Abstract
Background
In the majority of melanomas, the RAS/RAF/MEK/ERK signaling pathway is constitutively activated, due to oncogenic mutations in the BRAF and NRAS genes. The BRAF mutation has been mainly described in Caucasian melanomas. However, there is a lack of study evaluating the status, and the clinical significance, of BRAF mutation in the Asian population.
Objective
This study was aimed to determine the frequency of BRAF mutation, and to evaluate the correlation of BRAF status with clinicopathologic features and outcomes, in Korean primary acral lentiginous melanoma (ALM) patients.
Methods
ALM samples (n=36) were analyzed for the BRAF V600E mutation, by dual-priming oligonucleotide (DPO) based real-time polymerase chain reaction. The clinicopathologic features and prognosis of the patients were analyzed with BRAF mutation status.
Results
The incidence of BRAF V600E mutation was 19.4% (7/36). The BRAF V600E mutations were not associated with clinicopathologic features, except for the age factor. All of the BRAF-mutant patients survived without recurrence or metastasis, and have a better clinical outcome than BRAF wild-type patients.
Conclusion
In Korean primary ALM, a low frequency of BRAF mutation was shown; and BRAF mutation presented with a favorable prognosis. These results indicate that other distinctive genetic mechanisms may have more important roles in the development and progression of disease. Further multicenter study with large sample size is firmly needed, to confirm the results of our preliminary study.
Cutaneous melanoma is a potentially fatal neoplasm, with a complex and heterogeneous etiology. Several genes and signaling cascades, including the RAS/RAF/MEK/ERK signaling pathway, have been implicated in the pathogenesis of cutaneous melanoma. Somatic oncogenic mutations of BRAF have been identified most commonly in primary human melanomas, where mutational frequencies have been reported to be as high as 70%1,2. All the mutations were found within the kinase domain of BRAF, with a single substitution (T to A) of glutamate for valine at codon 600 (V600E) being responsible for 90% of the observed mutation1. This mutated kinase promotes constitutive ERK signaling, stimulating proliferation and survival, and providing essential tumor growth.
In the Asian population, the incidence of cutaneous melanoma is much lower than in the Caucasian population. Furthermore, the clinical and histological types of melanoma vary among different ethnicities, such that Caucasian patients are often afflicted with superficial spreading melanoma and nodular melanoma, whereas Asian patients present with acral lentiginous melanoma (ALM). Recent studies have revealed that the frequency of BRAF mutation in ALM was lower than in other types of melanoma3,4, and the effects of mutation on clinicopathologic features and clinical outcome remain uncertain, with previous studies reporting conflicting results2,5,6,7,8,9. However these observations are mostly conducted in Caucasian populations, and there have been few studies about the status and clinical significance of BRAF mutation in Asian patients10,11,12,13,14.
Furthermore, there has been only one report about the effects of BRAF mutations on the clinical features and outcome of melanoma in Korean patients13. Thus, the purpose of this study was to determine the frequency of BRAF mutation, and to evaluate the clinical significance of BRAF mutation in Korean primary ALM patients.
We retrospectively analyzed the clinical records of 36 patients who had been treated for pathologically proven melanoma that occurred in acral site at Dong-A University Medical Center (Busan, Korea), between July 1997 and October 2008. Clinical data, including age, sex, American Joint Committee on Cancer (AJCC) pathologic stage15, thickness (Breslow), ulceration, recurrence or metastasis of disease after initial diagnosis, and survival (follow-up persisted until September 2011, or until the missing of follow-up, or death of patients), were collected. This study was approved by the institutional review board of Dong-A University Medical Center (IRB 12-032), and written informed consent was obtained from all patients.
Thirty-six tumor specimens were obtained as surgical biopsies. For each case, formalin fixed, paraffin wax embedded sections (10 µm thick) were cut, using a sterile microtome blade, with two sections used for each sample. Each method was run three times, to ensure reproducibility.
The commercial QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) was used for DNA extraction, according to the manufacturer's protocol. The tissues were dewaxed with two washes of xylene, followed by the addition of 1 ml of 100% ethanol, to remove residual xylene. After dewaxing, tissues were digested with 200 µl of ALT buffer, containing proteinase K at 200 µg/ml, overnight, at 56℃. After digestion, 200 µl of AL buffer was added, and incubated at 70℃ for 10 minutes, followed by mixing with 200 µl of 100% ethanol. The solution was transferred into a spin column, centrifuged for one minute, and washed with AW1 and AW2 buffers. DNA was eluted with 200 µl of AE buffer preheated to 70℃, and further incubated at 70℃ for five minutes, before collection by centrifugation. The buffers and the proteinase were provided in the extraction kit.
