Abstract
Background
It is difficult to achieve satisfactory results with the traditional treatment of large-area skin defects and deep burns.
Objective
To test the treatment effect of an active dressing film made of a mixture of fibrin glue and bone marrow mesenchymal stem cells (BMSCs) for repairing burn wounds on the skin of rats.
Methods
Two scald wounds were made on the back of each rat. A total of 30 scald wounds were randomly divided into 3 groups, with 10 wounds in each group. In the experimental treatment group, the scald wounds were covered with the fibrin glue and BMSC mixture. The wounds of the experimental control group were covered with fibrin glue only. No intervention was administered to the blank control group. Thirty days after treatment, pathological sections were cut from the scalded local tissues of all rats from the 3 groups and observed with a microscope.
Results
The speed of scald wound healing in the experimental treatment group was faster than the other 2 groups. In the experimental treatment group, histopathological analysis revealed that the sebaceous glands showed obviously proliferous at the edge of the new tissue and gradually extended to the deep dermal layer of the new tissue.
Conclusion
BMSCs may have an active role in promoting skin tissue repair and generating skin appendages. Allogeneic BMSCs mixed with fibrin glue can contribute to the quick formation of a film-like gel over the scald wounds, which might be of significance for emergency treatment and skin-grafting operations.
Large-area skin defects and deep burns are difficult to treat with satisfactory clinical results. Although a variety of skin substitutes currently used in the clinic have some effects in the early period of treatment of severe scald or burn injuries, they cannot be used as permanent skin substitutes owing to their lack of dermal and epidermal structures and skin appendages1,2,3. Stem cell technology along with the development of tissue engineering technology can now provide new ways to promote wound healing. Many researchers are beginning to develop tissue-engineered skin for repairing skin defects and scald wounds4,5,6. The key to tissue engineering is the choice of a scaffold and seed cells. Bone marrow mesenchymal stem cells (BMSCs) can differentiate into a variety of tissues, including tendons and ligament, as well as cells, including osteoblasts, cartilaginous cells, and nerve cells7. Owing to the ease of isolation, culture, and proliferation, as well as the low rate of graft rejection of BMSCs, these cells are now the focus of cell biology and tissue engineering research. Fibrin glue has been used widely in biomedical fields as a natural macromolecular material with excellent biocompatibility8,9,10,11. In the present experiment, we chose rat BMSCs as the seed cells and fibrin glue as the scaffold. Fibrin glue and rat BMSCs were mixed to produce an active dressing film, which was used to repair burn wounds on the skin of rats. We expected the mixture to promote skin tissue repair and the generation of skin appendages.
All experiments were conducted in conformity with the institutional guidelines of the Zhejiang Academy of Medical Sciences, Hangzhou, China, and the National Institutes of Health Guide for Care and Use of Laboratory Animals for the care and use of laboratory animals. Four 1-day-old Sprague-Dawley (SD) rats were used as the sources of BMSCs, and 15 adult rats were used to make scald animal models for allogeneic BMSC transplantation. The mean weight of the adult rats was 150 g. For histological analyses, 15 rats were killed 30 days after transplantation.
Isolation of primary rat BMSCs was performed as follows: 1-day-old SD rats were anesthetized and decapitated to obtain the femur and tibia with a sterile operation. After being washed with phosphate buffered saline (PBS) containing 1% (v/v) penicillin and gentamicin, the tissues were chopped into small pieces and immersed in 2 ml of low-glucose Dulbecco's modified Eagle's medium (LG-DMEM, Invitrogen; Gibco, Grand Island, NY, USA). After complete mixing, the obtained suspension was filtered through a 200-mesh sieve. The cell suspension was plated on 24-well culture plates (Corning, Corning, NY, USA) with complete culture medium (LG-DMEM supplemented with 10% [v/v] fetal bovine serum [FBS], 100 U/ml of penicillin, and 100 mg/ml of gentamicin), which was incubated at 37℃ with 5% of humidified CO2. The culture medium was changed every 2 days. Cells within the sixth passage were used in the present study.
For chondrocyte differentiation, fourth-passage cells were cultureded on a 3.5-cm-diameter dish (Corning) with complete culture medium of LG-DMEM until the cells reached 80% confluence. Then, the medium was replaced with a chondrogenesis medium comprising high-glucose DMEM (HG-DMEM, Invitrogen) supplemented with 10 µg/L of transforming growth factor-β1 (PeproTech, Rocky Hill, NJ, USA), 4×10-5 g/L dexamethasone (Sigma-Aldrich, St. Louis, MO, USA), 0.05 g/L of ascorbic acid, 4.32 g/L of β-glycerophosphate, 2×10-3 g/L of insulin (Sigma-Aldrich), 0.10 g/L of pyruvate, 1.50 g/L of bovine serum albumin (BSA), 3% (v/v) of FBS, 1% (v/v) of penicillin and gentamicin. The medium was changed every 2 days. After 28 days of culture, the BMSCs were stained with toluidine blue O (Sigma-Aldrich) and observed by using microscopy.
For osteoblast differentiation, the cells were cultured in HG-DMEM supplemented with 4×10-5 g/L of dexamethasone, 0.05 g/L of ascorbic acid, 4.32 g/L of β-glycerophosphate, 3% (v/v) of FBS, and 1% (v/v) of penicillin and gentamicin. The BMSCs were cultured in osteogenic medium for 21 days and then stained with von Kossa dye to detect the deposition of mineralized nodules.
A 100-µl suspension of BMSCs with a density of 1×106 cells/ml was added to tubes for flow cytometry analysis (FACSCalibur; BD Biosciences, Franklin Lakes, NJ, USA). A total of 2 µl of anti-rat CD29-FITC (cluster of differentiation 29-fluorescein isothiocyanate), 4.5 µl of anti-rat CD106-PE (CD106- phycoerythrin), 0.5 µl of anti-rat CD44H-FITC, and 0.5 µl of anti-rat CD90/mouse CD90.1-FITC (Biolegend, San Diego, CA, USA) were each added to the tubes. After incubating the mixture with the antibodies for 20 minutes at room temperature and storing away from light, the mixtures were rinsed with 1 ml PBS in the presence of 1% BSA and resuspended into 500 µl PBS to determine the cell surface antigens. The results were analyzed by using CellQuest software (BD Biosciences) and the unlabeled rat BMSCs were used as the negative control.
