Abstract
Background
In cutaneous malignant melanoma (MM) with clinically uninvolved regional lymph nodes, sentinel lymph node (SLN) status is the most powerful indicator of both overall survival (OS) and disease-free survival (DFS). However, no studies on the long-term survival and clinical follow-up of Korean patients with acral lentiginous MM (ALM) undergoing SLN biopsy (SLNB) have been published.
Objective
The purpose of this study was to investigate the clinical prognosis and long-term survival of Korean patients with ALM according to SLN status.
Methods
Thirty-four ALM patients undergoing SLNB were included in this study. We evaluated clinical and histopathological follow-up data such as the stage of disease, treatment, recurrence, and metastasis, and analyzed OS and DFS according to SLN status.
Results
The median follow-up time was 60.5 months (range 3~127 months). Positive SLNs were noted in 14 patients (41.2%). Patients with negative SLNs had better OS and DFS than those with positive SLNs (p<0.05). Increased Breslow thickness was associated with short OS and DFS (p<0.05), and female patients showed better DFS than male patients (p<0.05).
The incidence of primary cutaneous malignant melanoma (MM) has been increasing dramatically worldwide for several decades. However, the increments in Asian countries such as Korea are steady and not as high as those in Western countries1,2. In Korea, the most common type of MM is acral lentiginous MM (ALM) on the hands and feet, in contrast to Western countries3. Cutaneous MM is one of the most aggressive human cancers, with high and early metastatic potential. Therefore, accurate staging and optimal management are the ultimate goals for improving overall survival (OS).
The sentinel lymph node (SLN) is defined as the first node in the lymphatic basin into which the primary tumor drains. Among the main prognostic factors for primary cutaneous MM, such as Breslow thickness, ulceration, and mitosis, the presence or absence of melanoma cells in lymph nodes draining the primary tumor site is the strongest predictor of both OS and risk of recurrence4,5. Since it was first reported by Morton et al.6 in 1992, SLN biopsy (SLNB) has been widely accepted as a minimally invasive method for identifying and pathologically staging regional lymph node basins, and it has been incorporated into the American Joint Committee on Cancer (AJCC) staging criteria of 20097. To date, many studies have been conducted in Western countries on the association between SLN status and survival in patients with MM8,9. However, there have been few reports on the benefit of SLNB in Asian populations, including the Korean population, given the low incidence of MM in these countries.
Melanoma sites and histological subtypes of MM differ between Korea and Western countries, so data on Caucasian populations cannot necessarily be applied to the Korean population. Accordingly, we conducted this study to evaluate the prognostic value of SLN status in Korean patients with ALM. To our knowledge, this is the first study to evaluate the prognostic value of SLN status on long-term survival in ALM patients undergoing SLNB in Korea.
We retrospectively reviewed all cases of primary cutaneous MM diagnosed pathologically at the Department of Dermatology in Dong-A University Hospital (Busan, Korea) from January 2000 to May 2012. Of these patients, 34 ALM patients who underwent SLNB were enrolled in this study. For the clinicoradiological evaluation of metastasis, laboratory and radiological tests were performed, including routine blood tests, tests for lactate dehydrogenase measurement, urinalysis, chest radiography, abdominal ultrasonography, chest and pelvic computed tomography (CT), bone scan, and positron emission tomography-CT. This study was approved by the institutional review board of Dong-A University Medical Center (IRB 12-032) and was performed in accordance with the Declaration of Helsinki.
Patients underwent lymphoscintigraphy approximately 2 to 6 hours before surgery in order to identify all the basins at risk and the SLN, as well as any possible interval nodes. A radioactive tracer (technetium-99m) was injected using an insulin syringe intradermally around the primary tumor at 4 points (Fig. 1A). Immediately after the injections, dynamic images of the corresponding lymphatic basins were obtained over 15 minutes using a gamma camera (MultiSPECT II; Siemens, Hoffmand Estates, IL, USA), which was followed by acquisition of a planar scan (10 minutes/image) or further dynamic scans until the SLN was visualized. A late planar scan of the draining lymph node basins was obtained after 2 to 3 hours. All possible lymph drainage regions were imaged (Fig. 1B).
External counting using a hand-held gamma-probe was performed to confirm the location of the SLN prior to surgery. Different anesthetic methods (local, spinal, or general) were employed depending on the type of surgery required (wide excision or amputation). After completing skin incision, surgical dissection guided by a hand-held gamma detection probe was performed to identify the hot node, which had much higher radioactivity than the surrounding lymph nodes. The hot node was regarded as the SLN (Fig. 1C).