The BRAF V600E mutation was detected using Anyplex™ BRAF V600E Real time detection system (Seegene Inc., Seoul, Korea). The reaction mixture was prepared as follows: for 1 reaction, the mixture contained 2 µl of 10X BRAF Oligo Mix (OM) containing amplification and detection reagents, 3 µl of 8-methoxypsoralen (8-Mop) solution to prevent carryover contamination, 10 µl of 2X Anyplex polymerase chain reaction (PCR) Master Mix (Seegene Inc.) containing DNA polymerase, and buffer with deoxynucleoside triphosphates. The reaction mixture tube was agitated, by inverting it 5 times, or by quick vortexing. 15 µl of the reaction mixture was dispensed into 0.2-ml PCR tubes. 15 µl of each sample's nucleic acid was added to the reaction mixture tube, in order to reach a total reaction volume of 20 µl. Real-time PCR was performed on a CFX96™ real-time PCR System (Bio-Rad, Hercules, CA, USA), under the following conditions: 15 min at 95℃, followed by 15 cycles of 15 seconds at 95℃, and 30 seconds at 60℃, and then 35 cycles of 30 seconds at 95℃, and 32 seconds at 60℃.
Data were summarized using descriptive statistics: frequency and percentage for categorical variables, and mean and standard deviation for continuous variables. Differences in patients' demographic and clinical characteristics were compared across subgroups, with Fisher's exact test for categorical variables, and t-test for continuous variables. Survival was estimated, using Kaplan-Meier curves. The associations of BRAF mutation and other clinicopathological factors with survival were also analyzed, using the Cox proportional hazards regression model. The 95% confidence intervals for hazard ratios were calculated, and reported, for the multivariate statistical model. Overall survival (OS) was defined as the time from date of first diagnosis, to death. Disease free survival (DFS) was defined as the time from date of first diagnosis, to local recurrence or metastasis, or death. Survival curves were compared between groups, using the log-rank test. All p-values less than 0.05 were considered statically significant. All statistical analyses were carried out using PASW Statistics 18.0 version (IBM Co., Armonk, NY, USA) and MedCalc 11.6.1 version (MedCalc Software, Mariakerke, Belgium) statistical software.
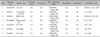
A total of 36 patients with primary ALM were included in this study (15 men and 21 women). The mean age at diagnosis of all patients was 58.2 years (range: 16~85 years); and all tumors were located in the acral area (hand: 36.1% and foot: 63.9%) (Table 1). Primary ALM lesions from a total of 36 patients were screened for BRAF V600E mutations, using dual-priming oligonucleotide (DPO)-based real-time PCR. BRAF V600E mutations were detected in 7 of the 36 patients (19.4%). The characteristics of the BRAF mutant patients are shown in Table 2.
Only the mean age was significantly different between patients with BRAF mutations, and those without BRAF mutations; while other clinicopathologic features, including sex (p=0.42), site (p=0.86), tumor thickness (mean tumor thickness: p=0.99 and Breslow thickness: p=0.70), presence of ulceration (p=1.00), and AJCC pathologic stage (p=0.69), were not. The mean age (45.6±14.7 years) of patients bearing BRAF mutations was younger, than that of patients without BRAF mutations (61.2±13.5 years; p=0.01). The mean tumor thickness (4.1±3.2 mm) of patients with BRAF mutations was thicker, than that of patients without BRAF mutations (4.0±3.9 mm; p=0.99); while the proportion of Breslow thickness that was more than 2.01 mm in the non-BRAF mutant group (72.4%), was higher than that in the BRAF mutant group (57.2%; p=0.70) (Table 1).
The recurrence, metastasis and survival data were collected for patients who were diagnosed as primary ALM, from the first time of diagnosis as melanoma, to September 2011.
Thirteen (36.2%) of the 36 patients were lost to follow-up. The median follow-up period was 65 months (range: 1~146 months). Overall, local recurrence occurred in 5 patients (13.9%), and 8 patients (22.2%) developed distant metastasis. Seven (19.4%) of the 36 patients are known to have died (Table 1). Among the 7 patients with BRAF mutation, all of the 5 patients who were able to be followed-up were alive, without recurrence or metastasis (Table 1, 2). We found that the patients with BRAF mutation tended to have a better OS (p=0.071), and had a better DFS (p=0.045), than patients with wild-type tumors (Fig. 1). The Cox multivariate analysis of the prognostic factors (BRAF mutation, sex, age, Breslow thickness, pathological T stage, pathological TNM stage, and ulceration) for OS and DFS are shown in Table 3, 4, respectively. In this study, we could not check whether the BRAF mutation is a prognostic factor, or not, for OS and DFS in the Cox's multivariate analysis, because the events (local recurrence, metastasis, and death) did not occur in BRAF mutant patients. But, OS of the ALM patients was associated with several factors in Cox multivariate analyses (Table 3), and age and Breslow thickness of the tumor significantly correlated with OS. Similarly, DFS was also associated with several prognostic factors in Cox multivariate analyses (Table 4), with age and Breslow thickness showing a significant correlation with DFS.
