Abstract
Background
Various kinds of alopecia can show small round or oval hairless patch. Dermoscopy could be a simple, useful tool for making a correct diagnosis.
Objective
The aim of this study is to investigate clinical usefulness of dermoscopy for diseases with small round or oval hairless patch on the scalp.
Methods
Dermoscopic examination was performed for 148 patients with small round or oval hairless patch using DermLite® II pro. The type and its patient number of alopecia investigated in the study were as below: alopecia areata (n=81), trichotillomania (n=24), tinea captis (n=13), traction alopecia (n=12), lichen planopilaris (n=8), discoid lupus erythematosus (n=7), congenital triangular alopecia (n=2) and pseudopelade of Brocq (n=1). The significance of dermoscopic findings for each disease were evaluated.
Results
Characteristic dermoscopic findings of alopecia areata were tapering hairs and yellow dots. Those of trichotillomania and traction alopecia were broken hairs. Dermoscopic findings of tinea capitis included bent hairs, perifollicular white macules and greasy scales. Discoid lupus erythematosus and lichen planopilaris were characterized by dermoscopic findings of lack of follicular ostia. Furthermore, keratin plugs were frequently seen in discoid lupus erythematosus whereas perifollicular hyperkeratosis and erythema were frequently seen in lichen planopilaris.
The presence of a small round or oval hairless patch on the scalp can be observed in many diseases, such as alopecia areata (AA), trichotillomania (TM), tinea capitis (TC), traction alopecia (TA), lichen planopilaris (LPP), discoid lupus erythematosus (DLE), congenital triangular alopecia (CTA), and pseudopelade of Brocq (PB). In these diseases, the clinical diagnosis could be difficult if only a small round or oval hairless patch is present. Skin biopsy, KOH examination, and several laboratory tests could be performed to make the correct diagnosis. However, some of these approaches are invasive and not always available. Dermoscopy was recently introduced as a useful technique for diagnosing various hair and scalp diseases, including AA, TM, androgenic alopecia, TC, DLE, LPP, or inherited hair shaft dystrophies1,2,3,4,5,6. The reports did not emphasize the dermoscopic differences among various forms of alopecia, but focused only on describing the dermoscopic findings of each disease. Furthermore, we noted that no dermoscopic algorithmic approach has been used for examining small round or oval hairless patches on the scalp. Therefore, we performed a cross-sectional study to investigate the usefulness of dermoscopy as a clinical approach for examining small round or oval hairless patches on the scalp. In this study, various types of alopecia presenting as a small round or oval hairless patch were examined by using dermoscopy, and the significance of the dermoscopic findings of each disease was investigated.
This study was designed as a descriptive cross-sectional study involving 148 patients who visited the Pusan National University Hospital between January 2008 and December 2011 with a small round or oval hairless patch on the scalp that was clinically suspicious of AA. Among these patients, 81 had AA, 24 had TM, 13 had TC, 12 had TA, 8 had LPP, 7 had DLE, 2 had CTA, and 1 had PB. The diagnosis for each disease was based on clinical manifestations and detailed patient history. Additionally, skin biopsy was performed for all patients with TC, LPP, DLE, and PB; KOH examination and fungal culture were also done for those with TC. Ninety-nine patients were women, and 49 were men. The age of the patients was 1 to 85 years (mean age, 30 years). Dermoscopic examination was performed for all the patches of the 148 patients, and characteristic dermoscopic findings were analyzed by 2 experienced dermatologists (WH Shim and MB Kim). The dermoscopy equipment used in this study was DermLite II Pro (3Gen, San Juan Capistrano, CA, USA), which is able to interrupt reflected light without the use of immersion gels. Statistical analysis was restricted to a few patients in each group. All procedures were approved by the institutional review board of the Pusan National University Hospital.
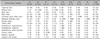
The characteristic dermoscopic findings for each disease are summarized in Table 1.
Yellow dots, clustered short vellus hairs, black dots, and tapering hairs were observed in 62%, 48%, 42%, and 40% of the 81 patients with AA, respectively (Fig. 1). Broken hairs were observed in all of the 24 patients with TM. Broken hairs showed characteristic split ends (Fig. 2). There were 12 patients with TA in this study, and the dermoscopic examination of their hairless patch showed broken hairs (100%) and black dots (92%) (Fig. 3). Greasy scales, bent hairs, and perifollicular white macules were observed in 100%, 62%, and 46% of the 13 patients with TC, respectively (Fig. 4). In the 7 patients with DLE, lack of follicular ostia (100%) and keratin plugs (86%) were observed (Fig. 5). Lack of follicular ostia, perifollicular hyperkeratosis, and perifollicular erythema was observed in 100%, 88%, and 88% of the 8 patients with LPP, respectively (Fig. 6). Dermoscopic examination of 2 patients with CTA revealed clustered short vellus hairs without other specific findings in both of them (Fig. 7). There was 1 woman with PB in this study, and the dermoscopic examination for her small round or oval hairless patch revealed a lack of follicular ostia without any other specific findings (Fig. 8).