Once the SLN had been identified, harvested, and measured again for radioactivity, the probe was used to search the harvested bed to ensure that there were no residual nodes with meaningful radioactivity (i.e., an SLN). After confirming no further meaningful radioactivity, primary layered closure was performed at the biopsy site. The identified SLN(s) were then confirmed again on the basis of meaningful radioactivity using the probe (Fig. 1D). H&E staining, staining for S-100, and staining for HMB-45 were then performed after formalin fixation to identify malignant cells and thus ascertain the presence of metastasis. Positive SLN specimens were histopathologically subclassified as having no metastasis, micrometastases (≤2 mm), or macrometastases (>2 mm).
This was a retrospective study, and all data were collected by reviewing medical records including clinical photographs, pathology slides, and medical charts. The clinical and demographic data included the patients' age, sex, the size and location of the tumor, clinical type, Breslow thickness, presence or absence of ulceration, clinical stage, histological stage, status of SLN, recurrence status, metastasis status, treatment modalities (for primary lesion, metastatic lesion, and recurrent lesion), OS, and disease-free survival (DFS). DFS was calculated from the date of SLNB to the date of death due to MM or recurrence or metastasis. Data on patients with no recurrence or on those who had not died were censored on 31 August 2012. Data on patients who died of other causes were censored at the time of death.
All statistical analyses were performed using IBM SPSS Statistics 19.0 (IBM Co., Armonk, NY, USA). For all patients (n=34), clinicopathological features were analyzed for association with SLN status using simple cross tabulations, Fisher's exact test, and the chi-squared test. The Kaplan-Meier method was used to evaluate DFS and OS, and survival curves were compared using the log-rank test. The associations of SLN metastasis and other clinicopathological factors with survival were also analyzed using the Cox proportional hazards regression model. The 95% confidence intervals for hazard ratios were calculated and reported for the univariate and multivariate statistical models. A p-value of less than 0.05 was regarded as statistically significant.
Table 1 shows the comprehensive clinical and pathological data. Twenty patients (58.8%) were men and 14 (41.2%) were women. The mean age of the patients was 57.7 years (range: 16~82 years). The mean Breslow thickness was 3.7 mm (range 0.9~9.0 mm). All melanomas were located on the hand (27%) or foot (73%). Ulceration was present in 50% of patients (n=17). The median follow-up duration was 60.5 months (range: 3~127 months). Local recurrence after surgery occurred in 8 patients (24%), and 11 patients (32%) showed distant metastasis (e.g., lung and brain metastases).
Of 34 patients, 14 (41.2%) had tumor cells in SLNs that were micrometastatic. The factors associated with positive SLNs are listed in Table 1. Positive SLNs significantly correlated with an increased local recurrence rate (43% vs. 10%, p=0.042) and pathological TNM stage (p<0.001). However, other factors did not correlate with SLN positivity (p>0.05).
In our study, the causes of death were closely associated with MM (local recurrence and distant metastasis). The Cox univariate and multivariate analyses of the prognostic factors (SLN status, sex, age, Breslow thickness, pathological T stage, pathological TNM stage, and ulceration) for OS and DFS are shown in Table 2 and 3, respectively. OS of the MM patients was associated with several factors in Cox univariate and multivariate analyses (Table 2), and SLN metastasis and Breslow thickness of the tumor significantly correlated with OS. Similarly, DFS was also associated with several prognostic factors in Cox univariate and multivariate analyses (Table 3), with SLN metastasis, sex, and Breslow thickness showing a significant correlation with DFS.
In the late 19th and early 20th centuries, Halsted10 introduced the 'tumor-node-blood' concept, hypothesizing that breast cancer cells metastasize from the primary tumor site via the lymphatics, after which systemic dissemination could occur via both the lymphatics and the bloodstream. In agreement with this concept, Snow11 suggested that melanomas first travel to a lymph node before disseminating systemically, and believed that early removal of the local lymph node basin might cure patients with no clinically palpable nodes. Accordingly, before the advent of SLNB, elective regional nodal dissection (ELND) was used to stage regional lymph nodes in patients with melanoma12,13. However, ELND is no longer performed for the following reasons. First, only 20% of patients with intermediate thickness melanomas (1.01~4.00 mm) have any nodal involvement, indicating that 80% of patients would undergo the procedure unnecessarily14. Second, postoperative complications including wound infections, seromas, hematomas, chronic lymphedema, and paresthesias can occur in a significant proportion of patients undergoing ELND15. Third, no prospective randomized trial has shown an OS benefit15. Compared to ELND, SLNB has been developed as a more prognostically accurate, less morbid approach to evaluating the lymphatic basin to which tumor cells may drain.