In the last decade, significant progress has been made in understanding of the genetic alterations in melanocytic tumors. The most exciting finding is the discovery of oncogenic BRAF and NRAS mutations in melanoma. A number of recent studies have shown that the RAS/RAF/MEK/ERK signaling pathway plays a crucial role in melanoma development, with ERK being constitutively activated in up to 90% of melanoma16. In melanoma, ERK activation is most commonly due to mutations of NRAS, and especially, BRAF genes1.
The RAF family of serine/threonine protein kinase are components of a kinase signaling cascade that links extracellular signals to downstream cellular effectors. In mammals, there are three highly conserved RAR genes: ARAF, BRAF, and CRAF. The BRAF gene encodes a serine/threonine kinase involved in signaling from RAS to ERK signaling pathway. BRAF signaling regulates a variety of cellular processes, including growth, differentiation and apoptosis17. The most common BRAF mutation, which accounts for more than 90% of cases of cancer involving this gene, is glutamic acid for valine substitution, at position 600 (V600E)1. BRAF V600E has elevated kinase activity, when compared with wild type BRAF;1 and it induces constitutive ERK signaling, through hyperactivation of the RAS/RAF/MEK/ERK pathway, stimulating proliferation, survival and transformation. BRAF is mutated in up to 70% of primary human melanoma1,2, and surprisingly, a high frequency of BRAF mutation has also been reported in common benign nevi18. However, BRAF V600E induces senescence in benign nevi, through transcriptional upregulation of cell cycle inhibitor p16INK4a19,20. Thus, BRAF plays an important role in cancer induction, maintenance and progression, given that it is mutated early in the initiation process. However, oncogenic BRAF by itself is not sufficient for cancer, and must cooperate with other processes, to induce the fully cancerous state.
Recent studies by Boris Bastian's group have revealed that there exist site-specific genetic alterations in melanoma21,22,23. They classified melanomas into four groups: melanoma on skin with chronic sun-damage (CSD melanoma), melanoma on skin without chronic sun-damage (non-CSD melanoma), melanoma on palms, soles and nail bed (acral melanoma), and melanoma on mucous membrane (mucosal melanoma). Non-CSD melanoma roughly corresponds to superficial spreading melanoma, CSD melanoma to lentigo maligna melanoma, and acral melanoma to ALM. They found that non-CSD melanomas were characterized by the high frequency of BRAF mutations (reaching up to 75%); and ALM (23%), mucosal (11%) and CSD melanoma (11%) showed a low frequency of BRAF mutation21,22,23. It was concluded that BRAF mutations are associated with acral melanomas originating in areas of repetitive acute sun exposure; but not in areas with chronic ultraviolet radiation (UVR) exposure, or those are protected from UVR altogether. Other studies have also revealed that the frequency of BRAF mutation in ALM was lower, than in other types of melanoma3,4. Most of these studies are conducted in the Caucasian population, but there have been only few reports about BRAF mutation in Asian patients10,11,12,13,14. In the Asian population, the most common type of melanoma is ALM; and to our knowledge, there is only one report about the status and the clinical significance of BRAF mutation in melanoma of the Korean population13. So, we determined the frequency of BRAF V600E mutation in ALM by DPO based real-time PCR, and the incidence of BRAF mutation was found to be 19.4%. According to recent studies conducted in Asian populations, the frequencies of BRAF mutation in ALM were 15.5% to 15.7%10,11. These results were similar to the previous Western studies. Notwithstanding the methodological difference between sequencing and PCR for detecting BRAF mutation, the result of our study is sufficient to explain the low frequency of the BRAF mutation seen in ALM Korean patients. Benlloch et al.24 compared the frequency of the BRAF mutation between the PCR and sequencing. There was no significant difference in the frequency of the BRAF mutation between the two groups. Because ALMs have a low frequency of BRAF mutations, it can be suggested that the activation of other distinctive genetic mechanisms serves an independent oncogenic function in ALMs lacking BRAF or NRAS mutations. In addition, these findings support the notion that divergent molecular pathways exist during melanoma development, which would explain the heterogeneous nature of this malignancy, which has been observed clinically.