Tapering hairs were observed only in patients with AA (40%, 32 of 81). Patients with TM (100%, 24 of 24), TA (100%, 12 of 12), TC (8%, 1 of 13), and AA (2%, 2 of 81) showed broken hairs. Bent hairs were observed only in patients with TC (62%, 8 of 13). Black dots were observed in several patients, including those with TA (92%, 11 of 12), TM (46%, 11 of 24), AA (42%, 34 of 81), TC (38%, 5 of 13), DLE (29%, 2 of 7), and LPP (13%, 1 of 8). Clustered short vellus hairs were observed in patients with CTA (100%, 2 of 2), AA (48%, 39 of 81), TA (42%, 5 of 12), TM (33%, 8 of 24), and TC (23%, 3 of 13). Lack of follicular ostia was observed in patients with LPP (100%, 8 of 8), DLE (100%, 7 of 7), PB (100%, 1 of 1), TC (15%, 2 of 13), and AA (12%, 10 of 81). Only patients with DLE showed keratin plugs (86%, 6 of 7). Yellow dots were observed in patients with AA (62%, 50 of 81), TM (25%, 6 of 24), and TA (17%, 2 of 12). Perifollicualr hyperkeratosis was observed only in patients with LPP (88%, 7 of 8), whereas perifollicular erythema was observed in those with LPP (88%, 7 of 8), AA (4%, 3 of 81), and TM (4%, 1 of 24). Perifollicular white macules (46%, 6 of 13) and greasy scales (100%, 13 of 13) were observed only in patients with TC. Atypical red vessels were observed in patients with DLE (71%, 5 of 7), LPP (63%, 5 of 8), TC (23%, 3 of 13), TA (8%, 1 of 12), AA (4%, 3 of 81), and TM (4%, 1 of 24).
The presence of a small round or oval hairless patch can be observed in various forms of alopecia, and it could be diagnostic conundrum for dermatologists. Dermoscopy could be a useful ancillary method for the improvement of diagnostic accuracy. However, no dermoscopic algorithmic approach has been established for examining small round or oval hairless patches on the scalp. Therefore, we propose a dermoscopic algorithm for examining this condition (Fig. 9). In accordance with the specificity of each dermoscopic finding, we believe that hair shaft abnormality should be checked first. This is because AA, TM, TA, and TC are the most common diseases presenting with a small round or oval hairless patch, and dermoscopic findings of hair shaft abnormality could be especially helpful in the diagnosis of these diseases. Second, it is important to check for the lack of follicular ostia to differentiate between scarring alopecia and nonscarring alopecia, and for the diagnosis of scarring alopecia such as DLE and AA. Lastly, changes in the perifollicular area and scales could give additional clues for the diagnosis of other diseases. This algorithm is very simple, and could be helpful as a clinical approach to examine a variety of alopecia types presenting with a small round or oval hairless patch on the scalp.
In this study, we observed a few characteristic dermoscopic findings of hair shaft abnormalities in small round or oval hairless patches. Tapering hairs are known to be the most specific dermoscopic finding of AA1, and result from follicular damage in anagen and rapid transformation to telogen1. In this study, tapering hairs were only observed in patients with AA. Tapering hairs, also named as 'exclamation mark hairs', could be observed with the naked eye; however, their characteristic feature of narrowing of the hair shaft towards the hair follicle is more readily perceived with dermoscopy. Lee et al.2 previously reported that broken hairs are a characteristic finding of TM. In this study, broken hairs were also frequently observed in patients with TM and TA. Bent hairs are the most specific finding of TC, and are characterized by bending of the hair shaft with homogenous thickness and pigmentation. Slowinska et al.4 previously reported a similar dermoscopic finding, which they called 'comma hairs'. They proposed that comma hairs are due to the cracking and bending of hair shafts filled with the hyphae of Microsporum canis4. However, we also observed bent hair shafts without shortening in patients with TC. Therefore, we prefer the term 'bent hairs' rather than 'comma hairs' in this study. Black dots are believed to be remnants of hair shafts arising from tapering hairs, broken hairs, and bent hairs1. In this study, black dots were observed in patients with TA, TM, AA, TC, DLE, and LPP. Therefore, black dots seem to be a nonspecific dermoscopic finding. Clustered short vellus hairs are known to be indicative of hair regrowth in nonscarring alopecia1. They were observed in patients with CTA, AA, TA, TM, and TC in this study.