A total of 15 SD rats with a mean weight of 150 g were enrolled in this study. The rats were intraperitoneally anesthetized with 3% (m/v) pentobarbital sodium. The back hairs of the rats were clipped. Then, the rats were placed in a prone position on the operation table and their extremities were tied. The back of the animals was scalded for 20 seconds by using a beaker containing half a cup of boiling water. Two scald wounds were made on the backs of the rats, one on each side. After scalding, each rat was treated with an intraperitoneal injection of 2 ml of physiological saline.
A total of 30 scald wounds on the rats' backs were randomly divided into 3 groups with 10 scald wounds each: (1) experimental treatment group; (2) experimental control group; and (3) blank control group.
The rats were subjected to escharotomy on the fourth day after scalding, and different treatments were conducted for the 3 groups. In the experimental treatment group, the scald wounds were covered with the mixture of fibrin glue and BMSCs by using a 'Y'-type syringe. The gel that formed within 2 minutes contained approximately 5×107 transplanted cells. The wounds of the experimental control group were injected only with fibrin glue. No intervention was administered to the blank control group. After transplantation, all wounds were bandaged for 3 days and then the bandages were removed. Observation and measurement of the diameters of the scald wounds were performed 30 days after treatment. The scald local tissues of all rats from the 3 groups were cut into pathological sections, stained with hematoxylin and eosin, and observed under the microscope (Olympus Corporation, Tokyo, Japan).
The experimental data were reported as mean±standard deviation; the differences of the diameters of the scald wounds in the 3 groups were analyzed statistically by using the t-test. All statistical analyses were performed using IBM SPSS Statistics 20.0 (IBM Co., Armonk, NY, USA) and p-values of <0.05 were considered significant.
On the first day of culture, the attached cells were few in number and distributed as short spindle-like cells. On the next day, many microcolonies appeared and the cells became elongated. The colonies multiplied quickly and gradually converged together. The cells showed a uniform, long spindle shape, and they were arranged spirally. On the fifth day, a cell monolayer was observed. The subcultured cells were initially spherical, and quickly attached to the wall of the plates within several hours and assumed a spindle shape again. After 3 days of cell transfer, a cell monolayer was observed. No significant changes were observed after 5 serial passages; however, increasing the number of passages would lead to diverse cell forms and aging cells.
The sixth-generation BMSCs were found to be normal diploid cells (1.00), with 86.99% of the cells in the G0/G1 phase. This showed that the cells had good proliferation activity (Fig. 1A).
After 21 days of osteogenic induction, the cells were positively stained with the von Kossa dye. Deposition of many brown focal mineralized nodules was observed. BMSCs that were chondrogenically induced for 28 days stained positive with toluidine blue dye, whereas the control groups showed negative staining. These results suggest that the BMSCs were pluripotent (Fig. 1B).
The expression of CD29, CD44H, CD90, and CD106 as surface markers of BMSCs was detected by using flow cytometry. All markers were positive, with the rate of positive expression being 99.58%, 93.30%, 82.50%, and 45.43% for CD29, CD44H, CD90, and CD106, respectively. The results were compatible with the characteristics of mesenchymal stem cells.
The scalded skin area was pale, and the skin became raised 10 minutes after scalding. On the first day after scalding, the skin gradually became red and some exudation appeared. On the fourth day after scalding, an eschar appeared on the scalded area, as well as yellow exudation around the scald. Physical activity of the rats significantly reduced (Fig. 2).
The pathological sections of the eschar showed that the epithelial cells had nuclear pyknosis. The collagen and elastic fibers in the dermal layer had been destroyed. A few residual hair follicles were visible, and the sebaceous glands showed structural failure. These histopathological results were compatible with skin pathological changes in deep second-degree burns12, suggesting that the method of making the rat scald model was feasible.
On the third day after transplantation, the wound dressings were removed. No substantial wound contraction was observed in all 3 groups. The mean diameter of the wounds was approximately 1.42 cm, and the wounds appeared bright red. On the seventh day after transplantation, the mean diameter of the dry and dark red wounds considerably reduced to approximately 0.79 cm in the experimental treatment group. However, the mean diameter of the wounds in the experimental control group and the blank control group was approximately 1.07 cm and 1.12 cm, respectively. The wounds of the experimental control group appeared dry and dark red, and a gray exudate remained on the wounds of the blank control group. On the 12th day after the transplantation, the mean diameter of the wounds was 0.25 cm in the experimental treatment group, and approximately 0.59 cm and 0.67 cm for the experimental control group and the blank control group, respectively. On the 14th day after the transplantation, some wounds in the experimental treatment group had healed, whereas the other 2 groups did not show any wound healing. On the 21st day after the transplantation, all the wounds of the experimental treatment group showed healing except for 1. The other 2 groups did not show healing of all the wounds until 30 days later (Fig. 3).