Previously, several studies have been carried out to examine whether mutations in BRAF confer different pathological features and clinical behavior. The effects of its mutation on clinicopathologic features and clinical outcome remain uncertain, with previous studies reporting conflicting results2,5,6,7,8,9. Some reports have shown that the BRAF mutation is associated with thinner tumor thickness, and lower rate of proliferation5,9; and these observations indicate that BRAF mutation may be associated with a more differentiated form of melanoma, with a slower cell proliferation rate. However, other studies were not able to find any association2,6. In this study, despite the statistical insignificance between the two groups, the proportion of Breslow thickness of more than 2.01 mm was lower in BRAF mutant patients, compared with wild type. Previous studies reveal that BRAF mutations were found to be inversely correlated with patients' age2,8,9,23,25. Although the close relationships of patient age, anatomic site, and sun-induced damage have made it difficult to segregate their individual associations with BRAF mutations, Bauer et al.25 have recently confirmed that patient age is independently associated with BRAF mutation frequency. We can also observe that BRAF mutant patients were younger, than BRAF wild-type patients. However, there was no significant association between BRAF mutations, and other clinicopathologic features.
In the majority of studies, BRAF mutations in primary melanoma have no apparent impact on DFS and OS2,5,6,8. Furthermore, a recent study by Jin et al.13 examined BRAF and KIT mutations in 202 Korean patients, and found no prognostic impact on BRAF mutation status, by multivariate analysis. In our study, we could not check whether or not the BRAF mutation is a prognostic factor for OS and DFS in the Cox's multivariate analysis, because the events (local recurrence, metastasis, and death) did not occur in BRAF mutant patients, and the number of patients in our study was too small for analysis. But, in the Kaplan-Meier curve, the BRAF mutant patients had a better clinical outcome, than BRAF wild patients. Our study showed that the BRAF mutant patients were younger, than BRAF wild patients. Moreover, in our study, younger patients had a better clinical outcome. We thought that this resulted from the differences in the melanoma sites and histological subtypes of the study population, between previous studies, and our study.
In addition, our data showed that BRAF wild type patients tend to have thicker tumor, compared with BRAF mutant patients, albeit without statistical significance. A large number of previous studies reported that NRAS mutations were associated with thicker tumor and higher mitotic rate, when compared to BRAF mutation2,5. Also, Devitt et al.5 identified that the presence of NRAS mutations is an adverse prognostic factor, leading to shorter melanoma specific survival. In general, BRAF and NRAS mutations are mutually exclusive; thus, the effect of these mutations on clinical outcomes may be different. Furthermore, previous studies demonstrated that the NRAS mutations were associated with thicker tumor, older age, and poor clinical outcome, compared to BRAF mutation2,5.
In conclusion, we assumed in our study that the BRAF wild patients might have NRAS mutation, which suggests that additional study on the NRAS mutation in ALM could be necessary, to confirm the effects of RAS/RAF/MEK/ERK signaling pathway on clinical outcome. Though a large scale analysis study on the survival rates associated with BRAF and NRAS mutation was conducted in Asian patients, the study included all types of melanoma, in contrast to this study, which included only ALM10. In addition, because the incidence of melanoma is far lower in the Asian, than in the Western population, and there are few systemic studies on the ALM and its survival rates associated with these mutations, further multicenter studies with larger sample size are needed, to confirm the result of this preliminary study in Korea.
Because the ALM has a low frequency of BRAF mutations, the potential therapeutic targets may be different from other types of melanoma. However, there are suggestions that ALM is also likely to be a target of BRAF kinase inhibitors, for the reason that in the majority of ALM, the RAS/RAF/MEK/ERK pathway is constitutively activated26. The stronger relationship between the RAS/RAF/MEK/ERK pathway and the ALM would be confirmed through additional NRAS mutation study in Korean patients, so that the BRAF kinase (e.g. Sorafenib) and selective RAF inhibitor (e.g. PLX4032, GSK2118436) could be reasonable treatments.
We acknowledge a number of limitations to our study. This study was a single-center study, with a limited number of patients. In addition, the incidence of melanoma is far lower in the Korean, than in the Western population; and there is a lack of systemic studies on ALM in Korea. For these reasons, we could not absolutely demonstrate the results of our study. Therefore, a multicenter study with a large sample size should be performed, to confirm the results of our preliminary study in Korea.
So in conclusion, a low frequency of BRAF mutation was shown, and BRAF mutation presented with a favorable prognosis in Korean primary ALM. These results indicate that other distinctive genetic mechanisms may have more important roles, in the development and progression of disease. So, further study is warranted into the molecular characterization of ALM, including the examination of CCND1, PTEN and KIT; as aberrations of these genes are likely to interact with BRAF and NRAS, to further drive clinical outcome.
Figures and Tables
Fig. 1
Kaplan-Meier curve for overall survival and disease free survival across subgroup, based on BRAF mutation.

