Abstract
Bowen's disease is a squamous cell carcinoma in situ and has the potential to progress to a squamous cell carcinoma. The authors treated two female patients (a 39-year-old and a 41-year-old) with Bowen's disease in the vulva area using topical photodynamic therapy (PDT), involving the use of 5-aminolaevulinic acid and a light-emitting diode device. The light was administered at an intensity of 80 mW/cm2 for a dose of 120 J/cm2 biweekly for 6 cycles. The 39-year-old patient showed excellent clinical improvement, but the other patient achieved only a partial response. Even though one patient underwent a total excision 1 year later due to recurrence, both patients were satisfied with the cosmetic outcomes of this therapy and the partial improvement over time. The common side effect of PDT was a stinging sensation. PDT provides a relatively effective and useful alternative treatment for Bowen's disease in the vulva area.
Bowen's disease usually manifests as a solitary slowly enlarging erythematous patch with an irregular margin on any part of the body. A number of different modalities are available for the treatment of Bowen's disease1, which can be categorized as: surgical and destructive therapies, topical therapies, and non-surgical ablative therapies2. Photodynamic therapy (PDT) is being increasingly used to treat superficial skin cancers; it is a non-destructive, painless treatment which achieves good cosmetic outcomes. It has also been shown to be an effective treatment for various cutaneous and non-cutaneous malignancies. This treatment modality is based on the generation of highly reactive oxygen intermediates due to the interaction between the light and a photosensiziter. Despite its feasibility and increasing popularity, PDT has not been studied much so far; only a few reports have been issued on its use to treat Bowen's disease in the vulva region. Here, we describe two cases of Bowen's disease arising in this region and which were treated with topical PDT using 5-aminolaevulinic acid (5-ALA) and a light-emitting diode device.
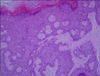
A 39-year-old woman presented with a 3-year history of mild bleeding after a minor trauma and ulcerative lesions located on the left labium minor. The lesions had slowly enlarged over time and occasionally bled and were continuously macerated and painful. The patient had no family history of skin cancer and was otherwise in good health. A physical examination of the lesions revealed erosive patches and verrucous papules with a pinkish center and a black-pigmented margin on the left labium minor (Fig. 1A). A complete blood count, liver function tests, and urine analysis findings were all within the normal limits or shown negative. A 4-mm punch biopsy was conducted on the left labium minor, and a diagnosis of Bowen's disease was established based on the clinical and histopathological findings (Fig. 2). The patient was not in favor of surgical lesion removal, and thus, we chose to use PDT. After washing the affected region with a 0.9% saline solution, a topical 5-ALA cream was applied to the cutaneous and the mucosal lesions as well as the clinically disease-free margin of 1 to 2 cm around the lesions. The affected area was then covered with transparent adhesive film (Tegaderm™; 3M, Bracknell, UK) and a light-opaque dressing to ensure photoprotection. Five hours later, the residual cream was gently removed using a 0.9% saline solution. To reduce discomfort, the patient was pre-medicated with non-steroidal anti-inflammatory drugs (NSAIDs). The lesions were irradiated with 120 J/cm2 of 633±3 nm red light from a light-emitting diode device, at a light intensity of 80 mW/cm2. All the lesions were treated over the course of six sessions, 14 days apart. The treatment resulted in an obvious lesion regression (Fig. 1B) and no significant side effect was encountered during the treatment or scarring after the treatment. An excellent clinical improvement was observed after the PDT, and lesions did not recur over the course of 18 months follow-up.
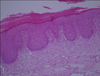
A 41-year-old woman presented with erosive macerative patches and verrucous papules on both major labia. The lesions had been initially noticed 1 year ago and slowly developed since them. The patient complained of a slight itchiness a moderate pain. She had no significant medical history or a family history of particular medical conditions. An examination revealed round, erosive patches, and verrucous papules on both major labia (Fig. 3). Based on the clinical and histopathological features, Bowen's disease was diagnosed (Fig. 4). 5-ALA emulsion (20%) was applied under an occlusive dressing; 5 hours later, the lesions were irradiated with 120 J/cm2 from a lightemitting diode (red light of wavelength 633±3 nm) and at an intensity of 80 mW/cm2. The patient experienced a slight stinging sensation during the treatment, but analgesics were sufficient to ameliorate the symptom. After 4 cycles of PDT, the skin lesions were much reduced. Subsequently, the patient was lost to follow up, and 1 year later underwent a total excision for a recurrence.