The SLN is known to be the first lymph node that drains a tumor. According to Morton et al.6,8, the SLN serves as an accurate marker for the involvement of the rest of the regional nodal basins. SLNB is based on the concept that lymphatic drainage from the primary tumor follows an orderly progression through afferent lymphatic vessels into the SLN(s) before flowing into the non-sentinel nodes in the regional lymphatic basin, rather than hematogenous spread of the tumor6,8,16. SLNB may be less complicated and invasive, and more accurate and effective in identifying occult nodal metastases in patients with melanoma, consequently providing better staging. Because of this, the technique has replaced ELND worldwide over the last few years.
Many studies have been conducted in Western countries on the association between metastasis to the SLN and patient outcome8,9, but to our knowledge, there has been a lack of research demonstrating the benefit of SLNB in Asian countries, including Korea. Melanoma sites and histological subtypes differ considerably between Korean and Western MM patients. In Western patients, superficial spreading melanoma is the most common subtype, and most melanomas are located on the trunk or lower limbs17, whereas the most common form in Korean patients is ALM on the hands and feet3. Although Breslow thickness is well known as a powerful predictor of patient outcome, Phan et al.18 reported that Breslow thickness was not found to be independently relevant to the prognosis of ALM (n=121). Therefore, the results of studies in Western countries cannot necessarily be applied to Korea, where striking differences are noted in histological subtype and primary tumor site.
In Japan, where a similar subtype of MM occurs in similar sites to those in Korea, Noro et al.19 analyzed a cohort of MM patients and reported that positive SLN status was a prognostic predictor of OS. The 5-year survival rate was significantly higher in patients with tumor-negative SLNs than in those with tumor-positive SLNs (p=0.0002). The association between positive SLN status and DFS was not analyzed. Another recent multicenter, large-scale study in Japan showed that SLN metastasis is a prognostic factor for both OS and DFS20. In accordance with these results, our study showed that patients with positive SLN status had a higher local recurrence rate (42.9% vs.10.0%, p=0.042) and tended to show a higher rate of distant metastasis (50.0% vs. 20.0%, p=0.135) than those with negative SLN status. In addition, patients with positive SLN status had higher hazard ratios for OS and DFS in Cox univariate and multivariate analyses (p<0.05) and shorter OS and DFS according to Kaplan-Meier survival curves than patients with negative SLN status. These results indicate that SLN status was a prognostic factor for OS and DFS in Korean patients with ALM.
This study also revealed that sex is a prognostic factor for DFS. A previous large-scale Western study showed that male patients have worse prognoses than female patients21, and consistent with these findings, our analysis demonstrated that male patients had poor prognoses compared to female patients in terms of DFS.
The current melanoma TNM classification system is predominantly an anatomic and pathological staging system, and Breslow thickness continues to be the main prognostic factor7. Furthermore, numerous studies have validated the clinical significance of Breslow thickness as an independent prognostic factor22,23. In agreement with previous studies, our study also suggested that Breslow thickness is an important prognostic factor for both OS and DFS in Korean patients with ALM.
Although previous Western studies have also reported that ulceration, pathological TNM stage, and pathological T stage are prognostic factors16,21, we did not find any relationship between patient outcome and other factors such as ulceration, pathological TNM stage, and pathological T stage in this study.
Our study was limited by being a single-center study with a limited number of patients. In addition, the incidence of melanoma is much lower in Korea than in Western countries, and there is a lack of systemic studies on ALM in Korea. Therefore, a multicenter study with a large sample size is required to confirm the results of our preliminary study.
In conclusion, to our knowledge, this is the first study on the long-term survival of patients undergoing SLNB for ALM in Korea. Our data showed that SLN-positive patients have worse OS and DFS than SLN-negative patients, which indicates that SLN status is an important prognostic factor for predicting OS and DFS in Korean ALM patients. SLNB, which is now recommended in the latest AJCC Cancer Staging Manual (7th edition), is a safe procedure with low short- and long-term morbidity and an acceptable low false-negative rate. Therefore, SLNB should be performed to predict the prognosis of Korean patients with ALM. Furthermore, SLNB may have important therapeutic implications, and advanced knowledge of the procedure could be useful to dermatologists in planning appropriate treatment for ALM patients in Korea.
Figures and Tables
Fig. 1
Lymphoscintigraphy-guided sentinel lymph node (SLN) biopsy. (A) Intradermal injection of radioactive tracer (technetium-99m) around the primary tumor. (B) The lymphoscintigram obtained from a patient with cutaneous melanoma on the right sole (primary tumor: red arrow, SLN: blue arrow). (C) Harvesting SLN(s) & measuring their radioactivity (SLN: black arrow). (D) Confirmation of the excised SLN(s) with significant high radioactivity.