In the absence of characteristic dermoscopic findings of hair shafts, identification of the presence or absence of follicular ostia could be helpful. Lack of follicular ostia is indicative of scarring alopecia5. In addition, in this study, the lack of follicular ostia was frequently observed in cases of scarring alopecia such as DLE, LPP, and PB. For alopecia, the discrimination between scarring alopecia and nonscarring alopecia may take precedence over the others7. However, few diseases considered nonscarring alopecia could be misdiagnosed as scarring alopecia8. For example, lack of follicular ostia was observed in some patients with AA in this study, and we observed that patients with long-standing androgenic alopecia could present with dermoscopic findings of lack of follicular ostia (data not shown). Therefore, we suggest that it is important to check for other dermoscopic findings to make the correct diagnosis.
Perifollicular change could be observed by using dermoscopy in some diseases. Dermoscopic findings of perifollicular change include keratin plugs, yellow dots, perifollicular hyperkeratosis, perifollicular erythema, and perifollicular white macules. Keratin plugs are known to be a specific finding of DLE5. Moreover, keratin plugs were observed only in patients with DLE in this study. Keratin plugs are believed to be associated with pilosebaceous atrophy through the inflammatory process9. Yellow dots are reported as a specific finding of AA1; however, they were also observed in patients with TM and TA in this study. Yellow dots are believed to be the result of follicular ostia filled with incompletely differentiated hair shafts and sebum1. Inui et al.1 reported the dermoscopic finding of yellow dots in patients with AA, TM, and androgenic alopecia, and suggested that yellow dots in patients with TM are different from those in patients with AA, because they contain black dots. However, in this study, yellow dots not containing black dots were also observed in some patients with TM. In this study, both perifollicular hyperkeratosis and perifollicular erythema were only observed in patients with LPP; the former represent perifollicular fibroplasias and scarring, whereas the latter represent perifollicular inflammation10. We proposed the new dermoscopic term 'perifollicular white macules', a description for whitish round or oval structure with hair in the center, which are thought to be a result of fungal infection of the hair bulb and pus formation11. Perifollicular white macules were observed only in patients with TC in this study.
Dermoscopic findings of scales, pigments, and vessels were also investigated in this study. Greasy scales were frequently observed in patients with TC. Pigment networks and atypical red vessels were also observed in some patches. However, we could not find the importance of these 2 findings for differentiating between diseases.
Among several diseases manifesting similar symptoms, an algorithmic approach facilitates stepwise identification of factors indicating a specific disease. Therefore, algorithmic approaches are widely used for many groups of diseases to differentiate between them. For making a diagnosis among the several diseases presenting with a small round or oval hairless patch on the scalp, we felt the need of a dermoscopic algorithm for a more rapid and accurate diagnosis; however, we could not find such an algorithm. Therefore, we created a dermoscopic algorithm for examining small round or oval hairless patches on the basis of the results of this study. This algorithm is first proposed in this study, and it is designed to determine the important dermoscopic findings indicating specific diseases via 3 simple steps. This algorithm is very simple, and could be very useful for dermatologists dealing with various kinds of alopecia.
This study has several limitations. Other diseases could show the presence of small round or oval hairless patches, which were not investigated in this study. However, we were trying to evaluate the dermoscopic findings of common diseases. The patients recruited in this study were all Asians with black hair. The frequency of some dermoscopic findings such as yellow dots and black dots would be different in other races. Furthermore, the small number of patients in some disease groups restricts statistical analysis.
We determined the characteristic dermoscopic findings of several diseases presenting with a small round or oval hairless patch. The algorithm prepared on the basis of these results will be helpful as a clinical approach for examining small round or oval hairless patches.
Figures and Tables
Fig. 1
Dermoscopic features of alopecia areata; yellow dots (A; arrow), clustered vellus hairs (B; dotted circle), black dots (C; triangle), and tapering hairs (D; white arrow).

