Abstract
Congenital self-healing reticulohistiocytosis (CSHRH) is a rare, cutaneous, self-limited form of Langerhans cell histiocytosis. Whereas multiple lesions are common, a solitary lesion is rare. A 14-day-old neonate presented with a solitary, 5-mm, oval, reddish, and eroded papule with crust on the left thigh that had existed since birth. No systemic involvement was found. Histopathology revealed dense infiltration of large histiocytes with scattered eosinophils and lymphocytes in the dermis. Immunohistochemistry showed S-100 and CD1a positivity. Two months later, the skin lesion involuted spontaneously, without evidence of recurrence and extracutaneous involvement. On the basis of the characteristic clinical course and typical histopathological findings, a diagnosis of solitary CSHRH was made.
Congenital self-healing reticulohistiocytosis (CSHRH), first described in 1973 by Hashimoto and Pritzker1, is a rare Langerhans cell disorder that typically presents at birth or in the neonatal period, and involutes spontaneously within weeks to a few months without the involvement of any other organs2.
Although CSHRH commonly presents as multiple cutaneous papulonodules, there have been a few reports of solitary lesions in the dermatological literature since Berger et al.3 first reported on a solitary variant of CSHRH4,5,6,7,8,9,10. Only three such cases have been reported in the Korean dermatological literature4,5. Herein, we report on an additional rare case of solitary CSHRH in a 14-day-old female neonate.
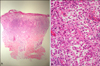
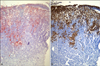
A 14-day-old female neonate was brought to our department by her mother because of a skin lesion on the left thigh that had been present since birth. She was delivered vaginally at full term, as the first child, after an uncomplicated pregnancy. Her birth weight, length, and Apgar score were within the reference ranges. She presented with a solitary, 5-mm, oval, firm, reddish, and eroded papule with crust on her left anterior thigh (Fig. 1A). The physical examination was otherwise normal, without signs of hepatosplenomegaly or lymphadenopathy. Laboratory tests, including complete blood count, urinalysis, blood glucose level, liver and kidney function, chemistry profile, chest radiograph, and newborn screening tests, were unremarkable. On hematoxylin and eosin-stained section of a skin biopsy from the lesion, focal erosion and crusting of the epidermis were observed, and the dermoepidermal junction was indistinct. Within the dermis, there was a dense dermal infiltrate of large and round histiocytic cells with abundant eosinophilic cytoplasm. The nuclei were of various shapes and sizes, from irregularly round to oval or kidney-shaped without atypia. Scattered lymphocytes, eosinophils, and neutrophils were also seen (Fig. 2). Most histiocytic cells showed positive staining for S-100 and CD1a, indicating that these were Langerhans cells (Fig. 3). Electron microscopy was not performed. Two months later, the skin lesion resolved spontaneously with a hypertrophic scar (Fig. 1B). Recurrence and systemic involvement were not observed during a follow-up period of 6 months. A diagnosis of solitary CSHRH was made on the basis of the clinical and histopathological findings.
Langerhans cell histiocytosis (LCH) is characterized by monoclonal proliferation of Langerhans cells, and the diagnosis is based on the histological criteria established by the International Histiocyte Society in 19876. The clinical variants of LCH consist of Letterer-Siwe disease, Hand-Schuller-Christian disease, eosinophilic granuloma, and CSHRH6. LCH mainly affects children and is commonly recognized as a sporadic disorder. Genetic factors and viral infections are considered to be likely pathogenic factors7.
CSHRH is rare, and the incidence reported in the literature varies substantially. This disease has probably been underdiagnosed because the lesions regress spontaneously8,9. It is characterized by congenital or neonatal isolated cutaneous involvement, sparing the mucosae, and with no extracutaneous involvement7,8,9,10. The lesions can be multiple or, rarely, solitary1,2,3,4,5,6,7,8,9,10,11. Solitary CSHRH seems to represent about 25% of the patients among all cases of CSHRH7,8. This form usually presents with a single cutaneous red-brown nodule that is firm and painless, and the nodule tends to progress to crusting or ulceration7,8. It can develop in any anatomical site of the body, and its mean size ranges from 5 to 20 mm7,8. Only three cases of solitary CSHRH have been reported in the Korean dermatological literature (Table 1)4,5,12. In our case, the cutaneous lesion had been present since birth, with no predilection areas. The clinical appearance of all four Korean cases involved a papule with crust. Systemic involvement was not detected from the laboratory results, and the lesions spontaneously regressed. Clinically, the Korean cases of are not much different from the Western cases.
The histopathological findings of solitary CSHRH are the same as multiple papulonodular forms. The findings reveal a dense dermal infiltrate composed predominantly of large histiocytes with abundant eosinophilic cytoplasm and round to oval or kidney-shaped nucleus8,9. These are accompanied by a mixed infiltrate with variable numbers of eosinophils and lymphocytes8,9. The diagnosis is confirmed by a positive immunohistochemical staining for CD1a and S-100, markers of Langerhans cells8,11. Electron microscopy examination shows Birbeck granules and laminated dense bodies in the histiocytes; however, it is usually unnecessary and not routinely performed8,11,13.
Differential diagnosis includes juvenile xanthogranuloma, hemangioma, congenital Spitz nevus, congenital fibrosarcoma, infantile fibrous hamartoma, infantile myofibroma, and, although not a solitary lesion, benign cephalic histiocytosis could also be considered. In most cases, routine histology and immunohistochemistry, such as S-100 and CD1a staining, aids in excluding those diseases8,9,10.
No treatment is recommended, and the prognosis is excellent, with the lesions regressing spontaneously within a few weeks or months8,9,10. In the case of solitary CSHRH, associated visceral anomalies have never been found initially or during follow-up, unlike the classic form of CSHRH, for which hematological, hepatic, bone, and lung anomalies have been reported3,4,5,7,8,9,10. Recurrence and late complication have also never been reported for solitary lesions3,4,5,7,8,9,10,12. No guidelines for the follow-up of CSHRH have been established. Concerning solitary CSHRH, Zunino-Goutorbe et al.8 recommended regular physical examination for at least 2 years initially, supplemented by simple laboratory tests and radiographs, with repetition of laboratory analyses perhaps exclusively at 6 months and imaging studies only if required by clinical manifestations. Our patient's lesion resolved after 2 months without any intervention, and there was no evidence of extracutaneous involvement, complication, and recurrence. Our case report is significant because it provides photographic documentation of the self-regressing nature of solitary CSHRH.
In summary, because of its self-healing nature, solitary CSHRH has probably been underestimated, and physicians may have missed the diagnosis in the past. This rare solitary CSHRH should be included in the differential diagnosis of congenital solitary cutaneous nodules, and histopathological examination is essential to differentiate between the numerous disorders.
Figures and Tables
Fig. 1
Clinical photographs of congenital self-healing reticulohistiocytosis. (A) A solitary, 5-mm, oval, firm, reddish, and eroded papule with crust on the left anterior thigh at initial presentation. (B) After 2 months, the lesion clinically resolved with hypertrophic scar.