References
1. Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, et al. Mutations of the BRAF gene in human cancer. Nature. 2002; 417:949–954.

2. Edlundh-Rose E, Egyházi S, Omholt K, Månsson-Brahme E, Platz A, Hansson J, et al. NRAS and BRAF mutations in melanoma tumours in relation to clinical characteristics: a study based on mutation screening by pyrosequencing. Melanoma Res. 2006; 16:471–478.

3. Saldanha G, Potter L, Daforno P, Pringle JH. Cutaneous melanoma subtypes show different BRAF and NRAS mutation frequencies. Clin Cancer Res. 2006; 12:4499–4505.

4. Lang J, MacKie RM. Prevalence of exon 15 BRAF mutations in primary melanoma of the superficial spreading, nodular, acral, and lentigo maligna subtypes. J Invest Dermatol. 2005; 125:575–579.

5. Devitt B, Liu W, Salemi R, Wolfe R, Kelly J, Tzen CY, et al. Clinical outcome and pathological features associated with NRAS mutation in cutaneous melanoma. Pigment Cell Melanoma Res. 2011; 24:666–672.

6. Akslen LA, Angelini S, Straume O, Bachmann IM, Molven A, Hemminki K, et al. BRAF and NRAS mutations are frequent in nodular melanoma but are not associated with tumor cell proliferation or patient survival. J Invest Dermatol. 2005; 125:312–317.