Fig. 4
Dermoscopic features of tinea capitis; greasy scales (A; arrow), perifollicular white macules (B; triangles) and bent hairs (C; white arrow).
Fig. 5
Dermoscopic features of discoid lupus erythematosus; keratin plugs (arrow), lack of follicular ostia (dotted circle) and pigment network (triangle).

Fig. 6
Dermoscopic features of lichen planopilaris; perifollicular hyperkeratosis (arrow), perifollicularerythema (triangle) and lack of follicular ostia (dotted circle).

Fig. 7
Dermoscopic features of congenial triangular alopecia; clustered short vellus hairs without otherspecific findings (dotted circle).

Fig. 8
Dermoscopic features of pseudopelade of Brocq; lack of follicular ostia (dotted circle) without otherspecific finding.

Fig. 9
The algorithm for dermoscopy of small round or oval hairless patch on the scalp. AA: alopecia areata, TM: trichotillomania, TA: traction alopecia, TC: tinea capitis, CTA: congenital triangular alopecia, DLE: discoid lupus erythematosus, LPP: lichen planopilaris, PB: pseudopelade of Brocq.

References
1. Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: analysis of 300 cases. Int J Dermatol. 2008; 47:688–693.

2. Lee DY, Lee JH, Yang JM, Lee ES. The use of dermoscopy for the diagnosis of trichotillomania. J Eur Acad Dermatol Venereol. 2009; 23:731–732.

3. Lacarrubba F, Dall'Oglio F, Rita Nasca M, Micali G. Videodermatoscopy enhances diagnostic capability in some forms of hair loss. Am J Clin Dermatol. 2004; 5:205–208.

4. Slowinska M, Rudnicka L, Schwartz RA, Kowalska-Oledzka E, Rakowska A, Sicinska J, et al. Comma hairs: a dermatoscopic marker for tinea capitis: a rapid diagnostic method. J Am Acad Dermatol. 2008; 59:S77–S79.
5. Duque-Estrada B, Tamler C, Sodré CT, Barcaui CB, Pereira FB. Dermoscopy patterns of cicatricial alopecia resulting from discoid lupus erythematosus and lichen planopilaris. An Bras Dermatol. 2010; 85:179–183.
6. Wallace MP, de Berker DA. Hair diagnoses and signs: the use of dermatoscopy. Clin Exp Dermatol. 2010; 35:41–46.

7. Stefanato CM. Histopathology of alopecia: a clinicopathological approach to diagnosis. Histopathology. 2010; 56:24–38.

8. Fanti PA, Tosti A, Bardazzi F, Guerra L, Morelli R, Cameli N. Alopecia areata. A pathological study of nonresponder patients. Am J Dermatopathol. 1994; 16:167–170.
9. Bielsa I, Herrero C, Collado A, Cobos A, Palou J, Mascaró JM. Histopathologic findings in cutaneous lupus erythematosus. Arch Dermatol. 1994; 130:54–58.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download