The histopathological sections showed that the newly formed epidermis with a normal structure was thicker than the normal epidermis in all groups. The newly formed dermal layer showed only collagen fibers consisting of fibroblasts. We found that the sebaceous glands showed obviously proliferous at the edge of the new tissue and gradually extended to the deep dermal layer of the new tissue in the experimental treatment group. The epidermal layer recessed and formed a hair follicle-like structure in the experimental treatment group but not in the other 2 groups (Fig. 4).
Conventional dressings can only be used as a temporary adjuvant therapy for skin burns but not for the treatment of large-area deep burns. The development of skin tissue engineering could offer patients a better quality of tissue repair. Ideally, patients would prefer tissue-engineered skin that not only can cover the wound immediately but also has the function of normal skin tissue.
The skin is mainly composed of the epidermis and dermis, and each layer consists of a variety of cells. Therefore, 1 of the most important aspects of tissue engineering is to choose a multipotent cell as the seed cell that can develop into all cell types of the skin. In this study, we selected BMSCs as seed cells because they could differentiate into various cells and tissues7,13. Many studies have found that BMSCs can differentiate into cells of the skin appendages14,15, such as sweat gland tissue16, at the wound site. BMSCs can also be induced to express the endothelial cell phenotype under suitable conditions17,18,19. Our experimental results also confirmed that these cells have multiple differentiation potentials. BMSCs have low immunogenicity. They can secrete certain cytokines to activate CD4+/CD25+ regulatory T-cells, inducing immune tolerance20,21,22. Therefore, in our experiments, we used allogeneic cells for transplantation to solve the problem of insufficient cells.
Another important aspect is the choice of scaffolds for the tissue-engineered skin. Fibrin glue is extracted from human plasma. The biological product is mainly composed of fibrinogen and thrombin preparations. It imitates the final stage of blood coagulation, that is, with the action of thrombin, Ca2+, and clotting factor XIII, fibrinogen rapidly solidifies and forms fibrin glue as a high-porosity structure consisting of a 3-dimensional network. The pore structure and high porosity of fibrin glue make it difficult to wash away by body fluids, and not easily degradable. The structure is also beneficial because it has a variety of growth factors and cells to adhere to23. Fibrin glue also has the characteristic of high plasticity24. It can be made into any shape for use in complex clinical cases, especially for the repair of uneven wounds. Furthermore, the mechanical properties of fibrin glue are superior to those of other gel-like scaffolds. In 2006, Liu et al.25 first reported in 'Science' that fibrin glue is 1 of the known natural fibers with the highest ductility and elasticity. Because fibrin glue has good cell and tissue compatibility, biodegradability, and no rejection and toxicity, it is a good candidate for tissue engineering of scaffolds.
In this study, we mixed fibrin glue with allogeneic BMSCs to produce an active dressing that can be used to coat burn wounds. The experimental results showed that the active dressing quickly formed a film-like gel on the wound. This method can cover wounds immediately, and thus provides a very good choice for patients with burns who need emergency skin substitutes.
From the transplantation therapy for the scalded rats, we found that the composite could promote healing of the scald wounds. There has been no consensus about the exact mechanism of action of MSCs in wound healing. One hypothesis involves the differentiation of MSCs into neo-tissues. Another hypothesis is that MSCs exert paracrine effects on the wound. Many researchers have suggested that the paracrine process may also be involved in tissue repair26. Our previous experiments showed that the transplanted cells are present in the neo-tissue27. Many studies have also demonstrated that BMSCs have the capacity to differentiate into certain cells in the neo-tissue28,29. This suggests that the transdifferentiation of BMSCs is involved in tissue repair.
Histological examination showed that the skin tissue of rats has a strong self-repair capability. In the case of full-thickness skin defects, it can repair itself to form new skin. The regenerated skin has a complete epidermal structure, although its dermal structure is incomplete. Owing to the lack of elastic fibers, the newly formed skin lacks elasticity and has poor mechanical properties compared with normal skin.
Importantly, the sebaceous glands showed obviously proliferous at the edge of the new tissue in the experimental treatment group. Furthermore, there was a hair follicle-like structure in the epidermal layer. The results suggest that BMSCs can promote skin appendage regeneration, which makes it possible to achieve a compound skin with complete physiological function.
In the comprehensive analysis of the experimental results, we found that the composite of fibrin glue and BMSCs could induce the formation of a complete skin structure and accelerate the healing rate of burned skin. The active dressing film made with fibrin glue and BMSCs is a good choice as a skin substitute for the treatment of patients with burns in the emergency setting.
Figures and Tables
Fig. 1
(A) Cell cycle analysis: 86.99% of the cells were in the G0/G1 phase, 6.76% were in the synthesis phase (S phase), and 6.25% were in the G2/M phase. (B) In vitro differentiation assay, von Kossa staining, and toluidine blue staining of rat bone marrow mesenchymal stem cells (BMSCs). (a) The negative controls (uninduced BMSCs) did not stain positive for von Kossa dye (×100). (b) After 21 days of osteogenic induction, the cells showed positive von Kossa staining (×100). (c) The negative control BMSCs were negative for toluidine blue staining (×100). (d) After the BMSCs were chondrogenically induced for 28 days, they showed positive toluidine blue staining (×40).

