Dear Editor:
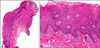
Infantile perianal pyramidal protrusion (IPPP) is a rare benign cutaneous disorder, first reported by Kayashima et al. in 19961. It is characterized by a solitary protrusion, most often observed in the perineal area, anterior to the anus. Herein, we report a case of acquired IPPP in a female Korean patient; to the best of our knowledge, this is only the second such case reported in Korean dermatologic literature2. A 2-year-old girl visited our clinic, presenting with an anal lesion that was discovered 5 months previously. She had no medicosurgical history, but experienced intermittent constipation that was untreated. The patient had no history of sexual abuse. Skin exam revealed a solitary skin-colored papule, located anterior to the anus (Fig. 1). A skin biosy of the papule indicated epidermal acanthosis, and dermal fibrovascular cores with lymphocytic infiltration (Fig. 2). Vacuolar changes and dermal edema were not observed. Correlation of the clinical and histologic findings resulted in a final diagnosis of acquired IPPP. Excluding this recent case, approximately 107 IPPP cases have been reported in the literature1. All patients with IPPP, except one, were women, including our patient. Age at diagnosis ranged from birth, to 13 years. Three types of IPPP were recently proposed: constitutional IPPP, acquired IPPP, and IPPP caused by lichen sclerosus et atrophicus (LSA). Constitutional IPPP that could have familial or congenital origin, is the most common type, and is thought to be associated with structural weakness of the perineum in women. It regresses within a few weeks, although some cases have reportedly been prolonged for years. Constipation is known to be indicative of acquired IPPP, although the pathogenesis of this disorder is not yet completely understood. Regression of IPPP was reportedly observed, after constipation was controlled1. LSA associated IPPP involves a skin protrusion clinically similar to those observed in other types of IPPP, but is histopathologically different in the exhibition of dermal vacuolar changes, along with dermal edema, and a lichenoid lesion, characterized by infiltration of inflammatory cells. Although our patient did not exhibit pathologic findings typical of LSA associated IPPP, she presented with constipation, which indicated acquired IPPP. Despite being proposed as a subtype of IPPP, the pathophysiology of acquired IPPP is unclear. Histologic findings of IPPP, except in patients with LSA associated IPPP, indicate epidermal acanthosis and dilated vessels with fibrous tissue, although normal histology has also been reportedly observed1. Condyloma should be differentiated from IPPP, by epithelial cells with perinuclear vacuolization, and the presence of human papilloma virus3. Hemorrhoids, which also occur in the anal area, are vascular cushions within the anal canal. The disease is different, in that the onset of hemorrhoidal disease is commonly between 45 to 65 years of age, accompanied by symptoms such as painless bleeding, painful mass, anal swelling, or soiling4. Histologically, hemorrhoids exhibit superficial ulcerations, overlying mucosa with acute and chronic inflammations. Thrombosed vessels could be detected5. Various treatment modalities are available for IPPP, such as management and control of bowel movement, application of topical corticosteroids, or observation based on the type and suspected underlying conditions. IPPP is clinically important, because the papule at the perineum in children may confuse physicians, and result in a misdiagnosis of condyloma or sexual abuse. Although we now present this case as the 'second' report, we also consider this disease to be quite common in Korean infants. Our case is worthy and informative, however, in that we observed not only typical clinical features, but also showed histologic features of IPPP by skin biopsy, which is not routinely done. Herein, we report a case of IPPP, and physicians are recommended to consider this disease during diagnosis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download