Abstract
Angiosarcoma is a highly malignant vascular tumor of endothelial origin. Initially, a cutaneous manifestation presents as a singular or multifocal bruise-like patches on the skin, most frequently on the face, the scalp or the neck regions. On progression, the lesions become violaceous, and ill-defined spongy nodular tumors appear. Our patient was a 71-year-old man with a previous history of angiosarcoma on the right forehead and was treated with an excision and local radiation 3 years ago. Several months after the treatment, a dark brownish to violaceous patch with edema arose from the right upper eyelid and spread out to the lower eyelid. Clinically, an ecchymosis caused by trauma or other hemangioma was suspected more than a recurrent angiosarcoma. Histopathologic examinations including immunohistochemical studies were consistent with cutaneous angiosarcoma. Herein, we report a rare case of a recurrent isolated angiosarcoma without the recurrence of a primary lesion.
The optimal treatment for a craniofacial angiosarcoma is a surgical resection with a postoperative radiation; yet frequently, the disease is already extensive at the time of the diagnosis that it is not completely resectable1,2. The prognosis is grave with a recently reported 5-year local recurrence rate of 84% and the 5-year survival rate range from 12% to 34%3,4. Previously, our patient was treated for a primary angiosaroma of the right forehead with a surgical resection followed by a radiation therapy 3 years ago, and the tumor recurred on the right upper eyelid that was remote from the site of the previous surgery, not the right forehead where the primary angiosarcoma developed. Initially, ecchymosis caused by a trauma or other hemangioma was more suspected than a recurrent angiosarcoma because there was no sign of recurrence around the surgical scar. This case illustrates that a locally recurrent angiosarcoma can develop without a direct connection to the primary lesional recurrence. We report here a rare case of a recurrent isolated eyelid angiosarcoma remote from the primary angiosarcoma, showing ecchymosis-like clinical feature.
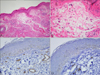
A 71-year-old Korean male was presented with a dark brownish to violaceous discoloration with edema on the right eyelid. He had been diagnosed with angiosarcoma on the right forehead 3 years ago and was treated with a complete excision of the lesion with a negative margin and an adjuvant radiotherapy (66 Gy in total) at another university hospital. Several months after the treatment, a dark brownish to violaceous patch with edema arose from his right upper eyelid and gradually spread out to the lower eyelid (Fig. 1A). Clinically, an ecchymosis caused by a trauma or other hemangioma was suspected more than a recurrent angiosarcoma, because the lesion was about 3 cm away from the surgical scar from the previous operation on the right forehead, and it presented as an edematous, purpuric patch such as the black eye. A skin biopsy taken from the upper eyelid showed numerous irregular anastomosing vascular channels lined by a single layer of somewhat enlarged atypical endothelial cells dissecting collagen bundles in the dermis (Fig. 2A, B). Immunohistochemically, the tumor cells showed a positive reaction for CD31 and D2-40 (Fig. 2C, D). A pathologic diagnosis of well differentiated angiosarcoma was made, and it was identical to that of primary angiosarcoma of the right forehead 3 years ago.
All routine laboratory tests, including a complete blood count, a urinalysis, the blood glucose level, the liver and the kidney function and the chemistry profile were within normal range. Positron emission tomography-computed tomography findings showed no evidence of distant metastasis. Because the tumor involved almost the entire right eyelid diffusely, a surgical excision was not an option. As the tumor gradually spread, he was referred to the radiooncology department for a radiotherapy. He underwent a radiation therapy with a total dose 66 Gy in 33 fractions over 2 months. After the 2 months' course of treatment, a moderate clinical improvement was shown (Fig. 1B). One and a half months later, we performed a skin biopsy to find out the histological improvement. But, the histopathologic findings revealed atypical scattered tumor cells in the dermis suggestive of the remnant of an angiosarcoma (Fig. 3A, B). An immunohistochemical staining was positive for the CD31 and negative for D2-40 (Fig. 3C, D). Thus, we concluded that he responded to the radiotherapy with a partial regression of the tumor. We could not perform the next sessions of radiotherapy because we believed that a periorbital edema and the induration might be worsened and he might not be able to open his eye. After a discussion with the multidisciplinary team, it was decided that he will be treated with a paclitaxel chemotherapy. Now, he is under a treatment with a weekly paclitaxel and we are following-up on the treatment response.
Angiosarcomas are rare malignant tumors arising from the vascular or the lymphatic endothelium and comprise 2% of all soft tissue sarcomas3. They can occur in a variety of sites, but 60% of the cases arise within the skin or the superficial soft tissues3. The majority of these tumors arise in the head and the neck area and, rarely had an isolated eyelid involvement been reported3,4,5,6. Interestingly, our patient was presented with an ecchymosis-like clinical feature on the unilateral periorbital area rather than a recurrent angiosaroma.
The pathogenesis of angiosarcoma remains unclear. It develops de novo in most cases although it has also been reported to arise after an irradiation of some vascular tumors or from a persistent chronic lymphedema in the extremities (Stewart-Treves syndrome)3,5.
Angiosarcoma typically appears as a slowly expanding erythematous plaque and a deceptively benign ecchymotic to bruise-like presentation may be observed. The clinical appearance of angiosarcoma can vary and the diagnosis is often delayed. The clinical differential diagnosis includes seborrheic dermatitis, ecchymoses, capillary haemangioma, cellulitis, erysipelas, rosacea, angioedema, melanoma and Kaposi's sarcoma. These are usually asymptomatic but may cause bleeding intermittently, become edematous, or cause pain. The skin lesions are usually red or blue, although they are occasionally tan or resemble a normal skin color3,4,5. Because they are often poorly defined, it is difficult to determine the the extent of the tumor.
Currently, there are no standard guidelines on the treatment of a cutaneous angiosarcoma. A wide surgical excision is the first choice of therapy in small angiosarcomas. This may be followed by an external beam radiotherapy in order to offer the best chance for a long-term control and survival. If a surgical excision is not possible in the case of a diffuse or multifocal tumor, radiotherapy is the choice for palliative therapy; yet, the role of chemotherapy remains undefined3,4,5,6,7,8. Several reports suggest that a paclitaxel may be effective in angiosarcomas of the head and the neck. Bevacizumab, a humanized monoclonal antibody to vascular endothelial growth factor (VEGF), with or without radiotherapy and chemotherapy, is another viable option; still, further studies are warranted2,9,10,11. VEGF is overexpressed in 80% of angiosarcomas2,10,11. Initially, our patient was treated with a radiation therapy because of the diffuse involvement of the eyelid, but it showed only a partial regression. After a discussion with the multidisciplinary team, we decided to treat the remnant tumor with a chemotherapy. The tumor began to be treated with a weekly paclitaxel and we are observing closely for the response. Bevacizumab is also under consideration.
Angiosarcoma of the face and the scalp is an aggressive tumor with a poor prognosis3,4,5,6,7,8,12. A local recurrence and a distant metastasis is frequent, and overall, a 5-year survival rate has been reported at between 12% to 34%3. The patients with a primary or an isolated eyelid angiosarcomas have a better prognosis when compared to those patients with a secondary eyelid involvement or those with a diffuse scalp and face tumors12. Angiosarcoma arising in the eyelid rarely extends centrifugally from the eyelid outward to other parts of the face, and they can be managed by a variety of surgical approaches which incorporates either a neoadjuvant or an adjuvant chemotherapy or a radiation12. Although angiosarcoma involving the eyelid progresses, an orbital involvement is rare and is seen in only 4% of cases12,13. Our patient had a recurrent angiosarcoma of a remote location on the eyelid without any sign of recurrence on the primary lesion after 3 years of surgical resection and radiation therapy.
In summary, in cases that angiosarcoma develops on the loose cutaneous tissue such as the periorbital area, it may show an edematous, purpuric or ecchymotic clinical manifestation rather than the nodular form. Thus, when the patient is presented with atypical eyelid lesions including a periocular edema or a discoloration, we should ask for the past medical history and include angiosarcomas in the differential diagnosis. Also, although the skin lesion seems to be resolved clinically after the treatment, physicians should perform a histopathologic evaluation to see whether there are any residual tumor cells.
Figures and Tables
 | Fig. 1Clinical photographs of recurrent angiosarcoma on the right eyelid. (A) Initial presentation. (B) After radiation treatment. |
 | Fig. 2Histopathological findings of the lesion before radiotherapy. (A, B) Numerous irregular anastomosing vascular channels lined by a single layer of enlarged atypical endothelial cells dissecting collagen bundles in the dermis (A: H&E, ×40; B: H&E, ×400). (C, D) Immunohistochemically, the tumor cells showed a positive reaction for CD31 (C: ×400) and D2-40 (D: ×400). |
References
1. Mendenhall WM, Mendenhall CM, Werning JW, Reith JD, Mendenhall NP. Cutaneous angiosarcoma. Am J Clin Oncol. 2006; 29:524–528.