7. Kumar R, Angelini S, Czene K, Sauroja I, Hahka-Kemppinen M, Pyrhönen S, et al. BRAF mutations in metastatic melanoma: a possible association with clinical outcome. Clin Cancer Res. 2003; 9:3362–3368.
8. Long GV, Menzies AM, Nagrial AM, Haydu LE, Hamilton AL, Mann GJ, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011; 29:1239–1246.

9. Liu W, Kelly JW, Trivett M, Murray WK, Dowling JP, Wolfe R, et al. Distinct clinical and pathological features are associated with the BRAF(T1799A(V600E)) mutation in primary melanoma. J Invest Dermatol. 2007; 127:900–905.

10. Si L, Kong Y, Xu X, Flaherty KT, Sheng X, Cui C, et al. Prevalence of BRAF V600E mutation in Chinese melanoma patients: large scale analysis of BRAF and NRAS mutations in a 432-case cohort. Eur J Cancer. 2012; 48:94–100.

11. Qi RQ, He L, Zheng S, Hong Y, Ma L, Zhang S, et al. BRAF exon 15 T1799A mutation is common in melanocytic nevi, but less prevalent in cutaneous malignant melanoma, in Chinese Han. J Invest Dermatol. 2011; 131:1129–1138.

12. Zhou QM, Li W, Zhang X, Chen YB, Chen XC, Guan YX, et al. The mutation profiles of common oncogenes involved in melanoma in southern China. J Invest Dermatol. 2012; 132:1935–1937.

13. Jin SA, Chun SM, Choi YD, Kweon SS, Jung ST, Shim HJ, et al. BRAF mutations and KIT aberrations and their clinicopathological correlation in 202 Korean melanomas. J Invest Dermatol. 2013; 133:579–582.

14. Ashida A, Uhara H, Kiniwa Y, Oguchi M, Murata H, Goto Y, et al. Assessment of BRAF and KIT mutations in Japanese melanoma patients. J Dermatol Sci. 2012; 66:240–242.

15. Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009; 27:6199–6206.

16. Cohen C, Zavala-Pompa A, Sequeira JH, Shoji M, Sexton DG, Cotsonis G, et al. Mitogen-actived protein kinase activation is an early event in melanoma progression. Clin Cancer Res. 2002; 8:3728–3733.
17. Peyssonnaux C, Eychène A. The Raf/MEK/ERK pathway: new concepts of activation. Biol Cell. 2001; 93:53–62.

18. Pollock PM, Harper UL, Hansen KS, Yudt LM, Stark M, Robbins CM, et al. High frequency of BRAF mutations in nevi. Nat Genet. 2003; 33:19–20.

19. Michaloglou C, Vredeveld LC, Soengas MS, Denoyelle C, Kuilman T, van der Horst CM, et al. BRAFE600-associated senescence-like cell cycle arrest of human naevi. Nature. 2005; 436:720–724.

20. Gray-Schopfer VC, Cheong SC, Chong H, Chow J, Moss T, Abdel-Malek ZA, et al. Cellular senescence in naevi and immortalisation in melanoma: a role for p16? Br J Cancer. 2006; 95:496–505.

21. Curtin JA, Fridlyand J, Kageshita T, Patel HN, Busam KJ, Kutzner H, et al. Distinct sets of genetic alterations in melanoma. N Engl J Med. 2005; 353:2135–2147.

22. Bastian BC, Olshen AB, LeBoit PE, Pinkel D. Classifying melanocytic tumors based on DNA copy number changes. Am J Pathol. 2003; 163:1765–1770.

23. Maldonado JL, Fridlyand J, Patel H, Jain AN, Busam K, Kageshita T, et al. Determinants of BRAF mutations in primary melanomas. J Natl Cancer Inst. 2003; 95:1878–1890.

24. Benlloch S, Payá A, Alenda C, Bessa X, Andreu M, Jover R, et al. Detection of BRAF V600E mutation in colorectal cancer: comparison of automatic sequencing and real-time chemistry methodology. J Mol Diagn. 2006; 8:540–543.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download