Fig. 2
Skin changes of the scald skin area at different times. (A) Ten minutes after scalding, (B) 1 day after scalding, and (C) 4 days after scalding.
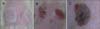
Fig. 3
Changes in wound diameter at different times after transplantation. *Compared with the experimental treatment group, p<0.01.

Fig. 4
Hematoxylin and eosin staining of the newly formed tissue in the 3 groups of rats 30 days after transplantation. The epidermal layer of each figure was marked with red arrow. (A) Normal skin: The epidermal layer (red arrows) was significantly thinner than in the other groups. There are abundant collagen and elastic fibers in the dermal layer, and they are disorderly arranged. Many skin appendages, such as sebaceous glands, hair follicles, and sweat glands, are also present (×100). (B) Blank control group. There are no elastic fiber and skin appendages in the dermal layer (×100). (C) Experimental control group (×100). (D) Experimental treatment group. Sebaceous glands show obviously proliferous at the edge of the new tissue, and gradually extend to the deep dermal layer. The epidermal layer recessed and formed a hair follicle-like structure (black arrows) (×100).

ACKNOWLEDGMENT
We thank Yunping Miao for her expert help with histology and Weifeng Ma for his care of the animals used in this study.
This study was supported by the China Natural Science Foundation (81071467), Zhejiang Natural Sciences Foundation (Y2090404), Zhejiang Medicine and Health Scientific Research Foundation (2011KYA001), Zhejiang Medical Key Subject Group Project (XKQ-010-001) Biological Medicine Key Discipline Group, and Zhejiang Provincial Science and Technology Plan Project of China (2013F1-0006).
References
1. Sheridan R. Closure of the excised burn wound: autografts, semipermanent skin substitutes, and permanent skin substitutes. Clin Plast Surg. 2009; 36:643–651.