Bowen's disease is an intraepidermal squamous cell carcinoma (carcinoma in situ) as originally described by John T. Bowen1. This disease has the potential to progress to an invasive carcinoma and may affect both the skin and the mucous membrane of the glans penis, vulva, and oral mucosa. Bowen's disease may occur at any age, but patients older than 60 years are typical, and it can occur anywhere in the body1. Lesions are slow growing, well-defined, erythematous plaques with irregular borders and a scaly or a crusted surface.
A variety of different modalities can be used to treat Bowen's disease, which can be categorized as: surgical and destructive therapies, topical therapies, and non-surgical ablative therapies2. Excision, cryotherapy, and curettage with or without cautery fall under the category of the surgical and the destructive therapy. Topical therapies involve the use of 5-fluorouracil (5-FU) or 5% imiquimod. Radiotherapy, laser ablation therapy, and PDT constitute non-surgical ablative therapies2.
The treatment decision making should taken into account multiple factors including the location, the size, and the number of the lesion, the clinician's expertise, the patient's age and the immune status, cosmetic outcome, and the patient's preference.
Bowen's disease in the vulva area is difficult to treat using cryotherapy due to its painful nature and some patients simply do not favor aggressive treatment for cosmetic reasons. On the other hand, PDT is painless and produces good cosmetic outcomes2. However, despite the many reports of successful PDT treatment (Table 1)3,4,5,6,7,8,9,10,11,12,13,14,15,16, only a few have described the treatment of genital lesions.
PDT is a well-established therapeutic option for actinic keratosis, basal cell carcinoma, Bowen's disease, and superficial squamous cell carcinoma, and inflammatory dermatoses like acne vulgaris and localized scleroderma. The pathogenic mechanism responsible for the development of topical PDT has not been determined. On the other hand, PDT is known to trigger cell death directly via apoptosis and necrosis17.
Calin et al.18 found no significant differences between the efficacies of coherent (laser) and non-coherent (lamps and light-emitting diodes) light sources. All the light sources have a similar efficacy for treatment, and no distinguished side effect was found between the light sources. The difference between the side-effect of the light sources is the imperceptibility19. The most common side-effects reported for PDT are erythema and pain11,19. This pain or discomfort is often described as a burning or stinging sensation and was experienced by our patients during the exposure to the light source. However, it has been reported that the size of the lesion is the strongest predictor of pain, rather than the light source19. Even though this discomfort can persist for several hours, it responds to NSAIDs19. In our cases, the pain and the discomfort were not severe. Erythema and short-term swelling occurred, but no superficial erosions or oozing lesions were observed after the exposure, and the side effects subsided over the course of one week.
PDT is a non-invasive treatment and allows anatomically difficult areas to be successfully treated2. PDT has the advantage of causing only a little damage to the normal tissue and providing excellent cosmetic outcomes. What is more, its side effects, such as stinging or burning, are minimal11,19.
Methyl-ALA (MAL) has been shown to be more lesion-specific for premalignant and malignant lesions than 5-ALA19. In addition, it is more stable and penetrates deep into the tissues due to its greater lipophilicity. Good clinical and cosmetic results have been reported for MAL20. In the above cases, the use of PDT using 5-ALA to treat the vulva lesions proved to be effective and achieved good cosmetic results. One patient experienced a mild stinging sensation in the treated area, but this was short lived.
The use of topical PDT for the treatment of Bowen's disease on the vulva area appears to be a highly effective therapeutic option that produces good cosmetic results. Furthermore, it is a tissue-sparing treatment and non-invasive. Both of our patients were satisfied with their cosmetic results, although the skin lesions partially remained. Further studies are needed to develop the use of PDT to treat Bowen's disease in the vulva region.
Figures and Tables
 | Fig. 1(A) Erosive patches and verrucous papules with a pinkish center and a black-pigmented margin on the left labium minor. (B) After six sessions of photodynamic treatment. |
References
1. Strayer DS, Santa Cruz DJ. Carcinoma in situ of the skin: a review of histopathology. J Cutan Pathol. 1980; 7:244–259.

