then filled with 0.1 ml of the HA filler. Afterwards, 0.35 ml of H2O2 (250 or 500 mM) was loaded on top of the HA filler. After 1, 3, and 4.5 hours of reaction, the absorbance of hyperphase solution was measured separately at 410 nm using a spectrophotometer.
Most HA dermal fillers are viscoelastic; in other words, they contain both elastic (solid) and viscous (liquid) components. The rheological property of HA fillers can be described by a complex modulus G*, which is defined as the sum of storage modulus G' and loss modulus G'', also known as elastic and viscous modulus, respectively. The storage modulus G' is often used to characterize the rigidity of a gel5, and a stiffer material has a higher G' and a softer material has a lower G'. When a filler is exposed to high temperatures, the phosphate in PBS can generate radicals. Therefore, we can indirectly determine the resistance of filler to radicals by measuring the corresponding G' value.
The gel-loading syringes were placed in an oven for 24 hours, and then the G' and G'' values were measured using a rheometer (AR 2000; TA Instruments Inc., New Castle, DE, USA) for determining δ=G''/G'. All the measurements were performed using a 20-mm steel plate oscillating at a frequency between 0.01 Hz and 10 Hz under a stress of τ=1 Pa. The presented values were obtained at the frequency of 1 Hz and were compared with the results obtained from the untreated syringes.
The viability of L929 mouse fibroblast cells treated with the effluents of HA fillers was greater than 90% (Table 2). None of the HA fillers showed any toxicity to cells. In the measurement of resistance to enzymatic degradation, about 76.9% of J-U, 60.5% of Perlane, and 32.4% of Cleviel were degraded by hyaluronidase at 10 IU/mg HA (Fig. 1). Almost 100% of 20 IU/mg HA fillers were degraded by hyaluronidase after 8 hours of reaction. In the displacement assay, 53.0% of J-U, 50.9% of Perlane, and 31.7% of Cleviel were degraded after 24 hours of reaction (Fig. 2A). Furthermore, the radical resistance tests revealed that 96.0% of Perlane, 70.4% of J-U, and 57.1% of Cleviel were degraded by treatment with H2O2 (Fig. 2B). These results indicate that Cleviel exhibits larger enzymatic and radical resistances than J-U and Perlane do. After 24 hours of heating, the G' values of J-U, Perlane, and Cleviel decreased by 50.9%, 38.8%, and 1.2%, respectively (Table 3), indicating the lowest heat resistance of J-U and the highest resistance of Cleviel among all the tested fillers.
Three days post-injection, the isolated HA fillers were removed from the dorsa of the hairless mice for evaluating the filler swelling effect. The weight of J-U, Perlane, and Cleviel after injection increased by 340% 162% and 105%, respectively, as compared with their original weights (Fig. 3). These results indicate that the swelling of injected HA fillers is caused by the absorbance of surrounding body fluids, and the monophasic HA filler, J-U, shows a higher degree of swelling than the biphasic fillers do.
Despite its well-addressed functionality as a component of biological tissues, HA can be toxic to cells when present at an extremely high concentration in normal tissues. We, therefore, tested the toxicity of Cleviel, whose HA concentration was 2-fold higher than that of the other commercial products. Our results confirmed that none of the HA fillers at the examined concentrations showed any toxicity to cells.
Different degradation tests can produce different results depending on the characteristics of the HA gels under examination. The test performed in an enzyme or radical solution mimics the relevant physiological condition, where individual HA particles are surrounded by the biological tissue or body fluid after their introduction into the human body. The displacement assay in our study uses a simple lumped-mass model for evaluating the degradation rate of HA gels11. The thermostability measurement focuses on the stability of HA component alone rather than its relationship with the endogenous enzymes or radicals. This test represents the decomposition process of HA gels, where no external material transfer is involved.
Hyaluronidase and radicals are the main factors causing the degradation of HA gels. Hyaluronidase is a huge molecule with a mass of 50 kDa, and can specifically decompose HA chains after being activated by the carboxyl acid of D-glucuronic acid, and cleave β 1,4-glucosaminidic bonds12. Thus, the physical binding of hyaluronidase to HA is needed for initiating the decomposition process. Furthermore, to generate rapid decomposition, a sufficient amount of hyaluronidase and enough space for hyaluronidase to recognize its binding site on HA molecule is required. In contrast, radicals do not show any selectivity and have a low molecular weight. The effect of HA concentration on the enzymatic degradation rate is much more significant than that of the inter-matrix space on the radical-based degradation4. In our study, Cleviel demonstrated the highest resistance to enzymatic decomposition, followed by Perlane and J-U.
The obtained results may be caused by the different particle sizes, degrees of crosslinking, and/or concentrations of HA in the fillers. Normally, the products consisting of smaller gel particles will degrade faster in the body than those containing larger particles. However, the particles used in the dermal fillers currently approved in the US have a limited size range. Therefore, the size of gel particles is unlikely to induce the observed differences in enzymatic degradation of HA fillers4,9. In general, the swelling ratio of a material decreases with the increase in the degree of crosslinking and HA concentration. The swollen gel networks have also been shown to decrease in size through degradation and exposure to hyaluronidase13. Therefore, we can assume that the degradation rates of HA gels may be associated with their swelling ratios.
We were unable to determine the rate of radical-mediated HA gel degradation using the conventional carbazole assay, because its reproducibility and sensitivity were insufficient for producing repeatable data. Instead, by using the displacement assay, we were able to quantitatively measure the HA degradation caused by both enzymes and radicals, because the method measured the dye concentration instead of the HA concentration. To maintain the shape and integrity of bulk HA gel over time, either a very small space or a highly viscous solution between the HA gel particles is preferable to prevent the external degradation materials from reaching the gel particles7,8. J-U is a monophasic HA filler with very small spaces between the gel particles. Therefore, the dye diffusion rate in the J-U filler would be smaller than that in the biphasic HA fillers. As expected, the initial dye diffusion rate in J-U was smaller than that in Perlane; however, the rates became comparable after 24 hours of HA degradation. Furthermore, we found that the dye dispersion rate in J-U was larger than that in the biphasic filler Cleviel after 24 hours of reaction. The slow degradation of J-U during the initial phase might be due to the viscous property of the monophasic gel filler. Whereas, J-U showed the lowest G' value (1/3 that of the biphasic fillers) among all the filler materials, indicating its highly deformable property. Furthermore, the rapid degradation of high-viscosity solution between J-U particles increases the particle distance, indicating that the resistance of HA gel particles also contributes to the resistance of gel block.
The high resistance of bulk Cleviel to degradation can be explained by the densely packed gel particles in the filler structure, which can retard the penetration of enzymes and radicals. This structure results from the combinative effect of a high HA concentration and high degree of crosslinking, i.e., a low swelling ratio. Thus, the main factor causing the high degradation resistance of Cleviel gel particles is the low gel swelling ratio due to its densely packed particle structure.
In the present study, we tested and compared different types of HA fillers to determine the essential physical characteristics that could retard the enzyme- or radicalinduced HA gel degradation. We found that a decrease in the gel-swelling ratio would lead to a retarding effect on the degradation of HA fillers.
Figures and Tables
Fig. 1
Resistance to enzymatic degradation measured by carbazole assay. Hyaluronic acid (HA) fillers diluted in phosphate buffered saline were incubated with hyaluronidase at 10 IU/mg HA (blue bar) and 20 IU/mg HA (pink bar) for 8 hours. The remaining HA was then quantified by the carbazole assay. SE: standard error. *p<0.05 as compared with Juvederm Ultra Plus.
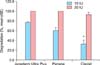
Fig. 2
Resistance to enzymatic degradation (A) and radical degradation (B) measured by displacement assay. (A) Hyaluronic acid (HA) fillers were incubated with hyaluronidase at 35 IU/mg HA. After 3, 6, 9, 12 and 24 hours of reaction, the absorbance of the hyperphase solution was measured at 590 nm. (B) HA fillers were treated by 500 mM H2O2. After 1, 3 and 4.5 hours of reaction, the absorbance of the hyperphase solution was measured at 410 nm. SE: standard error. *p<0.05 as compared with Juvederm Ultra Plus. #p<0.05 as compared with Perlane.