Fig. 2
The Kaplan-Meier survival curves of patients with positive sentinel lymph nodes (SLNs) (solid line) and negative SLNs (dotted line). (A) Overall survival and (B) disease-free survival are shown.
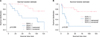
Table 1
Correlation of the SLN status with various clinicopathologic factors in 34 patients with cutaneous acral malignant melanoma

References
1. Johnson DS, Yamane S, Morita S, Yonehara C, Wong JH. Malignant melanoma in non-Caucasians: experience from Hawaii. Surg Clin North Am. 2003; 83:275–282.

2. Qiu D, Marugame T. Comparison of time trends in skin cancer incidence (1973-97) in East Asia, Europe and USA, from cancer incidence in five continents vol. IV-VIII. Jpn J Clin Oncol. 2008; 38:234–236.

3. Roh MR, Kim J, Chung KY. Treatment and outcomes of melanoma in acral location in Korean patients. Yonsei Med J. 2010; 51:562–568.

4. Wong SL, Balch CM, Hurley P, Agarwala SS, Akhurst TJ, Cochran A, et al. Society of Surgical Oncology. American Society of Clinical Oncology. Sentinel lymph node biopsy for melanoma: American Society of Clinical Oncology and Society of Surgical Oncology joint clinical practice guideline. J Clin Oncol. 2012; 30:2912–2918.

6. Morton DL, Wen DR, Wong JH, Economou JS, Cagle LA, Storm FK, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992; 127:392–399.

7. Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009; 27:6199–6206.

8. Morton DL, Thompson JF, Cochran AJ, Mozzillo N, Elashoff R, Essner R, et al. MSLT Group. Sentinel-node biopsy or nodal observation in melanoma. N Engl J Med. 2006; 355:1307–1317.

9. Debarbieux S, Duru G, Dalle S, Béatrix O, Balme B, Thomas L. Sentinel lymph node biopsy in melanoma: a micromorphometric study relating to prognosis and completion lymph node dissection. Br J Dermatol. 2007; 157:58–67.

10. Halsted WS. I. The results of radical operations for the cure of carcinoma of the breast. Ann Surg. 1907; 46:1–19.

11. Snow H. Abstract of a lecture on melanotic cancerous disease. Lancet. 1892; 140:872–874.
12. Breslow A. Tumor thickness, level of invasion and node dissection in stage I cutaneous melanoma. Ann Surg. 1975; 182:572–575.

13. Crowley NJ, Seigler HF. The role of elective lymph node dissection in the management of patients with thick cutaneous melanoma. Cancer. 1990; 66:2522–2527.

14. Beitsch P, Balch C. Operative morbidity and risk factor assessment in melanoma patients undergoing inguinal lymph node dissection. Am J Surg. 1992; 164:462–465.

15. Stebbins WG, Garibyan L, Sober AJ. Sentinel lymph node biopsy and melanoma: 2010 update part I. J Am Acad Dermatol. 2010; 62:723–734.
16. Medalie NS, Ackerman AB. Sentinel lymph node biopsy has no benefit for patients with primary cutaneous melanoma metastatic to a lymph node: an assertion based on comprehensive, critical analysis: part I. Am J Dermatopathol. 2003; 25:399–417.

17. Socrier Y, Lauwers-Cances V, Lamant L, Garrido I, Lauwers F, Lopez R, et al. Histological regression in primary melanoma: not a predictor of sentinel lymph node metastasis in a cohort of 397 patients. Br J Dermatol. 2010; 162:830–834.

18. Phan A, Touzet S, Dalle S, Ronger-Savlé S, Balme B, Thomas L. Acral lentiginous melanoma: histopathological prognostic features of 121 cases. Br J Dermatol. 2007; 157:311–318.

19. Noro S, Yamazaki N, Nakanishi Y, Yamamoto A, Sasajima Y, Kawana S. Clinicopathological significance of sentinel node biopsy in Japanese patients with cutaneous malignant melanoma. J Dermatol. 2011; 38:76–83.

20. Namikawa K, Yamazaki N, Nakai Y, Ihn H, Tomita Y, Uhara H, et al. Prediction of additional lymph node positivity and clinical outcome of micrometastases in sentinel lymph nodes in cutaneous melanoma: a multi-institutional study of 450 patients in Japan. J Dermatol. 2012; 39:130–137.

21. de Vries M, Speijers MJ, Bastiaannet E, Plukker JT, Brouwers AH, van Ginkel RJ, et al. Long-term follow-up reveals that ulceration and sentinel lymph node status are the strongest predictors for survival in patients with primary cutaneous melanoma. Eur J Surg Oncol. 2011; 37:681–687.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download