2. Fuller CK, Charlson JA, Dankle SK, Russell TJ. Dramatic improvement of inoperable angiosarcoma with combination paclitaxel and bevacizumab chemotherapy. J Am Acad Dermatol. 2010; 63:e83–e84.

3. Mitra A, Ramnath R, Nicholson S, Yung A. An erythematous nodule on the eyelid. Clin Exp Dermatol. 2008; 33:87–89.

4. Lapidus CS, Sutula FC, Stadecker MJ, Vine JE, Grande DJ. Angiosarcoma of the eyelid: yellow plaques causing ptosis. J Am Acad Dermatol. 1996; 34:308–310.

5. Gündüz K, Shields JA, Shields CL, Eagle RC Jr, Nathan F. Cutaneous angiosarcoma with eyelid involvement. Am J Ophthalmol. 1998; 125:870–871.

6. Hiemstra CA, Mooy C, Paridaens D. Excisional surgery of periocular angiosarcoma. Eye (Lond). 2004; 18:738–739.

7. Conway RM, Hammer T, Viestenz A, Holbach LM, Conway RM. Cutaneous angiosarcoma of the eyelids. Br J Ophthalmol. 2003; 87:514–515.

8. Wiwatwongwana D, White VA, Dolman PJ. Two cases of periocular cutaneous angiosarcoma. Ophthal Plast Reconstr Surg. 2010; 26:365–366.

9. DeMartelaere SL, Roberts D, Burgess MA, Morrison WH, Pisters PW, Sturgis EM, et al. Neoadjuvant chemotherapy-specific and overall treatment outcomes in patients with cutaneous angiosarcoma of the face with periorbital involvement. Head Neck. 2008; 30:639–646.

10. Rosen A, Thimon S, Ternant D, Machet MC, Paintaud G, Machet L. Partial response to bevacizumab of an extensive cutaneous angiosarcoma of the face. Br J Dermatol. 2010; 163:225–227.

11. Koontz BF, Miles EF, Rubio MA, Madden JF, Fisher SR, Scher RL, et al. Preoperative radiotherapy and bevacizumab for angiosarcoma of the head and neck: two case studies. Head Neck. 2008; 30:262–266.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download