Fig. 3
Post-swelling effect of hyaluronic acid (HA) fillers in hairless mouse. After injection of 0.2 ml of HA fillers into hairless mouse, the weight of isolated HA fillers from sacrificed mice was measured 3 days after injection. SE: standard error. *p<0.05, **p<0.01 as compared with Juvederm Ultra Plus. #p< 0.05, ##p<0.01 as compared with Perlane.

References
1. Buck DW 2nd, Alam M, Kim JY. Injectable fillers for facial rejuvenation: a review. J Plast Reconstr Aesthet Surg. 2009; 62:11–18.

2. Beasley KL, Weiss MA, Weiss RA. Hyaluronic acid fillers: a comprehensive review. Facial Plast Surg. 2009; 25:86–94.

3. Volpi N, Schiller J, Stern R, Soltés L. Role, metabolism, chemical modifications and applications of hyaluronan. Curr Med Chem. 2009; 16:1718–1745.

4. Hahn SK, Park JK, Tomimatsu T, Shimoboji T. Synthesis and degradation test of hyaluronic acid hydrogels. Int J Biol Macromol. 2007; 40:374–380.

5. Ibrahim S, Kang QK, Ramamurthi A. The impact of hyaluronic acid oligomer content on physical, mechanical, and biologic properties of divinyl sulfone-crosslinked hyaluronic acid hydrogels. J Biomed Mater Res A. 2010; 94:355–370.

6. Bogdan Allemann I, Baumann L. Hyaluronic acid gel (Juvéderm) preparations in the treatment of facial wrinkles and folds. Clin Interv Aging. 2008; 3:629–634.
7. Jones D, Tezel A, Borrell M. In vitro resistance to degradation of hyaluronic acid dermal fillers by ovine testicular hyaluronidase. Dermatol Surg. 2010; 36:804–809.

8. Sall I, Férard G. Comparison of the sensitivity of 11 cross-linked hyaluronic acid gels to bovine testis hyaluronidase. Polym Degrad Stab. 2007; 92:915–919.

9. Kablik J, Monheit GD, Yu L, Chang G, Gershkovich J. Comparative physical properties of hyaluronic acid dermal fillers. Dermatol Surg. 2009; 35:Suppl 1. 302–312.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download