2. Xia ZF. Development and status quo of the fermanent skin substitutes. Med J Chin PLA. 2003; 28:389–391.
3. Ren GH, Pei GX. Clinical application of tissue-engineered tissues. Chin J Tissue Eng Res. 2006; 10:152–156.
4. Middelkoop E, van den Bogaerdt AJ, Lamme EN, Hoekstra MJ, Brandsma K, Ulrich MM. Porcine wound models for skin substitution and burn treatment. Biomaterials. 2004; 25:1559–1567.

5. Liu P, Deng Z, Han S, Liu T, Wen N, Lu W, et al. Tissue-engineered skin containing mesenchymal stem cells improves burn wounds. Artif Organs. 2008; 32:925–931.

6. Huang S, Lu G, Wu Y, Jirigala E, Xu Y, Ma K, et al. Mesenchymal stem cells delivered in a microsphere-based engineered skin contribute to cutaneous wound healing and sweat gland repair. J Dermatol Sci. 2012; 66:29–36.

7. Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999; 284:143–147.

8. Zhu L, Li Q, Lin L, Wu H, Zhu S, Yu L. Effects of simulated microgravity on repairing articular cartilage defects by chondrocyte-modified fibrin glue bracket in rabbits. Chin J Bone Jt Inj. 2008; 23:741–744.
9. Tokuishi K, Yamamoto S, Anami K, Moroga T, Miyawaki M, Chujo M, et al. Successful application of subcutaneous adipose tissue with fibrin glue in conservative treatment of tracheobronchial rupture. Ann Thorac Surg. 2012; 94:1726–1729.