2. Duncan KO, Geisse JK, Leffell DJ. Epithelial precancerous lesions. In : Wolff K, Austen KF, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, editors. Fitzpatrick's dermatology in general medicine. 7th ed. New York: McGraw-Hill;2007. p. 1021–1023.
3. Svanberg K, Andersson T, Killander D, Wang I, Stenram U, Andersson-Engels S, et al. Photodynamic therapy of nonmelanoma malignant tumours of the skin using topical deltaamino levulinic acid sensitization and laser irradiation. Br J Dermatol. 1994; 130:743–751.

4. Fijan S, Hönigsmann H, Ortel B. Photodynamic therapy of epithelial skin tumours using delta-aminolaevulinic acid and desferrioxamine. Br J Dermatol. 1995; 133:282–288.

5. Morton CA, Whitehurst C, Moore JV, MacKie RM. Comparison of red and green light in the treatment of Bowen's disease by photodynamic therapy. Br J Dermatol. 2000; 143:767–772.

6. Morton CA, Whitehurst C, McColl JH, Moore JV, MacKie RM. Photodynamic therapy for large or multiple patches of Bowen disease and basal cell carcinoma. Arch Dermatol. 2001; 137:319–324.
7. Salim A, Leman JA, McColl JH, Chapman R, Morton CA. Randomized comparison of photodynamic therapy with topical 5-fluorouracil in Bowen's disease. Br J Dermatol. 2003; 148:539–543.

8. Britton JE, Goulden V, Stables G, Stringer M, Sheehan-Dare R. Investigation of the use of the pulsed dye laser in the treatment of Bowen's disease using 5-aminolaevulinic acid phototherapy. Br J Dermatol. 2005; 153:780–784.

9. Morton C, Horn M, Leman J, Tack B, Bedane C, Tjioe M, et al. Comparison of topical methyl aminolevulinate photodynamic therapy with cryotherapy or fluorouracil for treatment of squamous cell carcinoma in situ: results of a multicenter randomized trial. Arch Dermatol. 2006; 142:729–735.
10. de Haas ER, Sterenborg HJ, Neumann HA, Robinson DJ. Response of Bowen disease to ALA-PDT using a single and a 2-fold illumination scheme. Arch Dermatol. 2007; 143:264–265.

11. Kim YJ, Kang HY, Lee ES, Kim YC. Photodynamic therapy for treatment of Bowen's disease. Korean J Dermatol. 2007; 45:237–241.
12. de Haas ER, de Vijlder HC, Sterenborg HJ, Neumann HA, Robinson DJ. Fractionated aminolevulinic acid-photodynamic therapy provides additional evidence for the use of PDT for non-melanoma skin cancer. J Eur Acad Dermatol Venereol. 2008; 22:426–430.

13. Calzavara-Pinton PG, Venturini M, Sala R, Capezzera R, Parrinello G, Specchia C, et al. Methylaminolaevulinatebased photodynamic therapy of Bowen's disease and squamous cell carcinoma. Br J Dermatol. 2008; 159:137–144.

14. Doffoel-Hantz V, Sparsa A, Marin B, Durox H, Bonnetblanc JM, Bédane C. The value of photodynamic therapy in the treatment of Bowen's disease. Ann Dermatol Venereol. 2008; 135:822–827.
15. Truchuelo M, Fernández-Guarino M, Fleta B, Alcántara J, Jaén P. Effectiveness of photodynamic therapy in Bowen's disease: an observational and descriptive study in 51 lesions. J Eur Acad Dermatol Venereol. 2012; 26:868–874.

16. López N, Meyer-Gonzalez T, Herrera-Acosta E, Bosch R, Castillo R, Herrera E. Photodynamic therapy in the treatment of extensive Bowen's disease. J Dermatolog Treat. 2012; 23:428–430.

17. Oleinick NL, Morris RL, Belichenko I. The role of apoptosis in response to photodynamic therapy: what, where, why, and how. Photochem Photobiol Sci. 2002; 1:1–21.

18. Calin MA, Diaconeasa A, Savastru D, Tautan M. Photosensitizers and light sources for photodynamic therapy of the Bowen's disease. Arch Dermatol Res. 2011; 303:145–151.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download