Fig. 2
Histopathological findings of the lesion. (A) Focal erosion and crusting of the epidermis, indistinct dermoepidermal junction, and a dense dermal infiltrate in the upper-and mid-dermis are seen. (B) A dense dermal infiltrate consists of large and round histiocytic cells with various nuclei in shapes and sizes, from irregularly round to oval or kidney-shaped without atypia (A: H&E, ×40; B: H&E, ×400).
References
1. Hashimoto K, Pritzker MS. Electron microscopic study of reticulohistiocytoma. An unusual case of congenital, self-healing reticulohistiocytosis. Arch Dermatol. 1973; 107:263–270.

2. Shin N, Kang MJ, Cho S, Whang KK, Hahm JH. A case of congenital self-healing reticulohistiocytosis. Ann Dermatol. 2000; 12:193–196.

3. Berger TG, Lane AT, Headington JT, Hartmann K, Burrish G, Levin MW, et al. A solitary variant of congenital self-healing reticulohistiocytosis: solitary Hashimoto-Pritzker disease. Pediatr Dermatol. 1986; 3:230–236.

4. Chun SI, Song MS. Congenital self-healing reticulohistiocytosis--report of a case of the solitary type and review of the literature. Yonsei Med J. 1992; 33:194–198.

5. Shin MS, Park HJ, Choi YJ, Park MY. A case of a solitary type of congenital self-healing reticulohistiocytosis. Korean J Dermatol. 2008; 46:411–413.
6. Writing Group of the Histiocyte Society. Histiocytosis syndromes in children. Lancet. 1987; 329:208–209.
7. Ersoy-Evans S, Gursoy T, Yigit S, Akcoren Z, Sahin S. Solitary congenital self-healing reticulohistiocytosis in monozygotic twins. Pediatr Dermatol. 2006; 23:273–275.

8. Zunino-Goutorbe C, Eschard C, Durlach A, Bernard P. Congenital solitary histiocytoma: a variant of Hashimoto-Pritzker histiocytosis. A retrospective study of 8 cases. Dermatology. 2008; 216:118–124.

9. Bernstein EF, Resnik KS, Loose JH, Halcin C, Kauh YC. Solitary congenital self-healing reticulohistiocytosis. Br J Dermatol. 1993; 129:449–454.

10. Masouyé I, Chavaz P, Salomon D, Balderer J, Carraux P, Saurat JH. Solitary Langerhans cell histiocytoma: an unusual form of Hashimoto-Pritzker histiocytosis? Pediatr Dermatol. 1990; 7:299–302.

11. Jensen ML, Bygum A, Clemmensen O, Fenger-Gron J. Congenital self-healing reticulohistiocytosis - an important diagnostic challenge. Acta Paediatr. 2011; 100:784–786.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download