10. Dhua AK, Ratan SK, Aggarwal SK. Chylothorax after primary repair of esophageal atresia with tracheo-esophageal fistula: successful management by biological fibrin glue. APSP J Case Rep. 2012; 3:16.
11. Miri Bonjar MR, Maghsoudi H, Samnia R, Saleh P, Parsafar F. Efficacy of fibrin glue on seroma formation after breast surgery. Int J Breast Cancer. 2012; 2012:643132.

12. Feng S, Hua L, Jin S, Yan Z, Zhao Y, Zhu Q. Making the rat scald model. Acta Universitatis Medicinalis Secondae Shanghai. 1996; 15:195–197.
13. Jiang Y, Jahagirdar BN, Reinhardt RL, Schwartz RE, Keene CD, Ortiz-Gonzalez XR, et al. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature. 2002; 418:41–49.

14. Li H, Fu X, Wang J. Primary experimental studies on differentiation of marrow mesenchymal stem cells into skin appendage cells in vivo. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2006; 20:675–678.
15. Li H, Fu X, Ouyang Y, Cai C, Wang J, Sun T. Adult bone-marrow-derived mesenchymal stem cells contribute to wound healing of skin appendages. Cell Tissue Res. 2006; 326:725–736.

16. Fu X, Sun T, Lei Y, Bao X, Zhang C, Cheng Z. Distribution of nerve and blood vessels in regenerative sweat glands induced from bone marrow mesenchymal stem cells. J Trauma Surg. 2009; 11:388–392.
17. Yang ZM, Fan ZF, Xie HQ, Qin TW, Peng WZ. Vascularization and its relationship to osteogenesis in transplantation of tissue engineered bone to repair segment defect of long bone. Chin J Microsurg. 2002; 25:119–122.
18. Fang LJ, Fu XB, Sun TZ, Li JF, Cheng B, Yang YH, et al. An experimental study on the differentiation of bone marrow mesenchymal stem cells into vascular endothelial cells. Zhonghua Shao Shang Za Zhi. 2003; 19:22–24.
19. Schatteman GC, Hanlon HD, Jiao C, Dodds SG, Christy BA. Blood-derived angioblasts accelerate blood-flow restoration in diabetic mice. J Clin Invest. 2000; 106:571–578.

20. Le Blanc K, Rasmusson I, Sundberg B, Götherström C, Hassan M, Uzunel M, et al. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet. 2004; 363:1439–1441.

21. Fibbe WE, Noort WA. Mesenchymal stem cells and hematopoietic stem cell transplantation. Ann N Y Acad Sci. 2003; 996:235–244.

22. Chao YH, Wu HP, Chan CK, Tsai C, Peng CT, Wu KH. Umbilical cord-derived mesenchymal stem cells for hematopoietic stem cell transplantation. J Biomed Biotechnol. 2012; 2012:759503.

23. Mosesson MW. Fibrinogen and fibrin structure and functions. J Thromb Haemost. 2005; 3:1894–1904.

24. Collet JP, Shuman H, Ledger RE, Lee S, Weisel JW. The elasticity of an individual fibrin fiber in a clot. Proc Natl Acad Sci U S A. 2005; 102:9133–9137.

25. Liu W, Jawerth LM, Sparks EA, Falvo MR, Hantgan RR, Superfine R, et al. Fibrin fibers have extraordinary extensibility and elasticity. Science. 2006; 313:634.

26. Cheng K, Rai P, Plagov A, Lan X, Kumar D, Salhan D, et al. Transplantation of bone marrow-derived MSCs improves cisplatinum-induced renal injury through paracrine mechanisms. Exp Mol Pathol. 2013; 94:466–473.

27. Yang YD, Zhang WY, Fang GJ, Wo EK, He ZJ, Hong Y, et al. Cell sources for cartilage defect repair with rabbit bone marrow mesenchymal stem cells PCR amplification for sex-determining gene sequence. J Clin Rehabil Tissue Eng Res. 2007; 11:7341–7344.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download